92
Benign Melanocytic Neoplasms
Benign Pigmented Cutaneous Lesions Other Than Melanocytic Nevi
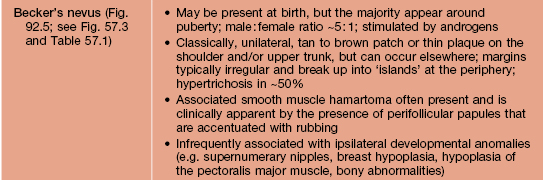
• This group of lesions can further be divided into: (1) predominantly epidermal lesions (Table 92.1; Figs. 92.1–92.5); and (2) dermal melanocytoses (Table 92.2; Figs. 92.6 and 92.7).
Table 92.1
Benign pigmented lesions other than melanocytic nevi (predominantly epidermal lesions).
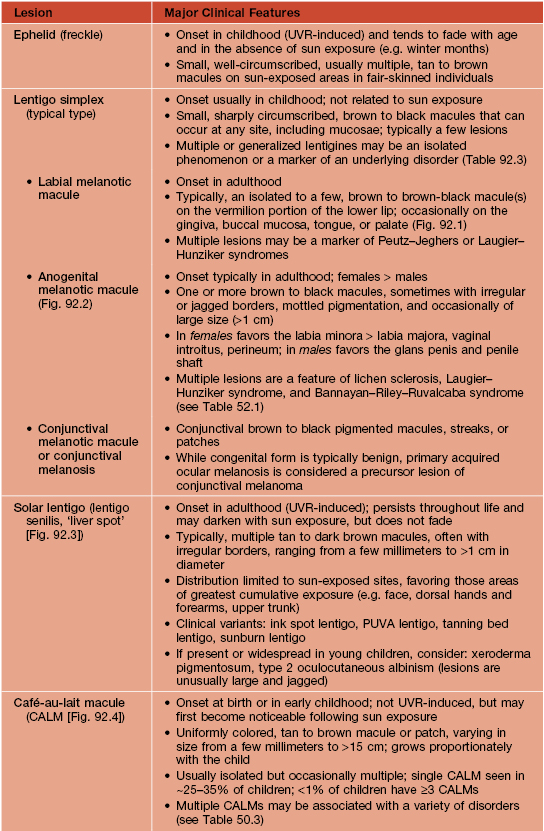
PUVA, psoralens plus ultraviolet A phototherapy.
Table 92.2
The spectrum and clinical features of dermal melanocytoses.
* DDx for nevus of Ota or Ito: patch or plaque blue nevus, ecchymosis, venous malformation; for nevus of Ito: extra-sacral Mongolian spot.
** Rx (if desired): pulsed Q-switched lasers (e.g. Q-switched ruby, alexandrite, or Nd:YAG lasers) beneficial but often requires multiple sessions.
CALM, café-au-lait macule.
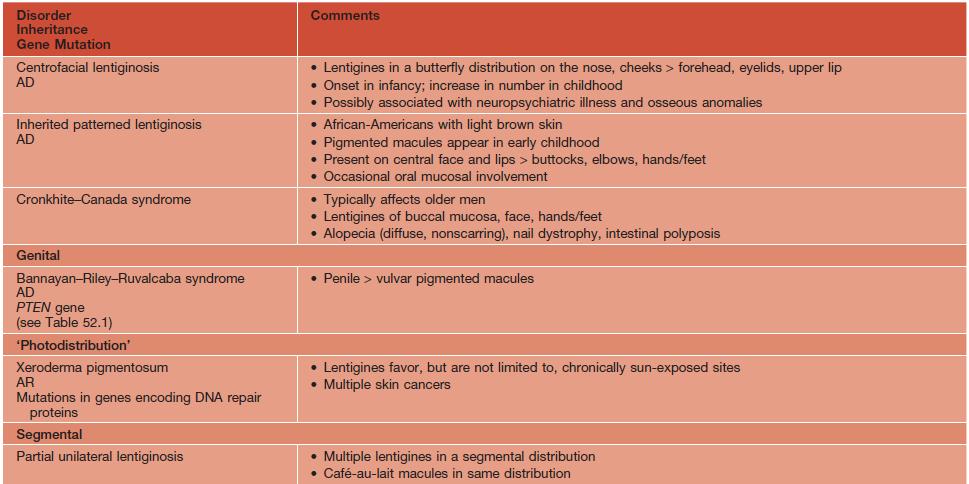
Table 92.3
Disorders associated with multiple lentigines.
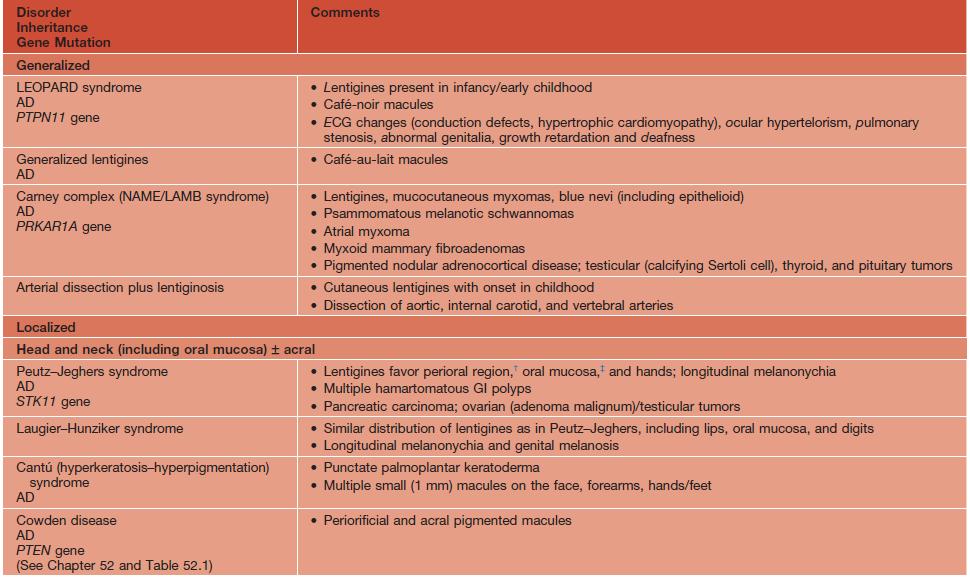
† May fade.
‡ Persists.
AD, autosomal dominant; AR, autosomal recessive; ECG, electrocardiogram; GI, gastrointestinal; LEOPARD, lentigines/ECG abnormalities/ocular hypertelorism/pulmonary stenosis/abnormalities of genitalia/retardation of growth/deafness syndrome; NAME, nevi/atrial myxoma/myxoid neurofibroma/ephelides syndrome; LAMB, lentigines/atrial myxoma/mucocutaneous myxoma/blue nevi syndrome.
Adapted from Bolognia JL. Disorders of hypopigmentation and hyperpigmentation. In Harper J, Oranje A, Prose N (eds.), Textbook of Pediatric Dermatology, 2nd edn. Oxford: Blackwell, 2006;997–1040.
Acquired Melanocytic Nevi (Moles)
• Benign proliferations of a type of melanocyte called a ‘nevus cell’.
• Both ‘ordinary’ melanocytes and nevus cells can produce melanin.
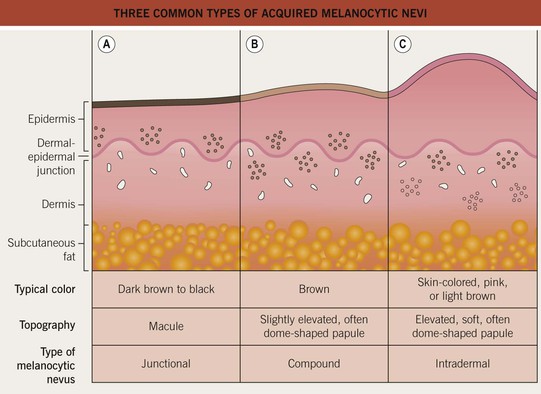
• Acquired melanocytic nevi can be categorized as common (banal) or atypical (dysplastic), and they are further named based on the histologic location of the collections of nevus cells (Fig. 92.8):
– Junctional melanocytic nevus: dermal-epidermal junction.
– Compound melanocytic nevus: dermal–epidermal junction plus dermis.
• Variants include halo, blue, Spitz, and ‘special site’ nevi (Fig. 92.9).
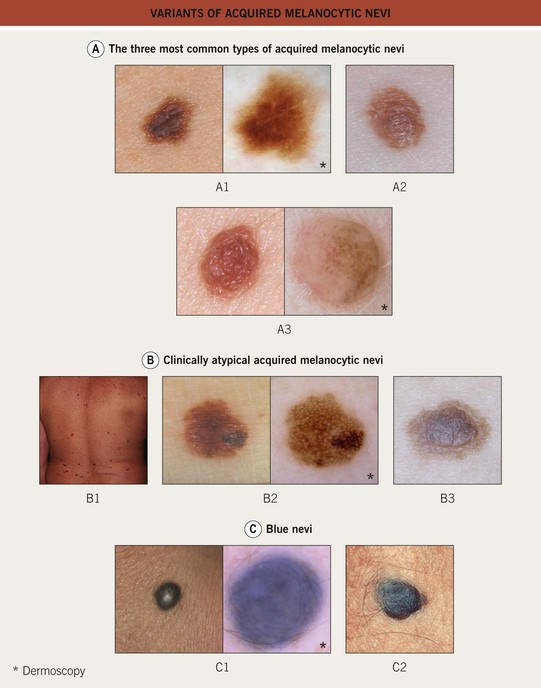
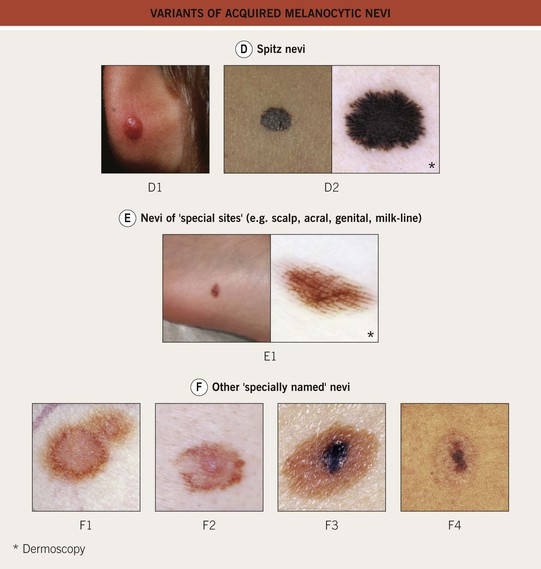
Fig. 92.9 Variants of acquired melanocytic nevi. A The three most common types of acquired melanocytic nevi. A1 Junctional nevus. Clinically, a brown macule with central hyperpigmentation. Dermoscopically, a uniform pigment network. A2 Compound nevus. Light to medium brown papule. A3 Intradermal nevus. A light tan, soft, raised papule. Dermoscopically, focal globular-like structures, whitish structureless areas, and fine comma vessels. B Clinically atypical acquired melanocytic nevi. B1 Multiple pigmented macules and papules of varying sizes on the back. B2 Close-up photo; the dermoscopy pattern is reticular-disorganized and can be seen with uncertain lesions. B3 ‘Fried egg’ appearance, with a central elevated soft papule and macular rim. C Blue nevi. C1 Common blue nevus. By dermoscopy, blue homogeneous color typically found in blue nevi. C2 Cellular blue nevus. A firm blue plaque is a common presentation. D Spitz nevi. D1 Classic Spitz nevus. Red dome-shaped papule on the ear of a child. D2 Reed nevus, typified dermoscopically by the classic starburst pattern (regular streaks at the periphery of a heavily pigmented and symmetric small macule). E Nevi of ‘special sites’ (e.g. scalp, acral, genital, milk-line). E1 Acral nevus. A brown macule on the sole of the foot. Dermoscopically, a lattice-like pattern is seen. F Other ‘specially named’ nevi. F1 Eclipse nevus. A tan center and thinner brown rim; note the stellate appearance of the brown rim. F2 Cockade or target nevus. Central lightly pigmented papule surrounded by a tan annulus then a brown ring. F3 One variant of combined melanocytic nevus. Dark brown to black papule within an otherwise uniformly pigmented light brown nevus. The differential diagnosis includes the possibility of a melanoma developing in a nevus. F4
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree