Fig. 24.1 Pityriasis rotunda. 63-year-old female with thyroid storm secondary to amiodarone, treated with thyroidectomy. There are circular thin plaques of scale on the back. Biopsy findings include epidermal changes (slight hyperkeratosis and focal hypogranulosis) and minimal inflammation. The lesions spontaneously resolved. A, Courtesy, Brittany Craiglow and Leon Luck.
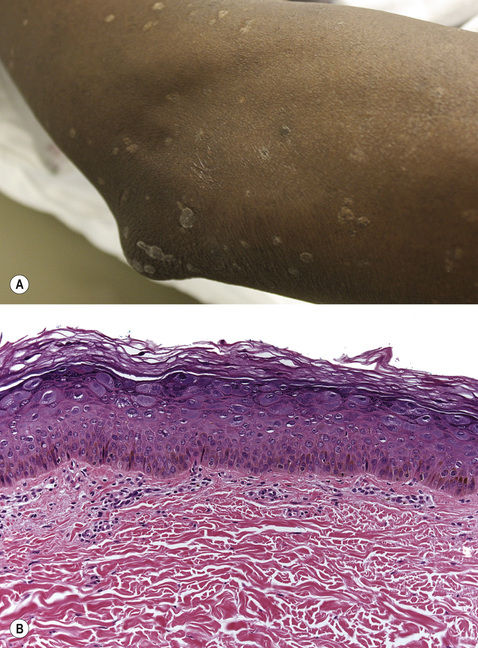
Fig. 24.2 Epidermodysplasia verruciformis. This HIV-negative male developed hypopigmented, flat-topped papules on the extremities in early adulthood. Clinically, the changes appear to be in the epidermis, and this corresponds to the biopsy findings of hyperkeratosis and altered cells (keratinocytes with expanded light pink–purple cytoplasm) in the granular layer. A,B, Courtesy, Yale Dermatology Residents’ Slide Collection.
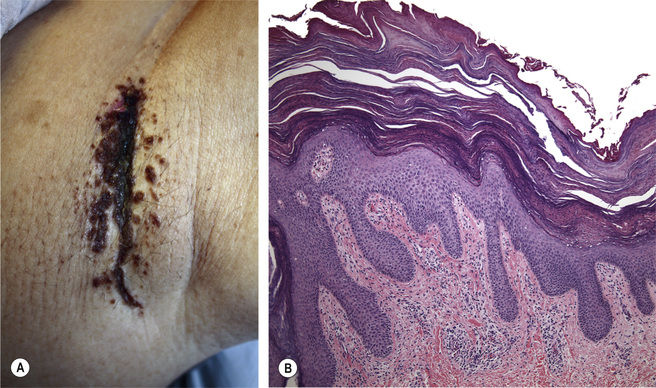
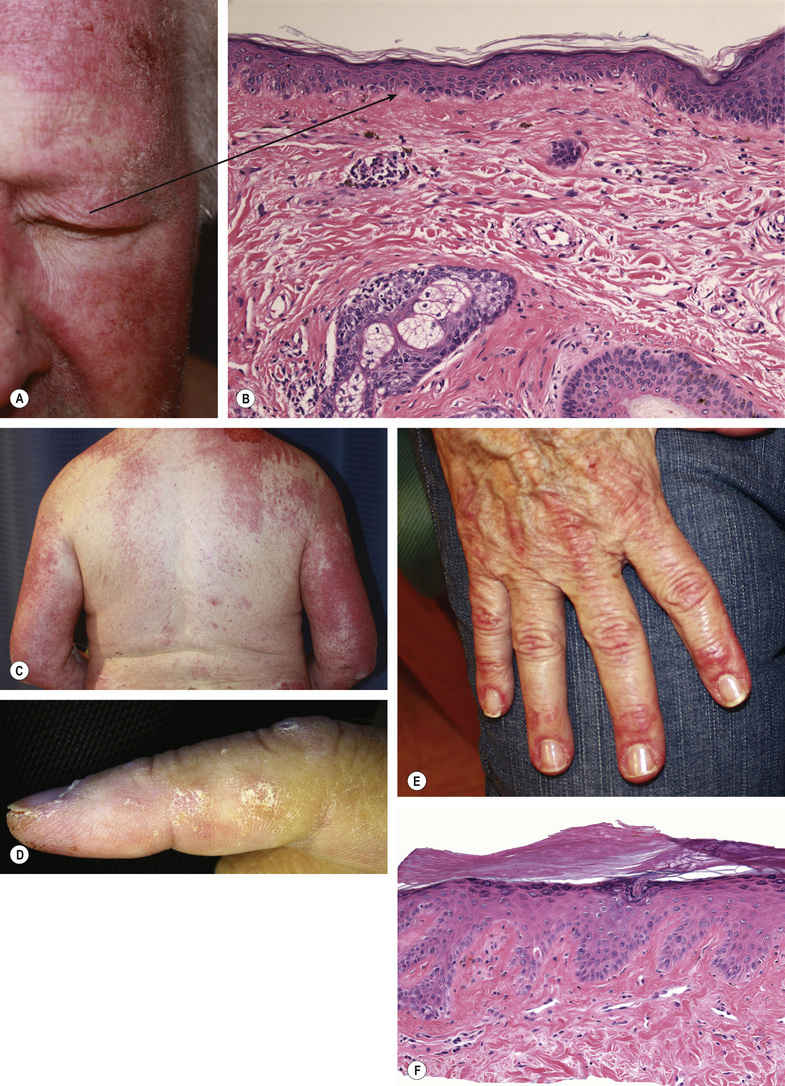
Fig. 24.4 A–F Dermatomyositis. Erythema, sometimes slightly scaly or eroded (particularly if the patient has pruritus). The erythema is pink to purplish in color and classically involves the eyelids (heliotrope rash) (A), the face, the chest and back (C), and the arms. Clues include nail fold telangiectasias (E) and jagged cuticles as well as erythema and flat-topped papules over the joints of the hands/knees/elbows. So-called “mechanic’s hands” may be evident, with scaling along the adjacent sides of the index finger and thumb (D). Histologic findings include subtle interface vacuolar change, often with minimal inflammation (B,F). A,C,D,E, Courtesy, Yale Dermatology Residents’ Slide Collection.
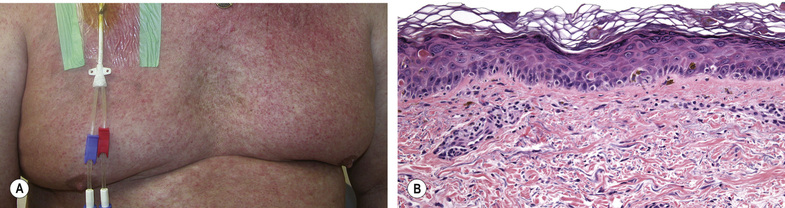
Fig. 24.5 Acute graft-versus-host disease. The clinical findings alone are non-specific and can closely simulate a maculopapular drug eruption. Clues include gastrointestinal symptoms/signs (i.e. diarrhea, liver function abnormalities). Classic histopathologic findings include interface vacuolar change with necrotic keratinocytes, sometimes extending into follicular epithelium. A, Courtesy, Yale Dermatology Residents’ Slide Collection.
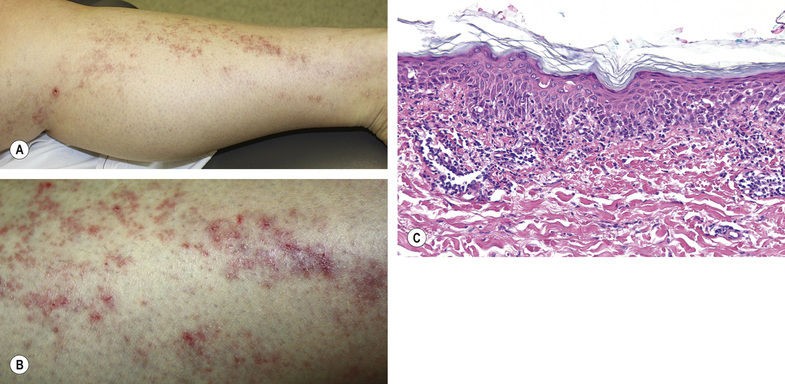
Fig. 24.6 Blaschkitis. In adulthood, this patient developed a linear streak of weeping papules and slightly violaceous patches on the leg. The lesion would wax and wane. Biopsy findings included lymphocytes at the junction of the epidermis and dermis, necrotic keratinocytes, and perivascular lymphocytes. Although histopathologic findings of Blaschkitis are typically spongiotic, interface patterns have been described. A,B, Courtesy, Yale Dermatology Residents’ Slide Collection; C, Courtesy Nemanja Rodic, MD.
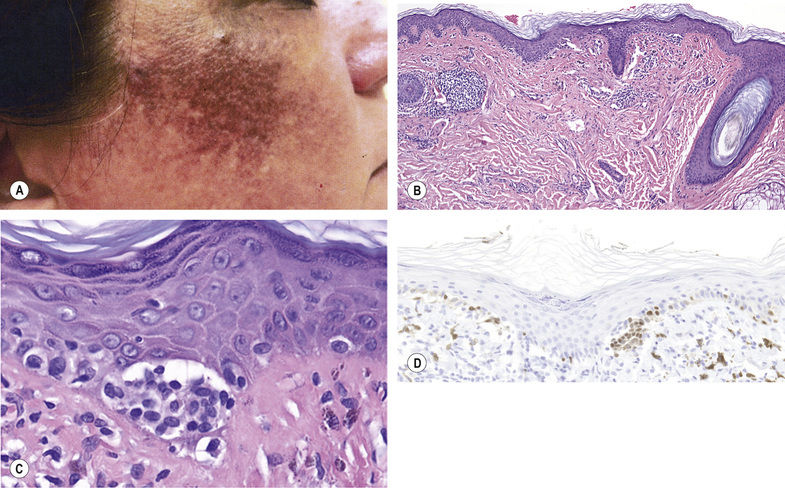
Fig. 24.7 Lichen planus pigmentosus. Bilaterally symmetric hyperpigmented patches on the cheeks (A). Biopsy findings alone have some resemblance to melanoma in situ (B), with small cells clustered in nests and arranged singly at the dermal–epidermal junction (C). Some of these cells are positive with MITF (D), but correlation with the clinical findings avoids misdiagnosis as a melanocytic process.
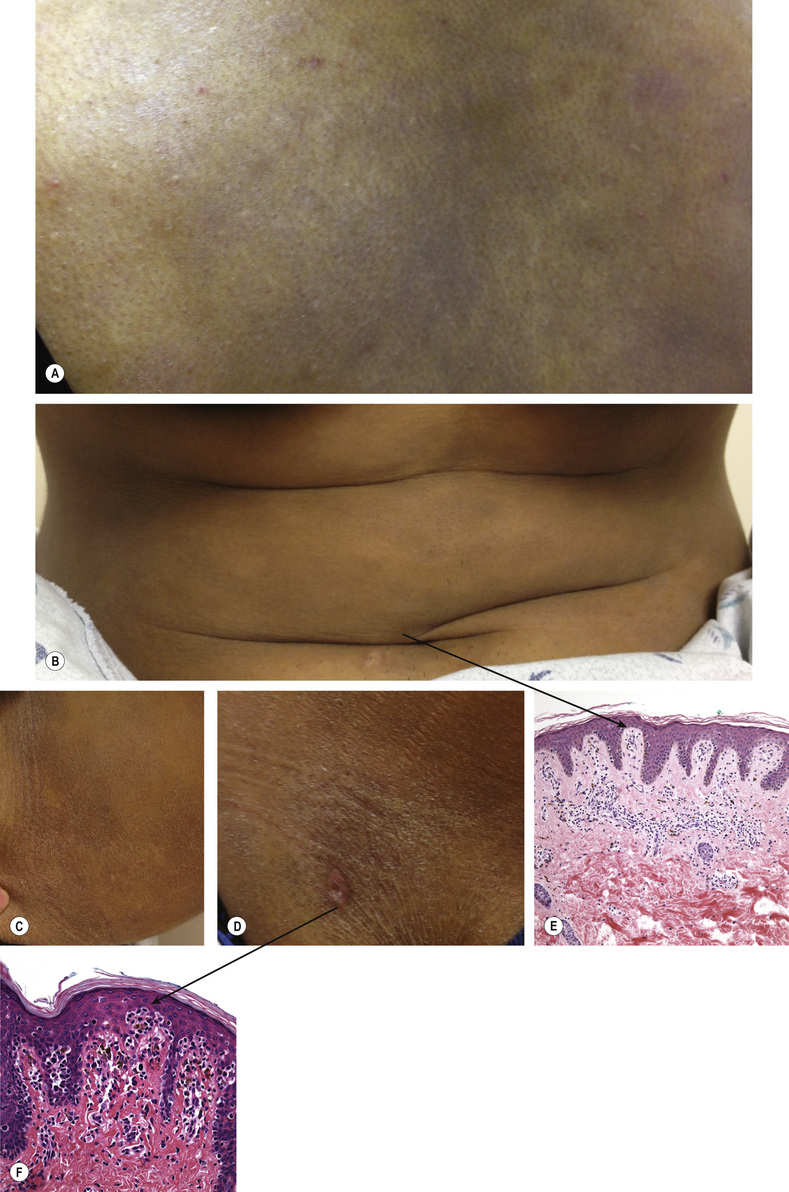
Fig. 24.8 A–F Hyperpigmented mycosis fungoides. 22-year-old female with asymptomatic to slightly pruritic ashy gray to brown macules and patches on her back (A) and abdomen (B), strongly resembling ashy dermatosis. Scattered on her inner arms (C), buttocks, and hips (D), she had slightly scaly lesions with focal atrophy. The biopsy site in (D) is light pink. The patient had multiple biopsies from different sites, all showing an epidermotropic, atypical lymphocytic infiltrate, more subtle in (E) than (F). She had clonal rearrangement of the T-cell receptor gene, with an identical clone found in 5 different sites. She was treated with ultraviolet light B phototherapy. E, Courtesy, Antonio Subtil, MD.
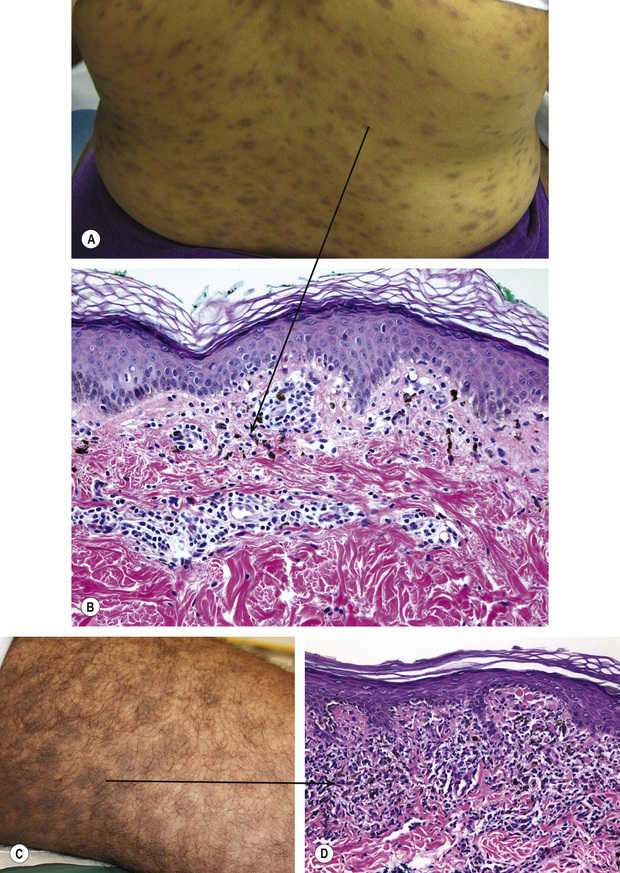
Fig. 24.9 Erythema dyschromicum perstans and lichen planus pigmentosus (inversus). Although erythema dyschromicum perstans (A,B) may have a thin pink border to the gray–brown oval lesions, as in this patient, such a border is more typically absent. The lesions often involve the trunk and upper arms and can be arranged in a distribution similar to pityriasis rosea. Lichen planus pigmentosus (C,D) is more brown in color, may involve intertriginous sites (so-called inversus, as in this patient with inner thigh lesions) and/or the face and neck, and may be associated with typical flat-topped, purplish lesions of lichen planus. Erythema dyschromicum perstans is typically less inflamed than lichen planus pigmentosus, with interface change and pigment incontinence (C). While lichen planus pigmentosus sometimes shows only pigment incontinence, this example shows lichenoid inflammation as well (D).

Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








