Supraorbital nerve—complete piercing, left side view: the view shows the supraorbital nerve (upper black arrow) already divided into its typical medial and lateral branch entering the brow through an osteofibrous channel and piercing the corrugator supercilii muscle. When the muscle plate is lifted, the branches of the supraorbital nerve (lower black arrow) can be detected. The insert in the right lower corner graphically shows the relation between the supraorbital nerve and the corrugator supercilii muscle. csm corrugator supercilii muscle, SON supraorbital nerve
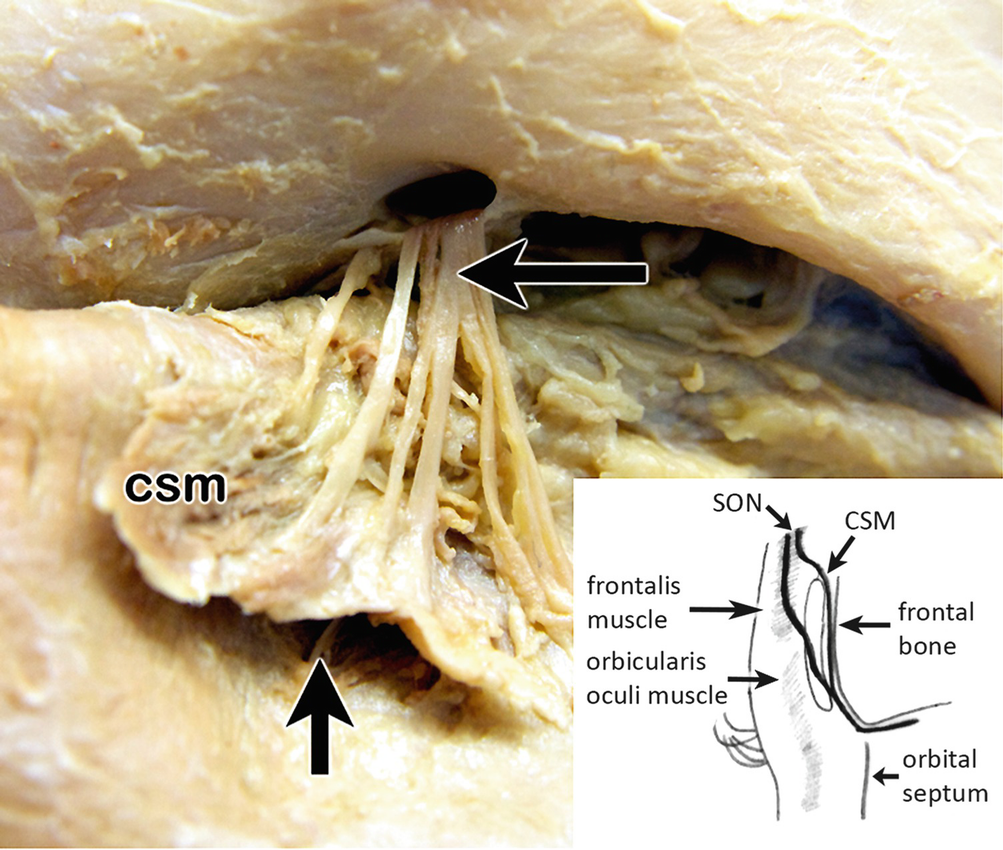
Supraorbital nerve—dividing into branches, left side view: several medial branches of the supraorbital nerve (upper black arrow) pierce the corrugator supercilii muscle completely, whereas lateral branches do not show any interaction with the muscle. When the muscle plate is lifted, the medial branches of the