Asian rhinoplasty is one of the most challenging ethnic rhinoplasties that plastic surgeons perform because of the thick skin and soft-tissue envelope. There are three goals: pleasing the patient, achieving an aesthetically appealing result, and preserving a natural look. Of these goals, the most arduous is to satisfy the patient, as many patients have unrealistic goals and may desire an extremely narrow Western nose. Furthermore, patients may bring in celebrity or model photographs and expect that outcome, even though it may not be suitable for their face or appear over-resected and pinched. The surgeon’s most important task is to attempt to persuade the patient that this result is nonfunctional, esthetically unfit, and difficult to achieve with their skin. For ethnic surgery, a clear and thorough grasp of nasal anatomy, function, and surgical techniques is paramount. An extensive preoperative discussion, including expectations, outcomes, and a detailed list of potential complications with the patient can prevent physician-patient miscommunication. Before surgery, it is essential to review the office examination, previous operative summary, photographs, nasal analysis sheet, problem list, and plan before proceeding with the surgical treatment.
Asian rhinoplasty is one of the most challenging ethnic rhinoplasties that plastic surgeons face primarily secondary to the lack of nasal dorsum and weak cartilaginous framework in combination with thick skin and soft-tissue envelope. Three goals that should be achieved are as follows:
- 1.
Pleasing the patient
- 2.
Achieving an aesthetically pleasing and functional result
- 3.
Maintaining a natural look.
Of these goals, pleasing the patient can prove to be the most difficult to achieve, because many patients possess unrealistic expectations and a desire to achieve an aquiline Caucasian nose. The patients may envision noses similar to those of models or celebrities, even though it may not be suitable for their faces, because of their lack of awareness of the underlying nasal structures. The surgeon’s most important task is to attempt to convince the patient that this result is unrealistic, nonfunctional, aesthetically unpleasing, and difficult to achieve with his or her thick skin. Only when this task is accomplished, with good communication and understanding of realistic outcomes between the surgeon and patient, may the surgery proceed with caution.
One of the most common problems in Asian rhinoplasty is the desire to achieve a less bulbous, Westernized nasal tip. To attain a defined nasal tip, aggressive over-resection of lower lateral cartilages is usually performed. When aggressive lower lateral cartilage reduction occurs, this usually causes the following problems: loss of projection, counterrotation (ptosis), loss of support, nasal obstruction, more bulbous nasal tip, and possible long-term nasal tip contour irregularities.
Modern rhinoplasty practices suggest that less is more and that aggressive cartilage removal is antiquated. Less cartilage removal, additional nasal support through structural grafting, and tip-suturing techniques are being advocated at national and international facial plastic meetings, suggesting that these techniques may lead to decreased revision rhinoplasties.
This article describes the Asian nasal anatomy, rhinoplasty goals, preoperative nasal evaluation and surgical planning, surgical sequence and techniques, postoperative care, risks and complications, and pearls.
Anatomy
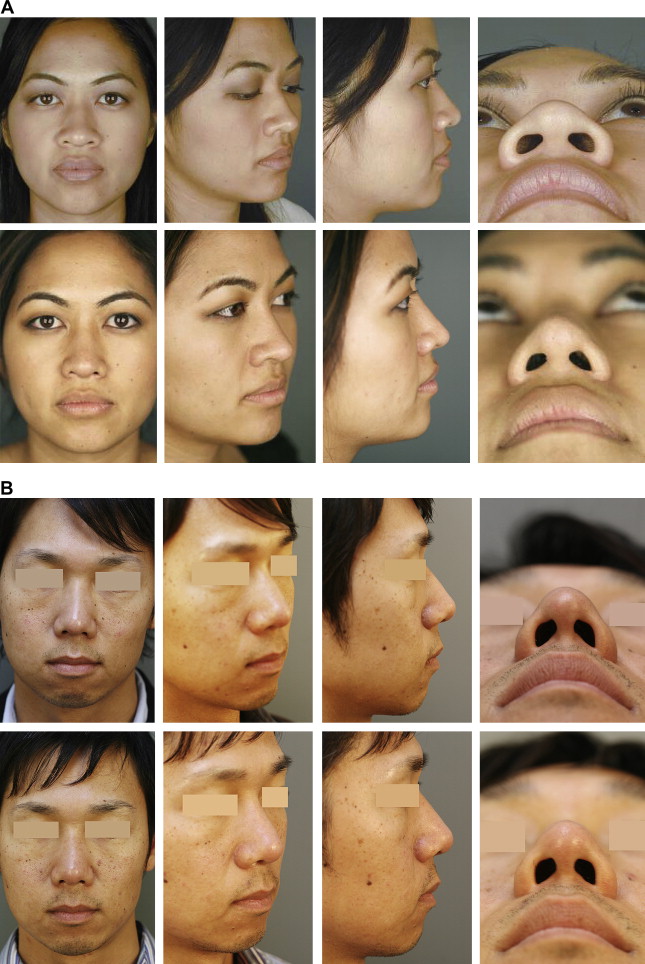
A brief description of the Asian nose is discussed and the descriptions described are present in most, but not all, typical Asian noses ( Fig. 1 A, B). These include the following:
- •
Thick skin with abundant fibrofatty tissue
- •
Deep, low, and inferiorly set radix
- •
Short, broad, and flat nasal bones with low nasal bridge and dorsum
- •
Wide, bulbous, thick-skinned, deficient, ptotic, nasal tip with abundant, fibrous, nasal superficial muscular aponeurotic system (SMAS), broad domes, minimal tip definition, flimsy and weak lower lateral cartilages
- •
Short and retracted columella
- •
Wide, thick, horizontal ala with flaring nostrils
- •
Retracted, acute nasolabial angle (less than 90 degrees) nasolabial junction with under-developed nasal spine.
Goals
The primary goals in Asian rhinoplasty are as follows:
- 1.
Thinner nasal bridge
- 2.
Augmented dorsum
- 3.
Refined tip with increased projection and rotation
- 4.
Vertically oblique nostrils and triangular nasal base
- 5.
Increased columellar length
- 6.
Obtuse nasolabial angle (greater than 90 degrees)
- 7.
Moderate skin and soft-tissue envelope thickness for aesthetically pleasing tip definition.
Goals
The primary goals in Asian rhinoplasty are as follows:
- 1.
Thinner nasal bridge
- 2.
Augmented dorsum
- 3.
Refined tip with increased projection and rotation
- 4.
Vertically oblique nostrils and triangular nasal base
- 5.
Increased columellar length
- 6.
Obtuse nasolabial angle (greater than 90 degrees)
- 7.
Moderate skin and soft-tissue envelope thickness for aesthetically pleasing tip definition.
Preoperative nasal evaluation and surgical planning
Excellent physician-patient communication is critical. During the consultation process, it is paramount to concentrate carefully on the patient’s desires and goals. It is important to assess whether or not the patient has realistic expectations and to determine the cause of the patient’s unhappiness with his or her nose. During this process, the plastic surgeon needs to assess whether the patient is a good candidate for ethnic surgery. Can your conservative rhinoplasty achieve the patient’s goals and make them satisfied with the overall result? Poor patient selection can lead to an unhappy patient and a significant amount of stress to the surgeon regardless of how successful the surgery is.
Furthermore, during the history and physical examination, special attention must be directed to determine if there is a component of nasal airway obstruction. If so, is the nasal airway obstruction static or dynamic and what are its characteristics? What factors alleviate or worsen this? For the physical examination, the authors use a nasal analysis worksheet ( Fig. 2 ) while performing a detailed visual and tactile evaluation of the nose.
During the physical examination, it is important to look, listen, and feel. First, the bilateral paramedian vertical light reflexes along the dorsum should be carefully inspected visually for symmetry.
Next, it is important to listen and observe the patient during normal and deep inspiration on frontal and basal views. Often, the diagnosis is easily identifiable, such as supra-alar, alar, or rim collapse (slitlike nostrils) during static or dynamic states. External valve collapse (lower lateral cartilage pathology) can be ascertained using a cotton-tipped applicator, while manually obstructing the contralateral nostril, to elevate the area of nasal obstruction, such as the alar rim, midalar cartilage, or supra-alar region. Often, nasal obstruction in the supra-alar region may identify an extremely narrow pyriform aperture secondary to low lateral osteotomies. By elevating the ptotic nasal tip, one can easily identify improvement of nasal airway obstruction. As the internal valve is the narrowest region of airflow, the Cottle maneuver can easily detect internal valve collapse. External visualization of the medial crura feet in the basal view can also reveal any contribution to nasal airway obstruction.
The nose should be palpated while examining the bony and cartilaginous skeleton, the tip, and skin and soft-tissue envelope to assess for any underlying asymmetries or lack of structure.
Following a thorough external nasal evaluation, the endonasal examination ensues with anterior rhinoscopy. The nasal septum is inspected for perforations, septal deviation, and for quantity of septal cartilage, because Asians often have short septums with insufficient cartilage. Other important causes of nasal obstruction are hypertrophic turbinates, obstructive synechiae between the lateral nasal wall and septum, nasal masses or polyps, and congenital abnormalities (concha bullosa).
During the physical examination, a problem list with solutions should be clearly documented on the nasal analysis sheet. For example, common problems include
- 1.
Bulbous, poorly projected tip with a plan of open rhinoplasty with structural grafting
- 2.
Low dorsum with a plan of augmentation with diced costal plan of augmentation with diced costal cartilage wrapped in costal perichondrium.
- 3.
Wide ala with a plan of bilateral alar base reduction.
If structural grafting is indicated, plan for the constituent material. A thorough knowledge of the types of autologous (septal, conchal, costal cartilage, and deep temporalis fascia) or alloplastic grafting and of harvesting techniques is needed.
In addition to standardized rhinoplasty preoperative photographs, computer imaging is useful to improve communication between surgeon and patient and visually solidify the end result. This strategy is useful only if patients are notified that the final image is not a guarantee of results. However, despite proper notification and consent, there have been reports of lawsuits filed by patients for results that are inconsistent with what was generated during the consultation. Computer imaging can help identify the patient’s expectations and unrealistic expectations can be identified through these images. Therefore, computer imaging is a powerful tool that further enhances patient evaluation for surgery. There have been numerous instances when computer morphing has identified patients with unrealistic expectations. Furthermore, the computer image can be used as a guide during surgery.
Often in Asian rhinoplasty, the patient has microgenia, and a chin implant would benefit the overall a esthetic appearance. Computer imaging will help the patient make a decision to undergo a chin implant.
Surgical sequence and techniques
Initially, attention is directed toward septoplasty and septal cartilage harvesting, with possible inferior turbinate reduction. This stage is followed by external rhinoplasty incisions and skeletonization for the external approach, or an endonasal approach if minimal tip work is to be performed, then nasal tip surgery with harvest/placement of autologous grafts, osteotomies if indicated, and next dorsal augmentation with autologous or alloplastic grafts, and lastly alar base reduction.
Septoplasty and inferior turbinate reduction
Asian noses rarely exhibit a deviated septum. If a deviated septum is identified, a standard septoplasty is performed. If the septum is not deviated, septal cartilage is harvested, leaving approximately 10 mm for the caudal and dorsal strut. Often, only a small amount of cartilage is harvested, which is insufficient for grafting, and auricular cartilage or costal cartilage for structural and dorsal grafting is often necessary. The patients are always informed preoperatively that this is a possibility. The literature notes multiple techniques and approaches to correct a deviated septum, so this is not discussed in detail here. If indicated, conservative turbinate reduction by your method of choice can be performed.
Open rhinoplasty
Injection
Most Asian rhinoplasties require an external approach to maximize exposure to the underlying framework and access to the nasal tip. After infiltrating the nose with ample lidocaine with epinephrine to help hydrodissect the skin from the skin and soft-tissue envelope and for control of hemostasis, a subdermal dissection over the nasal tip is performed, leaving the superficial muscular aponeurotic system (SMAS) dorsal to the cartilage mucoperichondrium. Once the nose has been opened, additional local anesthetic is injected to hydrodissect the mucoperichondrium from the lower lateral cartilages ( Fig. 3 ). Hydrodissection aids in dissecting SMAS/mucoperichondrium en bloc ( Fig. 4 A–E) from the nasal tip to use as an onlay or camouflage a tip graft. A subperiosteal dissection over the nasal dorsum is performed if dorsal augmentation is required or if a bony hump is present.
Nasal tip surgery
Tip surgery is the most difficult part of rhinoplasty, especially because the goals are improved definition, narrowed tip, increased projection, and rotation. If adequate projection is present with an over-rotated infratip lobule, a bruised cartilage infratip lobule graft Fig. 5 may be placed. Fig. 6 are often employed in most Asian rhinoplasty because poor tip projection is often identified.









