The development of the integumentary system is a series of events that starts in utero and continues throughout life. Although at birth, skin in full-term infants is anatomically mature, functional maturity develops during the first year of life. Pediatric skin transitions again with the onset of puberty. At each stage, there are changes in transepidermal water loss, skin hydration, and skin acidity that define the specific period of development.
Key points
- •
Skin is anatomically mature at birth but continues functional maturity during the first year of life.
- •
In contrast to adults, infant skin is in a constant state of flux with changes in transepidermal water loss, hydration, lipid content, and skin acidity.
- •
Mature barrier function is critical for maintenance of thermoregulation, hydration, and protection against infection.
- •
Impaired barrier function and skin desiccation increases the risk of disease including atopic or contact dermatitis, infection, and even lethal excess water loss.
Introduction
Fetal and pediatric skin are commonly believed to have advantageous properties for wound repair, with the ability of fetal skin to undergo scarless wound repair and the inherent youthful appearance of pediatric skin. However, infant and pediatric skin are also considered to be more sensitive and prone to injury than adult skin with the cosmetic industry marketing an extensive line of delicate products exclusively for the care and hygiene of infants and children.
Introduction
Fetal and pediatric skin are commonly believed to have advantageous properties for wound repair, with the ability of fetal skin to undergo scarless wound repair and the inherent youthful appearance of pediatric skin. However, infant and pediatric skin are also considered to be more sensitive and prone to injury than adult skin with the cosmetic industry marketing an extensive line of delicate products exclusively for the care and hygiene of infants and children.
Skin development
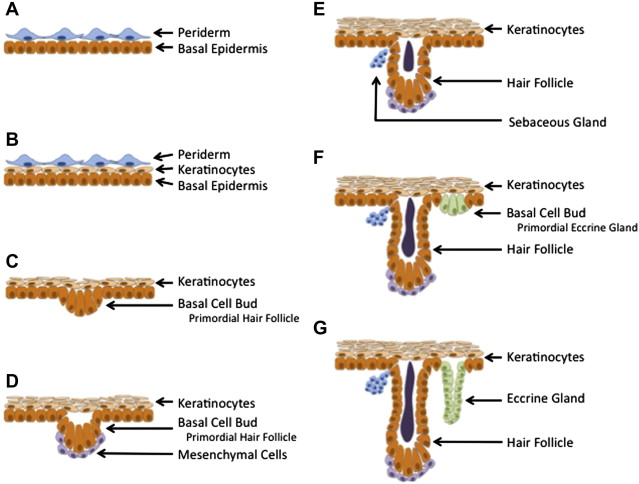
The development of the dermal/epidermal layers is a continuous process starting early in pregnancy with discrete patterns related to gestational age, developing from the cranial to the caudal pole. At 4 weeks gestation, fetal skin can be visualized as 2 distinct layers: a basal cell layer covered by an outer layer, termed the periderm ( Fig. 1 ). The periderm is uniquely found in humans; there is no counterpart in animal models such as mice or rats. Keratinization begincs at 9 weeks gestation, and at 13 weeks gestation, stratification into different layers becomes apparent. Hair follicles begin to form as epidermal buds along the basal layer at 14 weeks gestation. In the subsequent 2 weeks, these epidermal buds are associated with local proliferation of mesenchymal cells associated with the epidermal bud as hair follicles rapidly develop. This is followed by continued elongation of the hair follicles. The development of eccrine sweat glands begins as epidermal buds in the basal layer at 20 weeks gestation and continue to develop over the next 10 weeks, first by elongating and then by coiling. At 24 weeks gestation, fetal skin continues to heal without scar, as keratinization and stratification into mature morphologic layers continues. After 24 weeks gestation, there is a transitional period when skin heals without characteristic scar deposition but fails to reconstitute the dermal appendages. This transitional period has been found in multiple animal models of fetal wound healing. The scarless wound healing phenotype is lost by the third trimester. At 34 weeks gestation, mature keratinocytes characterized by flattened, keratinized morphology are observed in conjunction with adult-type dermoepidermal undulations.
In later gestation, the fetal dermis is primarily thickened by an increase in collagen content. This dermis has higher levels of type III collagen, chondroitin sulfate, proteoglycans, and hyaluronan compared with adult dermis. Dermal elastin is also absent in fetal dermis.
During the last trimester, the fetus is covered by the vernix caseosa (VC), a protective coat secreted by the sebaceous glands and composed of protein (10%), lipids (10%), and water (80%). The VC is uniquely human, with no counterpart identified in animal models. This coat was initially posited to function as a lubricant in the birthing process. However, as the fetus continues to mature, part of the vernix sloughs from the skin surface into the surrounding amniotic fluid. This physiologic decrease of vernix with advancing gestational age renders this role unlikely. More recent studies of the VC suggest that the layer facilitates the transition from an aqueous in utero environment to the dry extrauterine environment. The vernix helps to protect the fetal epidermis from maceration while immersed in amniotic fluid and permits epidermal cornification and stratum corneum formation. The VC also contains high levels of lysozyme, lactoferrin, linoleic acid, as well as other antiinfective agents.
Full-term infants at birth have skin that is anatomically mature when examined histologically with all 5 layers present. These include from deep to superficial: stratum basale, stratum spinosum, stratum granulosum, stratum licidum, and stratum corneum. As epidermal cells mature, their morphology changes from the columnar stratum basale to the tightly overlapping squamous keratinocytes of the stratum corneum. The time to fully mature, keratinize, and form this protective horny layer varies depending on body site. This occurs more rapidly in facial skin than in the trunk and limbs. Neonatal skin has a relatively coarse texture compared with older infants and a more homogeneous smooth structure develops during the first 30 days of life. Infants have smaller corneocytes and a significantly thinner stratum corneum until 2 years of age.
During the next developmental period from infancy to puberty, there is little difference in skin between male and female patients. Both genders demonstrate a steady increase in dermal thickness, with boys developing thicker epidermal and dermal layers. At the onset of puberty, there is significant hormonal influence on the skin. After age 12 years, girls accumulate a thick layer of subcutaneous fat, which is absent in boys. On the other hand, boys exhibit a gradual thinning of their thick epidermal and dermal layers. These layers remain a constant thickness in females throughout adolescence and adulthood until menopause. In addition, dermal composition begins to change with advancing age starting at puberty; both sexes show similar rates of linear decrease in skin collagen content with age. Women start with a lower baseline collagen density and they seem to age earlier than men.
Skin function
Skin has multiple functions including regulation of body temperature and protection against physical, chemical, and biological insults. In full-term neonates at birth, the skin is histologically mature, however it remains functionally immature. Neonatal barrier functions are in a constant state of flux, in contrast to mature adult skin. It has been proposed that this changing infant skin barrier is not a deficit but a benefit because adaptive flexibility allows constant optimization, balancing growth, thermoregulation, water barrier, and protective functions.
Biophysical skin parameters
Skin can be defined by a variety of biophysical skin parameters, which permit the study of skin in a noninvasive manner. Multiple parameters, including transepidermal water loss, hydration, and skin acidity, are affected in skin diseases such as atopic dermatitis, psoriasis, and allergic or irritant contact dermatitis.
Transepidermal Water Loss
Transepidermal water loss (TEWL) describes the amount of water loss through the epidermis through evaporation and depends on multiple factors, including skin temperature, skin blood flow, local hemodynamics, degree of corneocyte formation, and stratum corneum lipid content. TEWL is measured by electrical skin impedance; lower impedance indicates higher skin hydration. There is a direct relationship between TEWL and skin development. In full-term infants, there is a significant decrease in TEWL indicating a functional barrier to evaporative water loss. At birth, the sweat glands are anatomically mature, however only a small fraction of these glands are functionally mature with secretory activity. During the first few months of life, impedance values begin to decrease corresponding to the recruitment and maturation of sweat glands. These values stabilize at 4 months in full-term infants.
Premature infants, less than 32 weeks’ gestation, have lower impedance and high TEWL at birth. This excess loss is a result of immature barrier function and thinner epidermal layers, relatively increased blood flow to the skin compared with other infants, as well as a high ratio of total body surface area to volume. These factors lead to increased insensible water loss. TEWL in these premature infants can exceed 30% of their total body weight within a 24-hour period. TEWL decreases as skin continues to mature, with improved barrier function. The barrier function regulating evaporative losses varies according to anatomic location. In general, TEWL is higher in the facial region, compared with the body. The highest TEWL is reported in the nasolabial fold and perioral regions, with the lowest TEWL over the cheeks. There are no gender differences noted in the neonatal or pediatric period.
Skin Hydration
At birth, skin is transitioned from continuous immersion in an aqueous solution to exposure to relatively low humidity ambient air. Maintenance of skin hydration is critical for skin function, including plasticity, flexibility, prevention of fissures, and proper desquamation. Neonatal skin responds with a dramatic decrease in hydration at birth. Skin hydration then quickly increases for up to 90 days after birth, as the eccrine glands mature. This increased skin hydration persists for up to the first year of life and subsequently stabilizes to adult levels.
The sebaceous glands also play an important role in maintaining optimal skin hydration, secreting lipid-rich sebum. The highest sebum levels in the face are located in the nasolabial area. These glands are hormonally regulated and are active in utero , producing the VC. After birth, there are low levels of sebum protection until puberty, when it markedly increases to adult levels, particularly in boys.
Skin Acidity
Fully mature skin is characterized by a physiologic acid mantle with the pH maintained between 4.5 and 6.0. This acid mantle is an important mechanism in the skin’s defense against infection. The enzymes in the upper epidermis are optimized to function at pH 5.6. Neonatal skin is characterized by a higher pH compared with older pediatric and adult patients, regardless of gestational age, sex, mode of delivery, or body weight. This newborn skin has a different chemical composition of skin surface lipids. Maturation and maintenance of the acid mantle depends on lactic acid, free amino acids, and fatty acids found in sebum and sweat. Once established, the acid mantle is more uniformly distributed anatomically in the early pediatric population. At the onset of puberty, the intertriginous areas, such as the axilla and inguinal region, approach a neutral or even alkaline pH, as found in adults.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree




