38 Bladder Drainage and Urinary Protective Methods
BLADDER DRAINAGE
Transurethral Catheterization
The first self-retaining transurethral catheter was described in 1937 by Foley. A saline-inflated intravesical balloon holds the catheter in place. The ease of insertion of the Foley catheter has led to its use in various situations in which bladder drainage or monitoring of urine output is required. The Foley is commonly used after many gynecologic procedures. The major gynecologic indication for use of a transurethral Foley catheter is bladder drainage after operative procedures, with little or no dissection around the urethra (such as a vaginal or abdominal hysterectomy). It can be also used when the need for drainage is expected to be fewer than 5 days or for a short time before beginning intermittent self-catheterization. It can be made of silicone/silastic or latex; no difference in inflammatory response is present over the long term.
The major difficulty with use of transurethral drainage is the potential for infection. The risk of infection after a single catheterization is 1% to 5%. The risk rises to 20% of patients maintained on closed drainage systems. Bacterial colonization of a closed system is unavoidable, with a rate of 5% to 10% per day. Asymptomatic bacteriuria, in the presence of an indwelling catheter, does not require treatment. Prophylactic antibiotics do not prevent bacteriuria or cystitis in the presence of a catheter, although they may postpone their onset. They may promote development of resistant organisms, although treatment after removal of the catheter may be useful. The use of periurethral antiseptic gels does not help prevent infection. Box 38-1 lists the Centers for Disease Control and Prevention (CDC) Guidelines for prevention of catheter-associated urinary tract infection.
BOX 38-1 CDC GUIDELINES FOR PREVENTION OF CATHETER-ASSOCIATED URINARY TRACT INFECTION
Suprapubic Catheterization
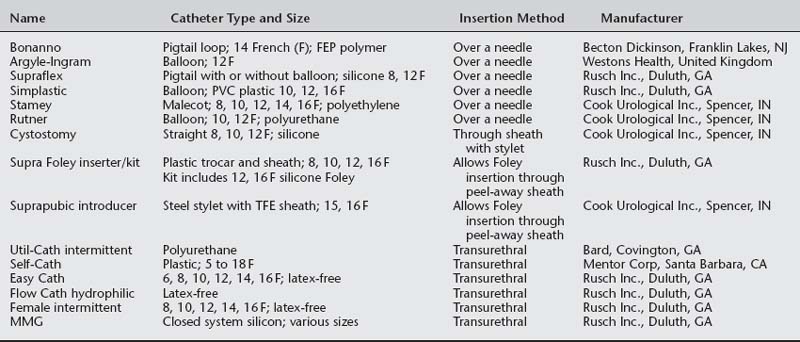
Hodgkinson and Hodari (1966) demonstrated a lower incidence of bacteriuria and shorter time to reestablish normal voiding with suprapubic bladder drainage, compared to transurethral drainage, after surgical procedures for incontinence. Other studies have supported these findings. Suprapubic catheters also improve patient comfort and ease of nursing care. They allow patients to control voiding trials, and they eliminate the need for transurethral catheterizations to check postvoid residual urine volumes. This makes them preferable for longer-term (more than a few days) use and in patients in whom postoperative retention is expected, such as the elderly and those with low flow rates on preoperative urodynamic testing (Table 38-1).
Like transurethral drainage, the main problem with suprapubic catheterization is infection, but to a lesser degree. In the postoperative setting, suprapubic drainage has a lower rate of infection than transurethral drainage. A recent randomized double-blind trial by Rogers et al. (2004) suggested that prophylaxis with nitrofurantoin until the catheter was removed decreased the rate of positive urine cultures, without selection for resistant organisms. When used for long-term drainage in patients with spinal cord injuries, 51% developed infections and 100% had asymptomatic bacteriuria. Other risks are associated with their use. Urinary deposits and blood clots may obstruct the smaller-caliber catheters, necessitating frequent irrigation. Leakage around the catheter may also be a problem. The invasive nature of insertion can lead to rare complications, such as hematuria, cellulitis, bowel injury, urine extravasation, and catheter fracture. Contraindications to suprapubic insertion, especially closed insertion, include extensive abdominal adhesions from previous surgeries, extensive intraoperative bladder reconstruction, and postoperative anticoagulation therapy. Despite these potential problems, suprapubic catheters are preferred to transurethral catheters when prolonged drainage is anticipated or when significant dissection around the urethra has been performed.
The major catheter types available are listed in Table 38-1 and shown in Figure 38-1. All are refinements of the original catheter and are inserted through a sharp trocar cannula or over a needle obturator. In general, a 10- to 12-French size is sufficient unless hematuria or debris is anticipated, in which case a larger 14- or 16-French bore is preferable.
Suprapubic catheters can be inserted using an open or closed technique. Cystotomy into the bladder dome under direct visualization is the safest method. This method is preferred when distention of the bladder is difficult, when gross hematuria is present, when there has been a recent cystotomy, or in the presence of malignancy. Any of the catheter types listed in Table 38-1, as well as a Foley catheter, can be used for open cystotomy. To perform this procedure, the bladder is filled with saline. A stab incision is made through the skin above or below the surgical incision with a scalpel. The catheter and introducer are passed through the skin, muscle, and fascia. The bladder is then punctured through the dome, taking care to avoid large vessels. The catheter is advanced through the sheath or over the needle guide, which is simultaneously withdrawn. Efflux of urine or saline should be ensured. If the catheter has a balloon, it is inflated. The catheter is sutured in place on the skin.
Closed insertion can be performed using various catheters, including an ordinary Foley catheter through an introducer, when there is no abdominal incision. To insert a catheter, the surgeon should place the patient in the Trendelenburg position and fill the bladder through a transurethral catheter or cystoscope, with at least 500 mL of sterile saline or water until the bladder is easily palpable abdominally. This positioning helps ensure that no bowel lies between the bladder and the anterior abdominal wall. After the usual skin prepping, the needle or trocar should be inserted through the skin and fascia into the bladder, at a point no more than 3 cm above the pubic symphysis and at an angle directed downward toward the pubic symphysis (Fig. 38-2, A). The trocar or needle is removed (Fig. 38-2, B
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree