Amastia (see 3.1.1)
3.1.1 Hypoplastic Breast
-
Athelia: isolated absence of the NAC
-
Amasia: absence of breast parenchyma
-
Amastia: absence of both the breast tissue and the NAC
-
Micromastia: postpubertal underdevelopment of breast tissue (hypoplasia)
History
History of injury/surgery to breast and ovaries, delayed puberty, chronic disease/endocrinology. Ask about primary amenorrhea and secondary sexual characteristics. Family history of delayed development (constitutional) or family history of similar diagnosis. Psychological distress for school age, and the family should be addressed. These diagnoses are usually diagnosed by examination. Athelia is discovered during childhood. Amasia, amastia, and micromastia are usually discovered later during pubertal growth. If 6 months passes after the age of 17 with no changes to the size, the diagnosis is confirmed.
Examination
Whole body exam for puberty characteristics, specifically tanner stage. Inspect and palpate, measure the breast size and width. Compare both sides (if less than 2/5 of the contralateral breast, then the breast is called hypoplastic). Body length and weight and growth percentile should be assessed. Photograph should be taken, and a bone age is ordered. Rule out Poland’s syndrome and endocrine causes—e.g. adrenal hyperplasia, turner syndrome, and testicular feminization disorders (which are usually bilateral).
Treatment
Breast augmentation after clinically confirming end of pubertal growth. NAC reconstruction is done to treat athelia.
3.1.2 Poland’s Syndrome

History
A rare congenital disorder that is characterized by hypoplasia of the pectoralis muscles and ipsilateral webbing of the fingers. It can include other deformities such as scoliosis, hypoplasia of the rib cage and lungs, upper extremity hypoplasia, breast and nipple hypoplasia, and deficiency in the skin layers and content. Other muscles in the shoulder can also be affected.
Exam
Upper limbs and chest should be examined thoroughly to identify the structures involved in the disorder. X-rays should be taken for the whole upper limb including both hands.
Treatment
Is focused on replacing or reconstructing the deficiency involved in the disorder. In regard to the breast, autogenous or alloplastic material can be used to replace breast tissues. Nipple-areolar complex (NAC) reconstruction is usually needed in cases where the NAC is involved.
The hand treatment is tailored to the extent of the deformity. Syndactyly release is the commonest operation needed for these patients.
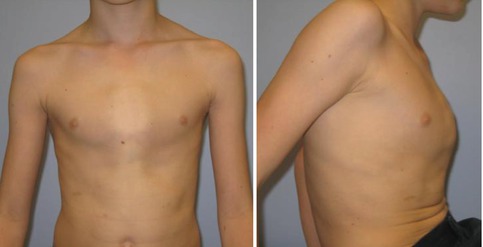
3.1.3 Pectus Excavatum

History
Congenital chest wall deformity in which several ribs and the sternum grow abnormally, producing a concave, or caved in, appearance in the anterior chest wall.
Examination
Examine the posture of the patient, any shoulder slope. Assess the severity of the defect and the asymmetry of the chest. You should also assess the degree of sternal involvement (related to severity), the diameter and movement of the chest wall, anterior flaring of the lower ribs, and the presence of scoliosis. Complete skeletal examination should be performed to rule out Marfan and Poland associations. Complete examination of the heart and lung should be performed.
Treatment
Nonsurgical treatment includes physiotherapy to correct the posture. Usually have minimal effect on the shape of the chest.
Surgical treatment includes:
1.
Alloplastic implant: as a camouflaging technique only with silicone implant
2.
Ravitch procedure: subperichondrial cartilage and rib resection, sternal osteotomy, and fixation of the sternum in the appropriate position
3.
WADA technique: sternal molding and turnover
Minimally Invasive Repair of Pectus Excavatum (MIRPE): Nuss procedure
3.1.4 Pectus Carinatum
History
Pectus carinatum is the second most common chest wall deformity observed in children (4:1 M:F). It is the protrusion of the sternum and ribs and is the opposite of pectus excavatum. It causes less functional limitation; however, pectus carinatum can lead to significant psychological distress and thus warrants an equally aggressive management approach. Physical symptoms can include musculoskeletal chest wall discomfort particularly while lying prone, respiratory symptoms, or palpitations.
Exam
Children with pectus carinatum may present at any age but typically are brought to medical attention at the time of puberty, as the deformity becomes more prominent during the adolescent growth spurt. Two distinct entities exist. The chondromanubrial variant describes protrusion of the manubrium, or superior component of the sternum, and has been termed the “pouter pigeon breast.” The chondrogladiolar variant describes protrusion of the gladiolus or body of the sternum. This deformity has also been referred to as “keel chest.”
Treatment
Compressive orthotic bracing, anterior sternal compression applied via an implanted metal bar (Abramson/Nuss repair), or removal of the abnormal rib cartilage while preserving the perichondrium and allowing regrowth of rib cartilage to the sternum in a more anatomic fashion combined with sternal osteotomy (Ravitch procedure).
3.1.5 Accessory Breast and Polythelia


3.1.5.1 Polythelia

History
Abnormal accessory breast tissue can be found as a mass that is located along the milk line and occur in 0.4–6 % of women. The tissue is usually asymptomatic, but patients may have complaints including swelling and tenderness of the affected region, irritation from clothing, and secreting milk or discharges. If constitutional symptoms are present, cancer should be ruled out. A complete family history should be taken of similar conditions and also of any history of breast cancer.
Examination
Ectopic breast tissue is most common in the anterior axillary line but may also be present in locations such as the face, back, labia, and thighs and can involve multiple nipples (polythelia).
Treatment
Surgical excision is recommended for adequate pathological evaluation as accessory breast tissue is subject to the same diseases as normal breast tissue. Liposuction is another option.
3.1.6 Tuberous Breast
History
A hypoplastic breast deformity that may affect bilateral or unilateral breasts in varying severity. Von Heimburg, Grolleau, and Meara have all proposed similar classification schemes that are the most widely used.
Exam
The range of physical findings includes elevation of the IMF, a constricted breast base, glandular hypoplasia, deficient skin envelope, and herniation of the breast parenchyma into the NAC.
Treatment
Numerous methods have been described with all attempting to release or enlarge a constricted base, augment volume as needed (implant and/or autologous), reposition the IMF, and reduce the size and herniation of the NAC. For mild-moderate deformities, this can be done via a periareolar incision in a single-stage manner, while severe cases may require multiple stages with tissue expansion.
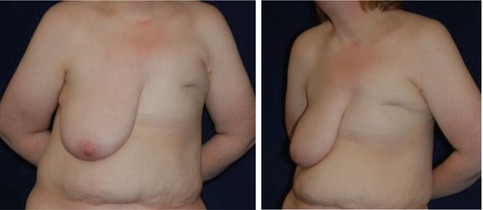
3.1.7 Juvenile Hypertrophy
Virginal breast hypertrophy, juvenile mammary hypertrophy, juvenile gigantomastia




History
Rare, extreme breast hypertrophy in peripubertal girls causing physical/psychological debilitation. Patients have a history of alarming rapid growth with breast pain, neck or back pain, and discomfort. This enlargement can occur at any time during the peripubertal period, sometimes occurring with the onset of thelarche and usually has a rapid phase lasting several months followed by a slower more indolent growth lasting years.
Exam
Exam demonstrates a firm glandular breast that may be tender and asymmetric. Patients may have a slouching posture and shoulder grooving (due to bra straps) similar to benign macromastia. Enlargement of the NAC is present as are skin changes such as thinning, ulcer or necrosis, and prominent veins. Nodules or masses may be palpated. Diagnosis is done after ruling out endocrine factors or masses in the breast.
Treatment
At the time of diagnosis, tamoxifen may be considered. A subcutaneous mastectomy with complete removal of breast tissue is the best option for recurrence but more deforming. Reduction mammoplasty has a better aesthetic but has a higher chance of recurrence; however, if followed by tamoxifen, the rate of recurrence is decreased. Patient should be counseled on the risk of recurrence with close follow-up.
3.2 Breast, Acquired
3.2.1 Breast Ptosis
Ptosis grade 1


Ptosis grade 2


Ptosis grade 3


Ptosis grade 3 (severe)


Diagnosis
Breast ptosis
History
Breast ptosis describes a descent of the breast parenchyma (nipple-areolar complex (NAC) and breast tissue). Etiologies include congenital (lower pole hypoplasia), acquired (idiopathic, involutional—postpartum/menopause), and iatrogenic (post-reduction or augmentation). Presurgical history should include personal or family history of breast cancer, stage of breast development, pregnancy/menopause changes, size changes with weight gain or loss, previous procedures, lactation, and future pregnancy plans.
Exam
Initial exam should include a breast exam and assessment of the degree of breast ptosis (Regnault’s). Other important points to look for are symmetry, quality of breast tissue, skin quality and elasticity, scars and striae, and NAC shape and size.
Regnault’s Classification
-
Grade I: Mild ptosis—The nipple is at the level of the inframammary fold and above most of the lower breast tissue.
-
Grade II: Moderate ptosis—The nipple is located below the inframammary fold but still lies anterior and superior to the lowest contour of the breast.
-
Grade III: Severe ptosis—The nipple is below the inframammary fold and at the lowest portion of the breast, pointing downward.
-
Pseudoptosis (Glandular ptosis)—The nipple is located either at or above the inframammary fold, while the lower portion of the breast falls below the fold. This is most often seen when a woman stops nursing, as her milk glands atrophy, and her breast tissue descends.
Treatment
Directed by the classification, ranging from augmentation plus limited periareolar pexy to major skin resection. Mastopexy typically involves redistribution of the breast tissues with removal of excess skin. The procedure can be combined with breast augmentation to increase upper pole fullness.
3.2.2 Mondor’s Disease

History
Mondor’s disease is a self-limiting benign disease caused by thrombosis of the superficial veins of the anterolateral chest wall possibly secondary to retractile scarring of the fascia after breast surgery or biopsies with concomitant vein thrombosis.
Examination
Skin of the chest demonstrates tender cord-like lump. The diagnosis is confirmed by ultrasound—direct or indirect signs of thrombosis in the superficial veins.
Treatment
-
Chest wall: Spontaneous recovery in 2–8 weeks, anticoagulation is not needed.
-
Post breast surgery: This is not a thrombotic process. Reports suggest that manual rupture of the fibrous bands ensures immediate functional recovery and pain relief.
3.2.3 Macromastia

History
Patients with macromastia present to the clinic with enlarged breasts that tend to be ptotic and that cause chest, neck, back, and shoulder pain; difficulty performing deep inspirations; and the inability to fit into proper clothing.
Exam
Patients may show shoulder indentations from the brassiere and inframammary intertrigo. In patients over 30, a mammogram should be obtained for breast cancer screening pre-op. Measurements are taken to evaluate extent of breast ptosis and weight of the breasts.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree