Fig. 41.1
Decision algorithm
41.3 Complications Associated with PMRT
The aim of PMBR is to restore physical form and decrease the psychosocial distress associated with not having a breast. In the setting of PMRT, both prosthetic and autologous tissue reconstruction are associated with complications that can hinder these outcomes. Although some groups have found that patient satisfaction is high irrespective of complications [13], others suggest that postoperative complications contribute significantly to patient dissatisfaction following PMBR [14]. Patients contemplating PMBR in the setting of expected adjuvant radiotherapy need to be informed of the possible postradiotherapy complications associated with both types of reconstruction.
Delayed expander/implant reconstruction of a previously irradiated mastectomy defect is associated with a poor cosmetic outcome owing to contraction of the chest wall soft tissues and internal scarring (Fig. 41.2) [7]. These radiation-induced pathological processes can inhibit tissue expansion and prevent the formation of an aesthetic prosthetic breast mound with adequate ptosis [7]. As a result, some believe that immediate expander/implant breast reconstruction followed by PMRT is preferable over delayed reconstruction. Delivery of PMRT in the setting of IBR can occur either before or after exchange for a permanent implant. Regardless of the timing of delivery, PMRT has been shown to result in increased complication rates [15]. Possible complications include a poor aesthetic outcome due to dense scar formation, capsular contraction, and expander/implant extrusion (Fig. 41.3) [15]. Furthermore, in a recent study from the National Italian Cancer Center in Milan where complication rates were compared between a group of patients in whom PMRT was delivered to their permanent prosthesis (n = 109) and a group in whom PMRT was delivered to their tissue expanders (n = 50), it was found that the latter group had significantly higher rates of reconstructive failure (40 vs. 6.4 %) [10].

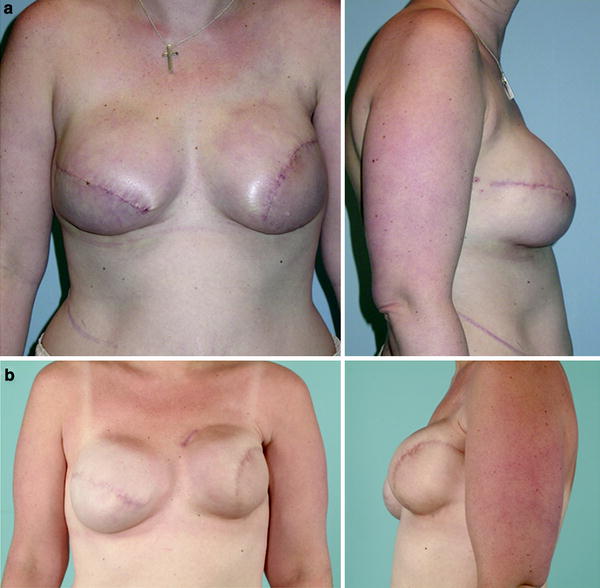

Fig. 41.2
Previous right mastectomy followed by radiotherapy
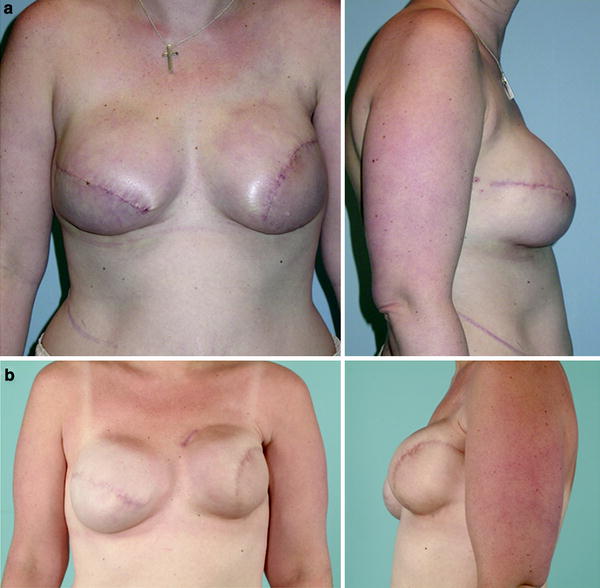
Fig. 41.3
Increased left breast capsular contracture formation following radiotherapy to the prosthetic breast mound. a Early postoperative result after completion of bilateral tissue expander/implant reconstruction. b One year after completion of radiotherapy of the left breast. Note the formation of a grade 3 capsular contracture at 1 year
Similar to prosthetic reconstruction, exposure of an autologous tissue breast reconstruction to PMRT is also associated with complications that can compromise the final aesthetic outcome. These include fat necrosis, parenchymal fibrosis, tissue envelope retraction, and hypertrophic scarring of the reconstructed breast [16]. In a study that compared IBR followed by PMRT versus PMRT followed by DBR, it was found that parenchymal changes such as fat necrosis and fibrosis were significantly higher in the group that received IBR followed by PMRT [11, 16]. This group also had higher revision rates compared with patients who underwent delayed reconstruction to replace their radiation-damaged tissues [11, 16]. Therefore, in general, most authors prefer to perform delayed autologous reconstruction in the setting of expected PMRT (Fig. 41.4) [6, 17].


Fig. 41.4
Preoperative and postoperative results after delayed right breast reconstruction using a free deep inferior epigastric perforator flap to correct a previously irradiated mastectomy defect
41.4 Prosthetic Breast Reconstruction in Patients Requiring PMRT
Prosthetic reconstruction is indicated in patients who are ineligible for autologous tissue breast reconstruction and may be preferred because it preserves tissue sensation, has a quicker postoperative recovery, and is not associated with a donor site defect. For those patients who exclusively desire prosthetic reconstruction and are known to require PMRT, the only viable solution may be to perform expander/implant reconstruction at the same time as the mastectomy. If the opportunity for IBR with an expander/implant is lost before PMRT occurs, then the option to reconstruct a delayed irradiated mastectomy defect will necessitate the use of autologous tissue.
Immediate prosthetic reconstruction in the setting of expected PMRT is feasible using the MSKCC protocol (Fig. 41.5). The MSKCC protocol is a staged approach that takes advantage of the time during adjuvant chemotherapy to fully inflate the tissue expander, and the time between the completion of adjuvant chemotherapy and start of radiotherapy to perform the permanent implant exchange. More specifically, at the time of the mastectomy and/or axillary lymph node dissection, a total submuscular tissue expander is placed. Approximately 2 weeks following placement, tissue expansion begins and continues during the 5 months of adjuvant chemotherapy [18]. Exchange of the tissue expander for a permanent implant occurs on average 4 weeks following the completion of chemotherapy [18]. Radiotherapy is started about 4 weeks after exchange, leaving time for the wound to heal [18]. Using this approach, McCormick et al. [18] demonstrated its oncologic safety with a 5-year locoregional control of 100 % and distant disease-free survival of 90 % in a series of 104 patients. In addition to increased survival, this approach resulted in good to excellent aesthetic results in 80 % of patients, and 72 % of patients stated that they would choose this treatment option again [19].
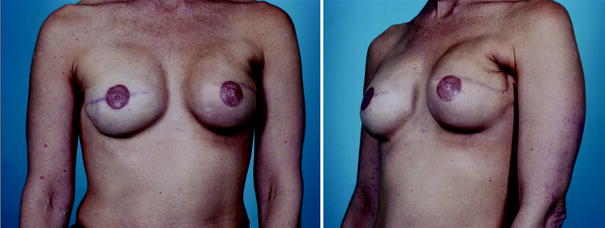
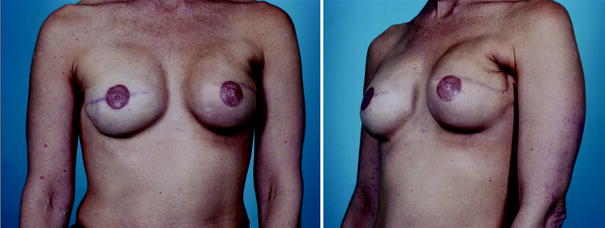
Fig. 41.5
Bilateral expander/implant reconstruction 2 years postoperatively with postexchange postmastectomy radiotherapy for the left breast (Memorial Sloan-Kettering Cancer Center algorithm). Note the grade 2 capsular contracture of the irradiated breast, with a still aesthetically pleasing result
A new ancillary tool to prosthetic reconstruction is the use of acellular dermal matrix to provide inferolateral coverage of the expander/implant where the pectoralis major muscle is deficient (Fig. 41.6) [20]. Purported advantages of acellular dermal matrix include the ability to bypass multiple tissue expansion processes by performing a one-stage implant reconstruction, improved postradiotherapy wound healing owing to its capacity to recellularize and revascularize tissue, decreased pain from eliminating the need to elevate the serratus anterior muscle, increased intraoperative tissue expansion volume, and improved aesthetics and ptosis [3, 20, 21]. However, the biological behavior of this dermal substitute in response to radiotherapy remains to be further elucidated [21]. Although several animal studies have shown that radiotherapy has no significant adverse effects on dermal matrix [22, 23], the small sample sizes and lack of long-term follow-up in current human studies preclude the formation of definitive conclusions [20, 24].


Fig. 41.6
Preoperative and postoperative results after left skin-sparing mastectomy and immediate one-stage acellular-dermal-matrix-assisted implant reconstruction. a Preoperative anterior and oblique views prior to skin-sparing mastectomy and reconstruction. b Postoperative photograph following left skin-sparing mastectomy and immediate one-stage acellular-dermal-matrix-assisted implant reconstruction and nipple/areolar reconstruction
41.5 Autologous Tissue Breast Reconstruction in Patients Requiring PMRT
The effects of PMRT on IBR with autologous tissue remain controversial. From an oncologic perspective, it has been suggested that the effectiveness of delivery of radiotherapy to the chest wall may be impaired by the presence of an intervening autologous tissue breast mound [25]. From an aesthetic perspective, advantages of IBR over DBR include preservation of the inframammary fold and pliability of the native breast skin to allow a more natural appearance [17]. However, these advantages may be lost when the autologous tissue mound is subjected to PMRT owing to volume loss and tissue contraction [11]. To further confound this issue, there is conflicting evidence as to whether there is improvement in quality of life and more psychological benefit to the patient in the immediate versus the delayed reconstruction setting [13].
In the setting of expected PMRT, we prefer to perform delayed autologous tissue breast reconstruction to avoid the deleterious effects of radiation on the newly created breast mound (Fig. 41.4) [6, 17]. This is the safer option since delayed autologous reconstruction of a previously irradiated mastectomy defect generally has fewer long-term complications than irradiating an autologous mound created during IBR. The optimal time between the completion of PMRT and reconstruction is controversial; however, a minimum of 6 months is generally recommended for sufficient healing of the radiation-damaged tissue [26]. Planning for delayed reconstruction of an irradiated mastectomy defect requires an understanding of how soft tissues respond to radiotherapy and an estimate of the amount of skin that needs to be replaced. Our preferred choices of autologous tissue flaps to be used in delayed reconstruction include the pedicled or free transverse rectus abdominis myocutaneous flap, the muscle-sparing transverse rectus abdominis myocutaneous flap, and the free deep inferior epigastric perforator flap. Three technical pearls in the delayed reconstruction of an irradiated mastectomy defect include excision of the previous mastectomy scar, lengthening of the superior mastectomy flap using a relaxing “dart,” and replacement of the entire lower mastectomy flap, which is generally scarred and noncompliant, with the healthy and pliable abdominal skin flap [3, 17]. With proper planning and execution, reconstruction of the breast mound with autologous tissue can result in excellent ptosis and shape, with the recreation of the inframammary fold.
In a patient who has either insufficient abdominal tissue or surgical scars that preclude the use of an abdominal skin flap, reconstruction using a latissimus dorsi myocutaneous flap in combination with an expander/implant is our second preferred method of DBR (Fig. 41.7). The adjunctive use of a latissimus dorsi flap can improve breast contour and offer protection against the adverse effects of radiation [27]. It is a well-vascularized flap that can be used to envelope the prosthesis to provide three unique advantages in an otherwise hostile irradiated milieu. First, the latissimus dorsi flap provides an extra layer of protection to lower the risk of implant extrusion; second, it likely contributes to better perfusion and healing of the overlying irradiated mastectomy skin; and lastly, it is thought to decrease the formation of capsular contracture around the prosthesis [27].










