Anterior Cervical and Lateral Cervical Apron Skin Flaps
B. W. EDGERTON
EDITORIAL COMMENT
This clever way of obtaining thin skin to resurface the floor of the mouth has the disadvantage that it cannot be used in postradiation neck dissections, particularly if the carotid vessels are exposed. The temporary fistula would be a serious disadvantage if radiation were contemplated postoperatively. The fistula can be avoided (see text). The author continues to believe that the safest and simplest techniques should be used when the results are comparable; regional flaps do sometimes get neglected.
Following World War II, the need for a method of immediate reconstruction of the lining of the oral cavity following surgical resection of large malignant tumors stimulated the design of a variety of new pedicle skin flaps about the head and neck (1, 2, 3). One of the most useful of these new regional flaps proved to be the cervical apron flap. Even in the 1990s this method offers certain advantages over the use of free flaps in cancer reconstruction.
INDICATIONS
The reconstruction of large lining defects in the oral cavity continues to be one of the (if not the most) important features in satisfactory functional rehabilitation of speech, eating, and appearance after the removal of large cancers of the head and neck. Resected lining of the oropharynx may be satisfactorily replaced by free skin grafts, but if good functional results are to be expected following resections of the anterior cavity, with or without removal of the symphysis of the mandible, a pedicle flap must be used. Bilateral nasolabial fold flaps will provide lining for the oral cavity in modest amounts (up to 2 inches), but usually the defects following adequate cancer resections are too large. The surgeon should consider the use of an apron cervical pedicle flap.
There are several advantages to the use of this particular flap in the treatment of oral cavity malignancy. The flap allows transfer of non-hair-bearing skin from the anterior or lateral neck region into the oral cavity by means of a transverse superior pedicle that is based along the lower border of the mandible. This apron of skin is used to provide needed lining for the floor of the mouth or the alveolar and buccal regions. It also will serve to replace resected tongue or to line the lower lip.
Elevation of the flap exposes the underlying deep contents of the neck, thus facilitating neck dissection and the removal of cervical lymph nodes that so often accompany the surgical excision of squamous cancer of the oral cavity. The apron cervical flap may be elevated, folded, and transferred at the time of tumor resection without prior delay procedures. It may be transferred, along with closure of the orocutaneous fistula, as a one-step procedure if desired (4).
I have continued to find the apron flap to be the most reliable and dependable “workhorse” for anterior oral cavity lining reconstruction. This flap also has proved to be of significant value in the repair of certain congenital defects, such as aglossia-adactylia, and in the repair of gunshot wounds with major losses of the floor of the mouth and mandible.
ANATOMY
The circulation to the flap is highly reliable in the absence of preoperative intensive radiation therapy to that portion of the neck. The blood supply of this flap is so vigorous that it has proved to be one of the few regional flaps in the head and neck region that will support an immediate free bone graft to a defect in the mandible—providing a high probability of bone graft osteosynthesis. Pedicle flaps of less vigor, such as those from the chest or shoulders, often are associated with slow bone graft absorption when used to cover an immediate bone graft. Although this is treated as a random pedicle flap, it does in fact receive descending branches from the labial vessels and from vessels reaching the flap from each lower cheek region.
In most instances, the flap is elevated so that it includes the platysma muscle underlying the entire apron flap. This muscle provides a vigorous layer of blood vessels to nourish the flap, analogous to the additional circulation provided through the deep fascia in modern fasciocutaneous flaps.
FLAP DESIGN AND DIMENSIONS
This flap must be planned from the outset of treatment because it is not possible to use it once a neck dissection has been performed through the usual neck incisions. It is a flap that should be used with caution even in a nonoperated neck if that patient’s neck has been exposed to a heavy dose of preoperative radiation.
Certain anatomic points need to be considered in the design and planning of an apron cervical flap. In female patients, the absence of hair-bearing skin in the neck gives one the latitude to design the flap so that the apron lies at a somewhat higher level on the neck than in male patients. With men, that portion of the flap destined for permanent intraoral replacement should be marked carefully to lie inferior to the normal beard line in the lower neck (Figs. 190.1 and 190.2). The width of the expected lining defect within the oral cavity should be estimated carefully. The width of the apron part of the flap need not exceed that measurement.
There is essentially no limit to the width of this flap. The pedicle will easily carry sufficient non-hair-bearing skin from the lower neck to replace the entire width of the anterior oral cavity. I have moved flaps with aprons up to 14 cm wide and 10 cm long. It is unusual to require this much flap tissue for oral cavity repair.
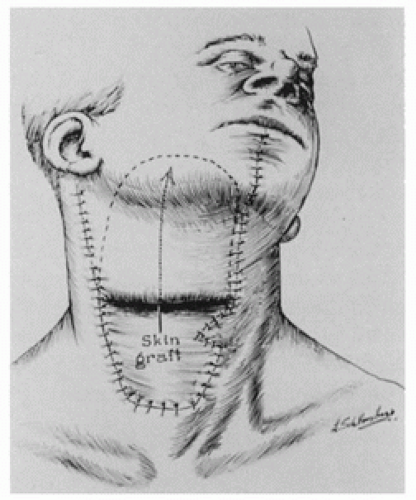 FIGURE 190.1 In the first stage, a primary cancer of the right floor of the mouth was removed in continuity with a right radical neck dissection. The contents of the deep neck were exposed by the design and shape of the apron flap. The lower part of this flap, or the “apron,” must be raised from a part of the neck below the hairline in men. In most instances, the chin and lower lip-splitting incision used here for exposure is unnecessary. I currently extend this medial incision at the hyoid level toward the mastoid process on the contralateral side. A deliberate dart is created along the anterior border of the skin graft to avoid any later linear contracture.
Stay updated, free articles. Join our Telegram channel
Full access? Get Clinical Tree
 Get Clinical Tree app for offline access
Get Clinical Tree app for offline access

|





