Escharotomy of the hand is performed by incising the eschar in the intermetacarpal spaces. Care is taken not to unnecessarily sever or expose underlying extensor tendons
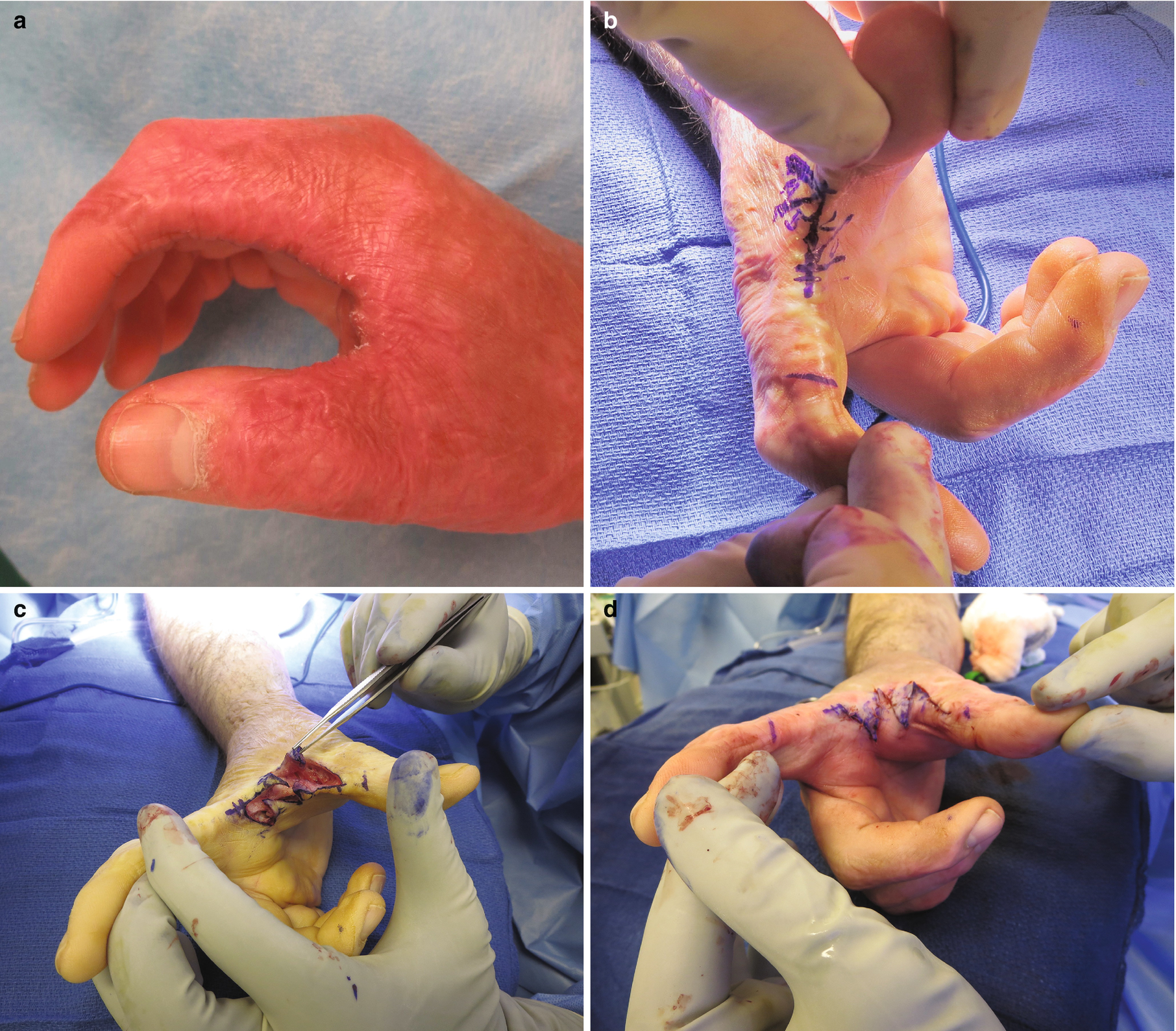
Patients with circumferential forearm burns are at risk for compartment syndrome when edema collects deep to the unyielding eschar resulting in decreased arterial flow and venous congestion. If escharotomy is not performed as described above, ischemic tissues (i.e., skeletal muscle) will become edematous leading to compartment syndrome and permanent muscle death. Electrical injuries and burns with an associated crush injury are more likely to increase compartmental pressures, resulting in compartment syndrome due to muscle injury. Deep muscle compartments are often more injured than superficial after electrical burns due to bone’s elevated resistance to current flow. Neuropraxia following electrical shock can also complicate the initial assessment. The diagnosis of compartment syndrome is generally clinical and heralded by the constellation of pain on passive stretch, paresthesias, pallor, paralysis, decreased pulses, and poikilothermia. Systemic signs, including myoglobin-induced metabolic acidosis, may be the only sign of compartment syndrome in an obtunded patient with myonecrosis. Compartmental pressures of >30 mmHg or within 10–20 mmHg of diastolic pressure are diagnostic of compartment syndrome [5]. In the setting of suspected compartment syndrome, or failure of escharotomy to restore distal perfusion, fasciotomy should be performed in the operating theater. Forearm incisions include a dorsally and volarly oriented release that targets all three compartments of the forearm (anterior, posterior, and mobile wad). Additionally, if compartment syndrome of the hand is suspected, a full release of all ten compartments and both peripheral nerve canals (carpal tunnel and Guyon’s canal) should be performed [3, 6]. The compartment release is commonly achieved through four incisions: ulnar hand (hypothenar), thenar eminence, dorsal index finger metacarpal (interossei and adductor pollicis), and dorsal ring finger metacarpal (interossei). The carpal tunnel and Guyon’s canal are released in a standard fashion.
36.5 Surgical Management
36.5.1 Early Excision and Grafting
Early excision and grafting have been shown to reduce hypertrophic scarring and subsequent contractures leading to a reduced need for later reconstructions [7–10]. Superficial and intermediate partial-thickness burns will often heal within 2 weeks and rarely require early excision. However, deeper wounds that are expected to take longer to heal (i.e., longer than 21 days) should be carefully monitored for healing potential. Burns should be excised and grafted once they demonstrate inability to heal. Given the relatively small surface area of the hand, timing of hand excision in a patient with extensive burns should be weighed against the need to remove large areas of eschar to prevent burn wound sepsis.

The Versajet water dissector provides precise tissue excision and is particularly well suited for areas of convexity and concavity
The majority of hand burns can be covered with split thickness skin grafts. In order to guide graft harvest, the wound bed should be templated and transposed to the planned donor site. The anterolateral thigh is a sufficient donor site for majority of patients. A dermatome with the widest guard appropriate for the amount of skin needed helps to minimize the number of graft junctions. For the majority of excised dorsal wounds, 0.012 inch thick grafts are sufficient while 0.015–0.018 inch thick grafts are necessary for the palm. Sheet grafts are preferred to mesh grafts in order to provide better functional and cosmetic results [16–18]. Full-thickness grafts harvested from the inguinal crease or the flank may be the most appropriate choice for small burns on both the dorsum and the palm. Grafts are affixed with absorbable sutures and fibrin glue in the wound bed. The edges of the graft are reinforced using with Hypafix (Smith and Nephew, London, UK) and Mastisol (Ferndale Laboratories, Ferndale, MI). A dressing of nonadherent material, fine-mesh gauze, Kerlix rolls, and a custom fabricated splint is applied. Of note, grafting should take place in the same position as splinting, attempting to maintain tension on the collateral ligaments (i.e., flexed metacarpophalangeal and extended interphalangeal) and abduct the first web space. The dressing is removed on post-operative day 1, and fluid collections are evacuated with a small incision in the graft. It is important to note that we do not make any pie-crusting incisions in the graft at the time of placement but only over areas where fluid accumulates. The wound should be inspected daily until no fluid collections are noted. The dressing is then maintained until post-operative day 5 and then replaced with a lighter nonadherent dressing to allow for range of motion exercises [16]. Negative pressure therapy is an alternative postoperative dressing that provides bolstering and transudate evacuation with promising results compared to traditional methods [19]. The donor site, if properly harvested and dressed, should re-epithelialize spontaneously within 2 weeks. We prefer Mepilex Ag (Molnycke) a silver-impregnated dressing or absorbent Tegadem, although a nonadherent gauze and bacitracin are also acceptable.
36.5.2 Pediatric Hand Burns
The pediatric palm burn may be an exception to aggressive early excision. Palm burns are frequently encountered in the infant and toddler population after contacting a hot surface (e.g., stove, fireplace, or heater). These burns are usually deep partial-thickness injuries and, therefore, may heal without surgery; however, controversy remains over the timing of excision and choice of graft for indeterminate and deeper burns. While there are advocates for early excision and full-thickness grafting to prevent infection and limit future contractures [20], in the author’s experience [21], a more conservative approach is warranted. There is no evidence to suggest that delay of the excision until week 2 or 3 prevents infection, and if the wound can heal within 3 weeks of time, avoiding excision may help to protect palmar sensation that is vital to overall hand function [22]. If excision is warranted, both split and full-thickness grafts are acceptable approaches to wound coverage. Typically, if the area of burn can be covered with a single full-thickness graft (i.e., harvested from a single site), then this will be performed; in other cases, a thick split thickness graft is used to minimize the need for multiple grafts with junctions on the palm. In the case of secondary reconstruction, full-thickness grafts are the preferred coverage following release.
Perhaps more important than the decision for surgery timing and choice of coverage is the need for aggressive hand range of motion therapy and splinting overnight. It is critical that children with palm burns undergo aggressive range of motion therapy immediately. Parents must be instructed on how to adequately range the hand and should do so at least 8–10 times daily. Splints should only be used at night or if early signs of contracture are noted.
36.5.3 Tissue Flaps
Severe burns , especially on the dorsum of the hand where the skin is thin with little underlying subcutaneous tissue, are often not amenable to skin grafting due to exposed bone or tendon and may require flap coverage. Digits sometimes require vascular soft tissue coverage to optimize function. Numerous soft tissue flaps have been described to provide durable coverage for areas for which skin grafting would not be appropriate, and the most common coverage options are described below. It is important to keep in mind injuries to deeper hand structures may also require management prior to wound coverage. For example, in cases where the extensor tendon and joint are burned, one should consider early joint arthrodesis to stabilize joint positioning and allow for faster functional recovery.
Local flaps. The radial forearm fasciocutaneous or fascial flap, based on the radial artery, is an appropriate choice for local coverage when the donor site remains uninjured. An Allen’s test, as well as Doppler examination of the superficial palmar arch, should be performed prior to raising the flap to ensure adequate ulnar perfusion of the hand. Skin grafting of the donor site in the case of a fasciocutaneous flap or recipient site in the case of a fascial flap will be necessary. The distally based posterior interosseus artery flap is a fasciocutaneous flap harvested from the dorsal aspect of the forearm and does not disrupt either of the major blood vessels perfusing the hand [23]. Although the flap’s perfusing vessel is sometimes hypoplastic or absent, this flap is especially useful when there has been an injury to either the radial or ulnar artery.

A pedicled abdominal flap was used to provide soft tissue coverage over exposed joints and tendons of the hand. In this case two separate flaps were used—one for the thumb and one for digits
Free tissue transfer. Free tissue transfer is necessary when extensive burns preclude local or distant pedicled flaps. Numerous options exist and can be carefully selected following the principle of “replace like with like” [24]. For the dorsum of the hand, this calls for thinner tissue including fascial and fasciocutaneous flaps such as the contralateral radial forearm flap, temporoparietal fascial flap, lateral forearm flap, serratus fascial flap, dorsal thoracic fascial flap, and dorsalis pedis flap. For the palmar surface, the glabrous skin is more challenging to replace. The above flaps may all be considered with the addition of perforator flaps in a thin patient such as the anterolateral thigh (ALT) flap. Innervated palmar skin is essential for hand function; thus, sensate flaps should be considered first. Prior to considering a free tissue transfer, the viability of the recipient vessels must be evaluated to ensure that they have also not been damaged. In severe injuries where there is loss of all digits or the entire hand, muscle flaps can be utilized to provide wound closure and provide a foundation for subsequent reconstruction or prosthetic devices [14, 25].
36.5.4 Skin Substitutes
A full discussion of skin graft substitutes is beyond the scope of this chapter; however, products curtailed to the hand are important to note. Skin substitutes may be useful in cases of extensive burn injury where there is limited donor site for harvesting quality autografts. Skin substitutes are applied to the freshly excised wound bed, and just as in the case of autograft placement, it is essential that the wound bed is viable and hemostatic prior to placement. Broadly, substitutes are viewed in two categories: temporizing bridges to autografting and dermal regenerative matrices that are used in combination with autologous skin grafts. Multiple products exist in both categories with varying success [26]. Bridging coverage includes cadaveric human skin (allograft) and porcine skin (xenograft), which all must be removed prior to definitive autografting. These options are often utilized to test the viability of wound beds in addition to temporary coverage [15].
Dermal regenerative matrices are used in viable full-thickness wounds to promote the formation of dermis through ingrowth of scaffolds. For dorsal hand burns, these products provide bulk and coverage where skin grafts might otherwise not take or suffer significant contour deformities. Integra (Integra Life Sciences, Plainsboro, NJ) is shark- and bovine-derived acellular collagen matrix with a silicon pseudo-epidermis. The product is used in a two-stage manner, whereby initial placement on a vascular wound bed is followed by a 3-week delay to allow ingrowth and autografting (with removal of silicon sheet). This is an excellent option for dorsal defects where serial Integra stacking allows for tissue bulking prior to autografting. A similar product, Matriderm (Dr. Otto Suwelack Skin & Health Care AG, Billerbeck, Germany) is a single-stage bovine collagen matrix. Like Integra, it is placed in a viable full-thickness defect, but instead of staged autografting, a think skin graft is placed over the Matriderm at the time of initial surgery. Proponents of Matriderm cite its improved pliability over other products [27]. Though acellular dermal matrix is often used in bridging, others have described its success in definitive reconstruction when used with thin autografts [28].
36.5.5 Amputation
Severe burns of the hand may result in injuries for which salvage is either impossible or impractical. The ultimate goal of treatment of hand burns is optimizing function. The loss of a digit often provides the patient with a more favorable outcome when compared to an insensate, painful, and stiff digit. Delayed amputation may be required when all other treatment options have been exhausted or failed. Length should be preserved at all times. As is the case with all severe hand burns, realistic discussions about the goals of reconstruction should take place prior to embarking on a plan of treatment. In addition, an area of viable soft tissue on a digit that is to be amputated may be useful for coverage the hand elsewhere. For example, if the dorsal aspect of a digit is burned down through the tendon and joint, a filet flap from the volar aspect of the digit can be used to cover any exposed MP joints or tendons.
36.6 Postoperative Care and Long-Term Management

Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








