

■ Radiation oncologists usually perform the multiple catheter insertions and surgeons insert the single insertion/multiple catheter devices (which is the focus of this chapter).
PATIENT HISTORY AND PHYSICAL FINDINGS
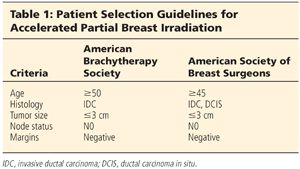
■ Patient selection for APBI is critically important (not everyone is a candidate).
■ The American Society of Breast Surgeons1 and the American Brachytherapy Society2 have published guidelines for patient selection (Table 1).
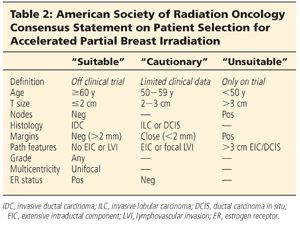
■ The American Society of Radiation Oncology (ASTRO) has published a consensus statement on patient selection for APBI (Table 2).3
IMAGING AND OTHER DIAGNOSTIC STUDIES
■ Controversy exists whether all patients undergoing APBI should get preoperative advanced breast imaging (magnetic resonance imaging [MRI] or positron emission mammography); however, most surgeons only do so selectively.
■ Ultrasound skills by the surgeon are helpful for insertion but are not mandatory.
SURGICAL MANAGEMENT
■ Brachytherapy devices are routinely placed in the surgeon’s office.
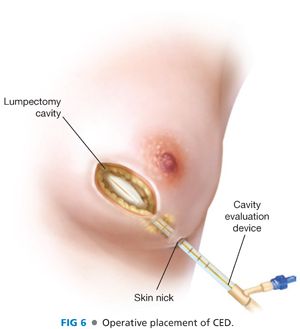
■ Cavity evaluation devices (CEDs) (FIG 5) can be inserted at the time of the lumpectomy as a “space holder” until exchanged in the office for the brachytherapy device.

Preoperative Planning
■ Preoperative consultation with the radiation oncologist will be helpful in facilitating postoperative treatment scheduling.
■ Postlumpectomy placement in the office begins with the preoperative plan for the lumpectomy including
■ Location of incisions (do not perform sentinel lymph node biopsy through the lumpectomy incision)
■ Use of oncoplastic techniques (minimal flap rearrangement is okay but major flap movement with obliteration of the lumpectomy cavity negates the use of APBI)
■ Thicker wound closure if possible (more tissue between skin and cavity may require skin resection and multilayer closure)
Positioning
■ Operative: No changes needed for CED placement.
■ Office: Generally, brachytherapy devices are placed from lateral to medial to minimize the nontherapeutic radiation that other parts of the body receive as the brachytherapy seed travels into and out of each of the catheters.
TECHNIQUES
OPERATIVE PLACEMENT OF A CAVITY EVALUATION DEVICE
First Step
■ After lumpectomy but before closure, a small skin nick is made laterally or inferiorly and the CED is tunneled from the skin nick into the lumpectomy cavity (FIG 6).
Second Step
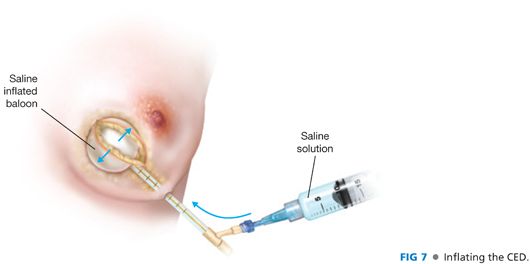
■ Inflate the balloon with enough saline to fill the cavity (FIG 7).
Third Step
■ Deflate the balloon and close the lumpectomy wound.
Fourth Step
■ Reinflate the balloon and note the volume used. This will assist in choosing the correct size of brachytherapy device to be placed in the office.
■ There is no need to suture the CED to the skin as the inflated balloon will hold it in place.
OFFICE EXCHANGE OF CAVITY EVALUATION DEVICE FOR BRACHYTHERAPY DEVICE
First Step
■ Review the pathology to ensure negative margins and negative sentinel node(s) and confirm with the radiation oncologist that the patient is a candidate for APBI.
Second Step
■
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