supraorbital nerve (lower black arrow) can be detected. The insert in the right lower corner graphically shows the relation between the supraorbital nerve and the CSM. csm corrugator supercilii muscle, SON supraorbital nerve
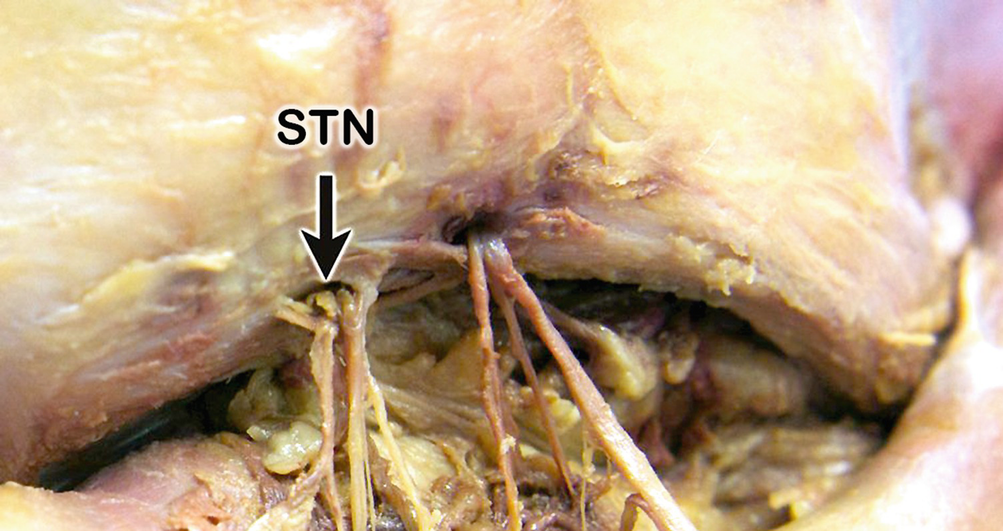
Supratrochlear nerve notch—(black arrow), left side view: supratrochlear (and supraorbital notch) bridged by a ligament at the upper orbital rim
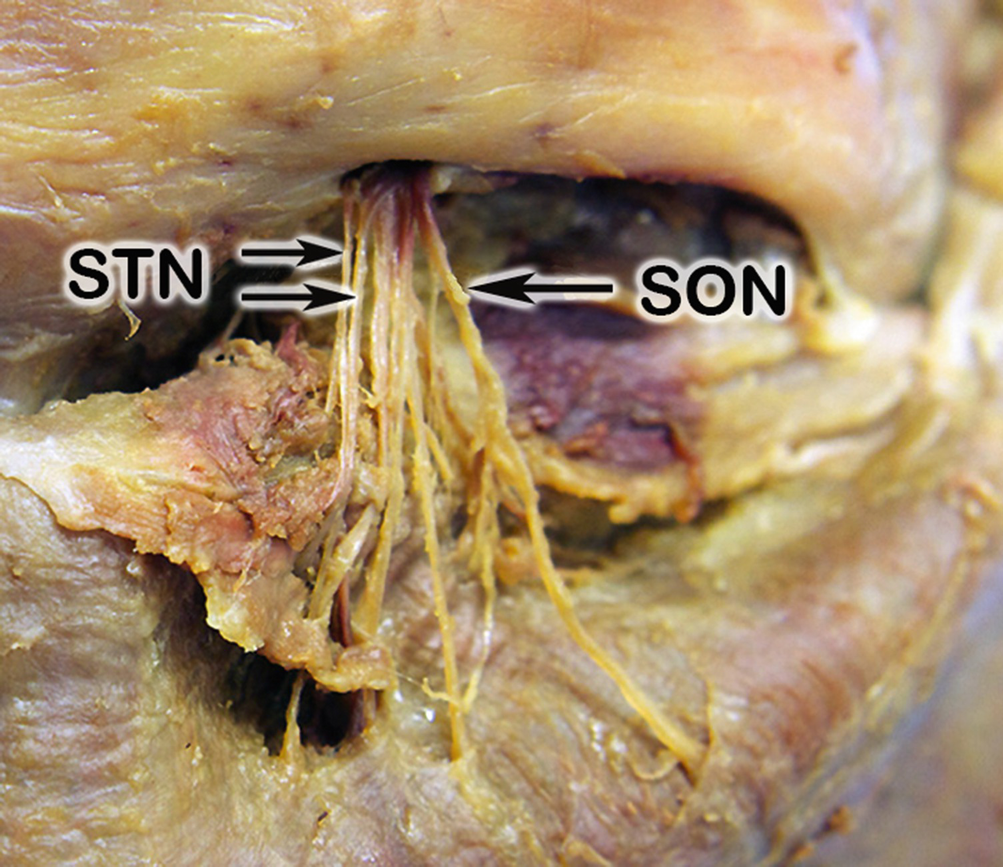
Common exit of the supraorbital and supratrochlear nerve, left side view: the picture shows the supratrochlear nerve exiting the orbit through the supraorbital notch together with the supraorbital nerve. SON supraorbital nerve, STN supratrochlear nerve
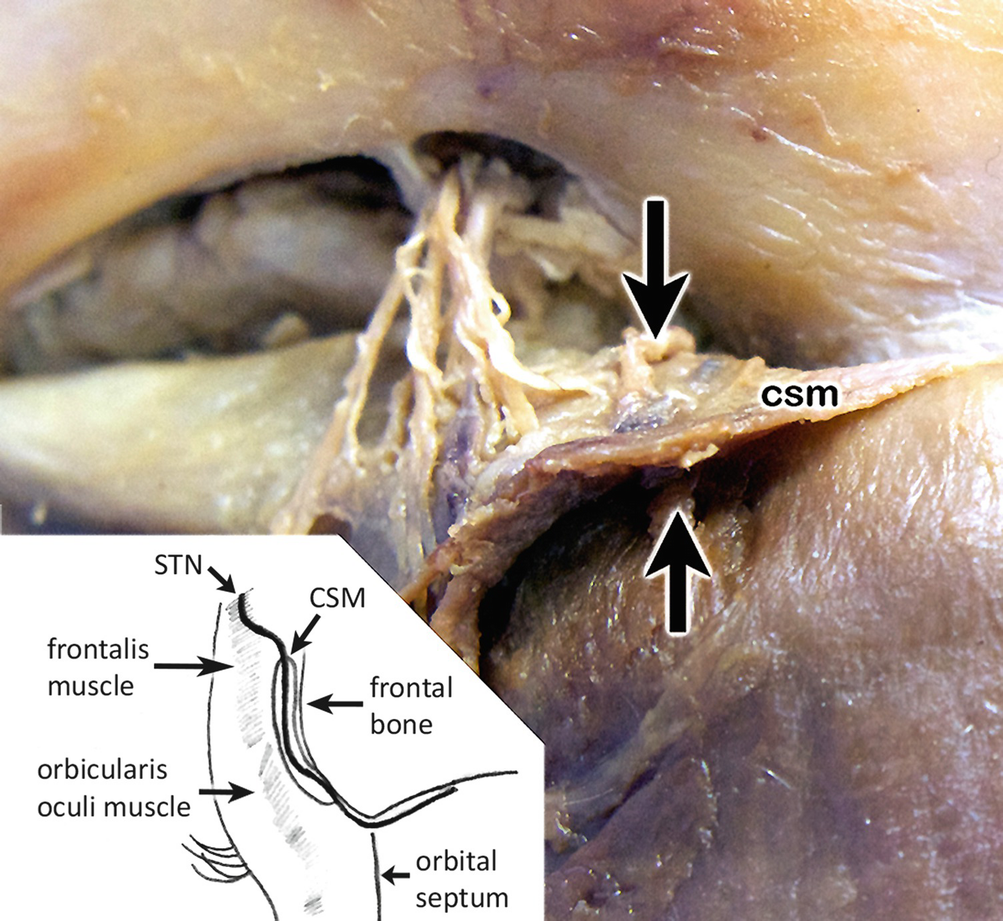
Supratrochlear nerve –complete piercing of the corrugator supercilii muscle, right side view: entrance (upper black arrow) and exit (lower black arrow) of the supratrochlear nerve. The insert in the left lower corner graphically shows the relation between the supratrochlear nerve and the corrugator supercilii muscle. csm corrugator supercilii muscle, STN supratrochlear nerve

Overview of the supraorbital and the supratrochlear nerve, left side view: the photograph presents an overview of the course of supratrochlear and supraorbital nerves and their relation to the corrugator supercilii muscle
The frontal nerve is the biggest of the three ophthalmic branches and branches off from the ophthalmic nerve within the lateral wall of the cavernous sinus. The frontal nerve enters the orbit immediately above the common tendinous ring and in between the laterally situated lacrimal nerve and the medially located trochlear nerve. Approximately in the middle of the orbit, lying directly on the levator palpebrae superioris muscle being its anatomical landmark, the nerve is divided into the STN and SON.
3.2.1 Topography of the Supraorbital Nerve (SON) (Figs. 3.1, 3.2, 3.3, 3.4, 3.5, and 3.6)
The SON as the commonly thicker branch of the frontal nerve continues the direction and usually turns slightly to medial. The branches of the SON exit the orbit in different ways and innervate the subcutaneous tissue, the skin of the frontal region, and the upper eyelid. In 59%, the SON proceeds undivided. In 41% the SON divides into a medial branch that exits the orbit through a frontal foramen or notch and a lateral branch that enters the brow also through a supraorbital foramen or notch. After its exit from the orbit, the SON usually is piercing the corrugator supercilii muscle completely. Own observations also showed cases where branches were passing by [7].
3.2.2 Topography of the Supratrochlear Nerve (STN) (Figs. 3.3, 3.4, 3.5, and 3.6)
The STN represents the commonly thinner branch of the frontal nerve and passes above the levator palpebrae superioris muscle. During its course, the STN is accompanied by the supratrochlear artery and vein. The STN courses undivided in 88% on the surface of the superior oblique muscle and exits the orbit above the trochlea. Own observations showed that in 72% the STN left the orbit through a frontal notch which was also bridged by a distinctive fibrous band [7]. In 8% it pierced also the fibrous band itself [7]. In another 18%, a true bony foramen was found. Usually the STN was already split into two separate branches before entering the CSM [7].
3.3 Occipital Surgical Nerve Anatomy (Fig. 3.7)
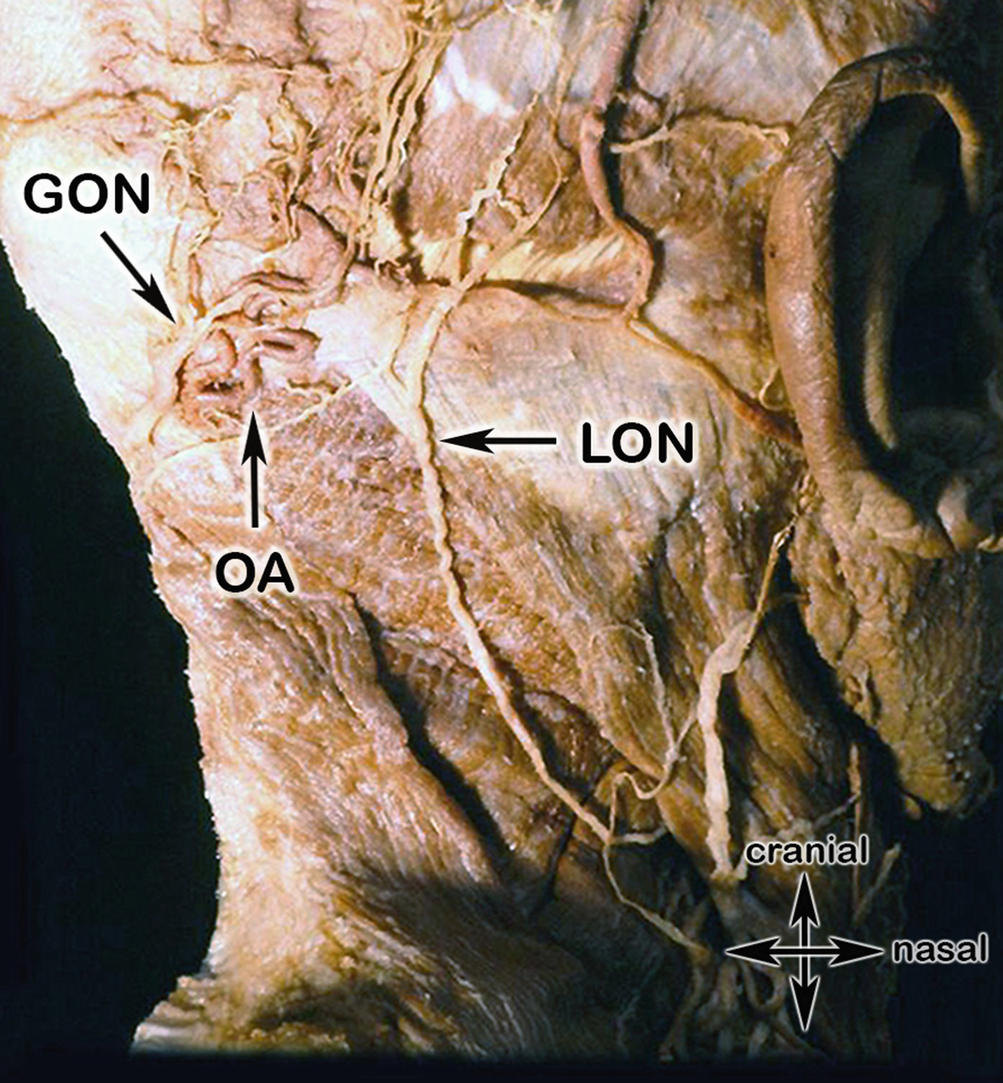
Overview of the neck and the occipital regions, right side view: the photograph shows the topographic relationship of the greater occipital nerve, the occipital artery, and the lesser occipital nerve as well as the sternocleidomastoid and trapezius muscles: GON greater occipital nerve, OA occipital artery, LON lesser occipital nerve
3.3.1 Topography of the Greater Occipital Nerve (GON) (Fig. 3.7)
The GON reaches this area along its course from deep to superficial lying on the obliquus capitis inferior muscle (sometimes penetrating this muscle), then penetrating the semispinalis and the insertion of the trapezius muscle as one trunk or already divided in its terminal branches. At its last stage of its path, the nerve or its branches pierce through a tendinous arch, the tendinous connection between the trapezius and the sternocleidomastoid muscle insertion. Along parts of its path, the GON is accompanied by the occipital vessels, often intertwining them. Therefore in this area musculature, vessels but also again fascial structures can lead to a nerve entrapment of the GON as well as of the lesser and (if present) the third occipital nerve.
3.3.2 Topography of the Lesser and Third Occipital Nerves (LON, TON) (Fig. 3.7)
While the third occipital nerve (TON) is the dorsal ramus of C3, the lesser occipital nerve (LON) is the ventral ramus of the C2 and C3 root. The topographical course of the LON is difficult due to its variability. The LON emerges from the posterior border of the sternocleidomastoid muscle at the so-called area nervosa, penetrating the superficial layer of the cervical fascia and running dorso-cranially to the neck and occipital region. During its further course at the occipital area, it can intersect and/or intertwine with the occipital artery, depending on its course more medially or laterally. At the border of the insertions of the sternocleidomastoid and the trapezius muscle, the LON also can be compressed by the tendinous arch, the cranial connection of both muscles.
What has to be pointed out is the frequently high variability of these nerves in this region: a so-called vicarious course of the GON and LON has to be borne in mind. In this case (as also shown in Fig. 3.7), a normal small LON is quite big and interacts with a “small” GON. The LON in this case is able to supply most of the sensory area of the GON.
If present, a sensory TON, the medial branch of the posterior division of the cervical root C3, at the end of its course also pierces the trapezius muscle and ends in the skin of the caudal part of the neck, regularly lying medial to and communicating with the GON.
3.4 Zygomaticotemporal Surgical Nerve Anatomy
The parotideomasseteric and zygomaticotemporal regions also contain sensory peripheral nerves, which also could be entrapped by anatomical structures and therefore may be also a cause for a central sensitization and could trigger a migraine headache [9, 12, 24].
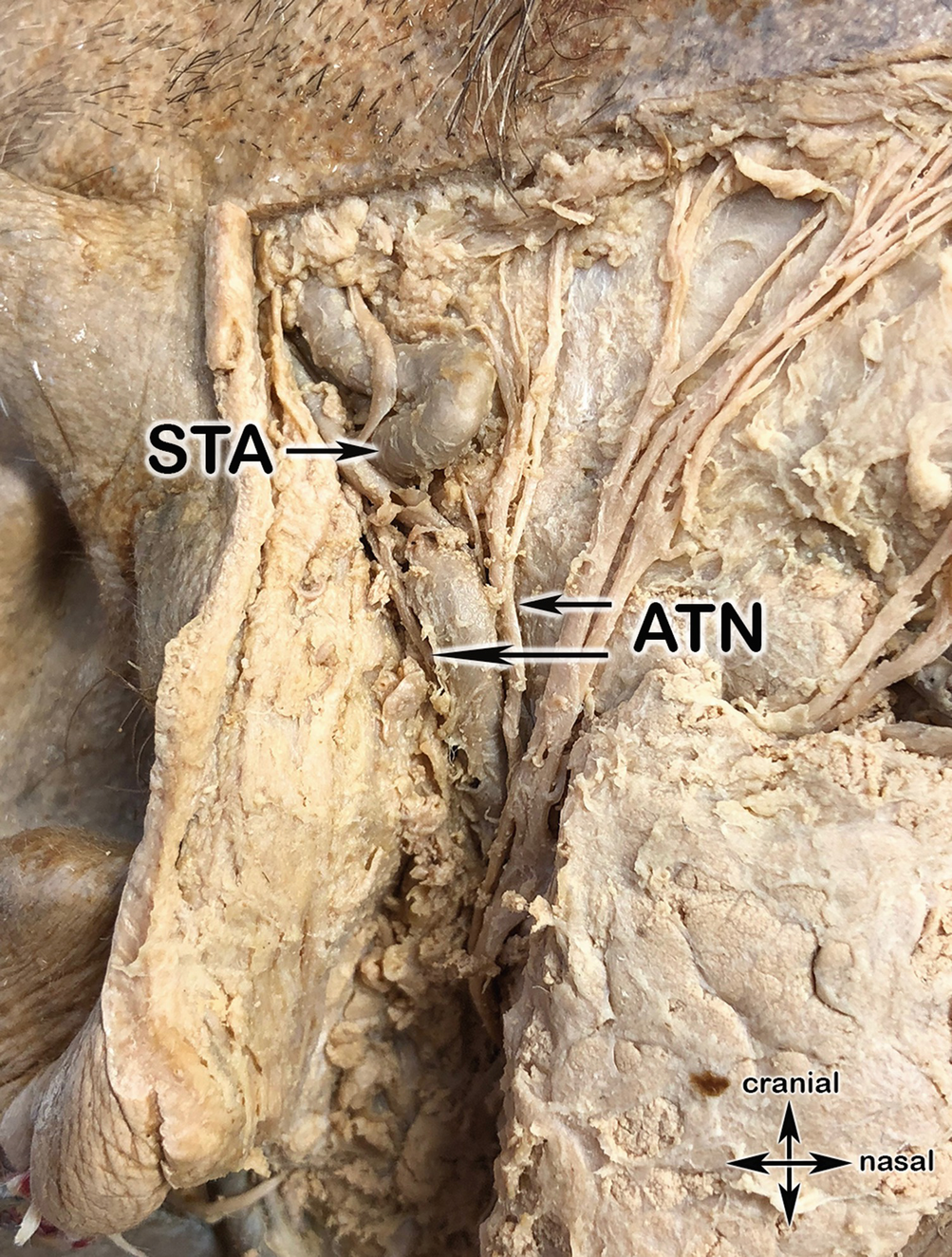
3.4.1 Topography of the Auriculotemporal Nerve (ATN) (Figs. 3.8 and 3.9)

Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree