Where does the nipple–areolar complex (NAC) get its innervation from?
Predominately from the lateral cutaneous branches of the fourth intercostal sensory nerve. These fibers course deep within the pectoralis fascia before rising to innervate the NAC from its posterior surface in 93% of cadaveric specimens.
 What is the sensory innervation to other areas of the breast?
What is the sensory innervation to other areas of the breast?
The upper pole is innervated by the supraclavicular nerves, which come from the third and fourth branches of the cervical plexus. The medial and lateral breast is innervated by the anterior and lateral cutaneous branches of intercostals nerves II to VII.
 What is the dominant vessel in the arterial supply to the breast?
What is the dominant vessel in the arterial supply to the breast?
The major blood supply comes from the internal mammary artery (IMA) perforators (estimated 60% total), with significant collaterals from the lateral thoracic artery, the thoracoacromial trunk, the thoracodorsal artery, as well as numerous intercostal perforators from interspaces 3 to 5.
 What are some relative preoperative indications that a free-nipple graft may be required during reduction mammoplasty?
What are some relative preoperative indications that a free-nipple graft may be required during reduction mammoplasty?
• Nipple transpositions >25 cm
• Smokers
• Patients with diabetes
 What determines the cup size of a bra?
What determines the cup size of a bra?
Cup size is a common reference point when patients describe their goals for breast reduction and describes the relationship of breast girth to chest girth. If breast girth exceeds chest girth by 1 in, the cup size is an A; 2 in is a B; 3 in is a C, 4 in is a D, and 5 in is a DD.
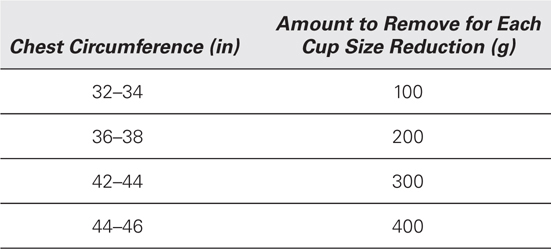
 What is Regnault’s correlation between chest girth and the amount of glandular resection required to approximate bra cup size?
What is Regnault’s correlation between chest girth and the amount of glandular resection required to approximate bra cup size?
 What is the management of the dusky postoperative NAC?
What is the management of the dusky postoperative NAC?
1. Release the sutures holding the NAC to make sure there is no tension-related problem.
2. If no brisk change in appearance, the flap should be opened in the operating room to check for pedicle-kinking or hematoma that could explain the ischemia.
3. Application of nitroglycerin paste to the NAC for a vasodilation effect should be considered.
4. If these maneuvers are ineffective, a free-nipple graft should be performed on a deepithelialized bed.
5. There are several case reports of salvage of ischemic NACs with hyperbaric oxygen.
 Why does a free-nipple graft survive when an NAC on a dermal-glandular pedicle will not?
Why does a free-nipple graft survive when an NAC on a dermal-glandular pedicle will not?
The metabolic demands of the NAC as a skin graft are less.
 What is the aesthetic appearance of a free-nipple graft?
What is the aesthetic appearance of a free-nipple graft?
There is always some degree of hypopigmentation that may require tattooing, especially in dark-skinned patients. Excision of the hypopigmented portions is also an option. Following a free-nipple graft the nipple lacks projection.
 In the rare cases requiring a repeat reduction mammoplasty, what should be done when the previous pedicle type is unknown?
In the rare cases requiring a repeat reduction mammoplasty, what should be done when the previous pedicle type is unknown?
Strong consideration should be given to a planned free-nipple graft. If you do know the previous pedicle design, the same pedicle should ideally be used to minimize the risk of devascularizing either the NAC or the pedicle itself.
Studies have shown that repeat reduction can be done safely without knowledge of the previous pedicle and without resorting to a free-nipple graft.
 Is a deepithelialized dermal pedicle required to maintain NAC viability?
Is a deepithelialized dermal pedicle required to maintain NAC viability?
No, although it theoretically provides a greater margin for error. The NAC can clearly survive on a well-designed glandular pedicle alone in favorable patients.
 What is the advantage of a closed (vs. open) design with a Wise inverted-T pattern-type flap design?
What is the advantage of a closed (vs. open) design with a Wise inverted-T pattern-type flap design?
A closed design, one in which the NAC opening is not initially precut in the incision, allows much greater flexibility for placing the nipple at the proper projecting part of the breast as well as allowing adjustments for symmetry with the contralateral breast.
 What is the key difference between the classic Strömbeck and McKissock techniques?
What is the key difference between the classic Strömbeck and McKissock techniques?
Both are inverted T-style designs with bipedicled dermoglandular flaps. They differ in the pedicle orientation with the Strömbeck oriented horizontally, while the McKissock “bucket handle” is folded on itself and oriented vertically.
 What are the odds of finding an occult breast cancer in a breast reduction specimen?
What are the odds of finding an occult breast cancer in a breast reduction specimen?
Retrospectively, this has been estimated between 0.16% and 0.4% in several recent studies.
 What is the effect of reduction mammoplasty on breast cancer risk?
What is the effect of reduction mammoplasty on breast cancer risk?
In peri- and postmenopausal women (age 40+), there was consistent reduction in relative risk for developing breast cancer of between 50% and 70%.
 What is the reduction in breast cancer risk after prophylactic mastectomy?
What is the reduction in breast cancer risk after prophylactic mastectomy?
The reduction in risk for developing breast cancer is 90% for bilateral prophylactic mastectomy. A unilateral prophylactic mastectomy after developing breast cancer in the contralateral breast approaches a 95% risk reduction.
 Where is the most common place for keloid scarring to occur with breast reductions?
Where is the most common place for keloid scarring to occur with breast reductions?
At the medial edge of the transverse incision.
 What are the recommendations for mammograms postreduction?
What are the recommendations for mammograms postreduction?
A postreduction mammogram 6 months after reduction should be performed to establish a new baseline image for future comparison.
 What is the result of overly long inframammary fold (IMF)-NAC vertical limbs with Wise-pattern inferior pedicle procedures?
What is the result of overly long inframammary fold (IMF)-NAC vertical limbs with Wise-pattern inferior pedicle procedures?
As the length of the vertical limb increases much beyond 5 cm, premature bottoming-out of the tissue has been frequently observed.
 Who are the best candidates for good results with suction-assisted lipectomy (SAL) breast reductions?
Who are the best candidates for good results with suction-assisted lipectomy (SAL) breast reductions?
The best candidates are breasts with little to no ptosis and a higher-fatty composition. Generally, older women with smaller breasts.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


