1 Anatomy for plastic surgery of the breast
Synopsis
 Size, symmetry, proportionality and the location of the breast and its landmarks on the chest wall all play a role in the attractiveness of the breast.
Size, symmetry, proportionality and the location of the breast and its landmarks on the chest wall all play a role in the attractiveness of the breast.
 Knowledge of breast anatomy, in particular, the vascular pedicle and location of the nerves, facilitates safe and effective surgical management.
Knowledge of breast anatomy, in particular, the vascular pedicle and location of the nerves, facilitates safe and effective surgical management.
 Any pre-existing asymmetries, spinal curvature, or chest wall deformities must be recognized and demonstrated to the patient, as these may be difficult to correct and can become noticeable in the postoperative period.
Any pre-existing asymmetries, spinal curvature, or chest wall deformities must be recognized and demonstrated to the patient, as these may be difficult to correct and can become noticeable in the postoperative period.
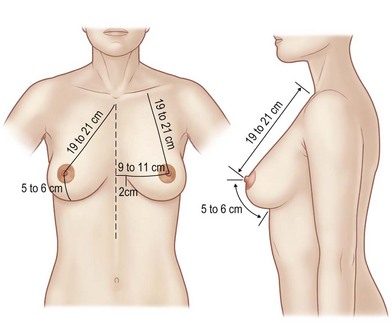
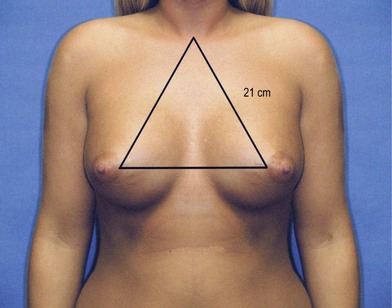
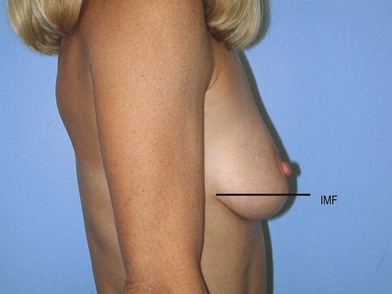
Ideal breast architecture
The appearance of the ideal breast is somewhat subjective. Each patient has their own opinion as to the aesthetics of their breasts, which should be given consideration with any operative alteration of the breast. Reconstruction or cosmetic enhancement of the breast encompasses not only the way the breast looks, but also how it feels to the touch. Size, symmetry, proportionality and the location of the breast and its landmarks on the chest wall all play a role in the attractiveness of the breast. Statistical standards for the dimensions of the breast have been analyzed and reported by various authors (Fig. 1.1).1–7 The distance from the sternal notch to the nipple and the distance from the midclavicular line are each 19–21 cm. The distance from nipple to the inframammary fold is 5–7 cm (Fig. 1.1). The distance from the nipple to the midline is 9–11 cm. These measurements offer guidelines for altering the breast, which must be individualized, based on proportionality, variances in chest wall anatomy, posture and patient preference (Fig. 1.2).
Development of the breast
The breast originates from the ectoderm, the germinal layer which forms the initial breast bud. The connective tissue is derived from the mesoderm. A group of glands, derived from the epidermis, develops within the dermis and underlying fascia. Breast development occurs along the milk line, which extends from the axilla to the groin. The normal breast develops at the level of the fourth intercostal space on the anterolateral chest wall. Supernumerary breast formation can occur anywhere along the milk line (Fig. 1.3). The most common location of supernumerary breast formation is at the inframammary crease on the left side, but additional breast formation can occur in the axilla as well.
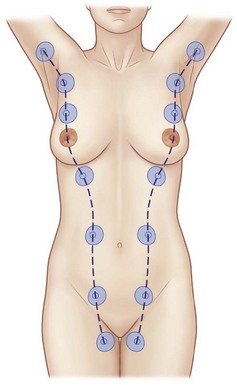
Fig. 1.3 The milk lines.
(Reproduced with permission from Standring S, ed. Gray’s anatomy, 40th edn. London: Churchill Livingstone; 2008.)
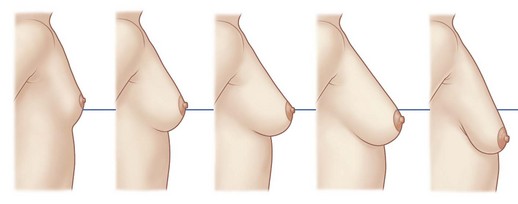
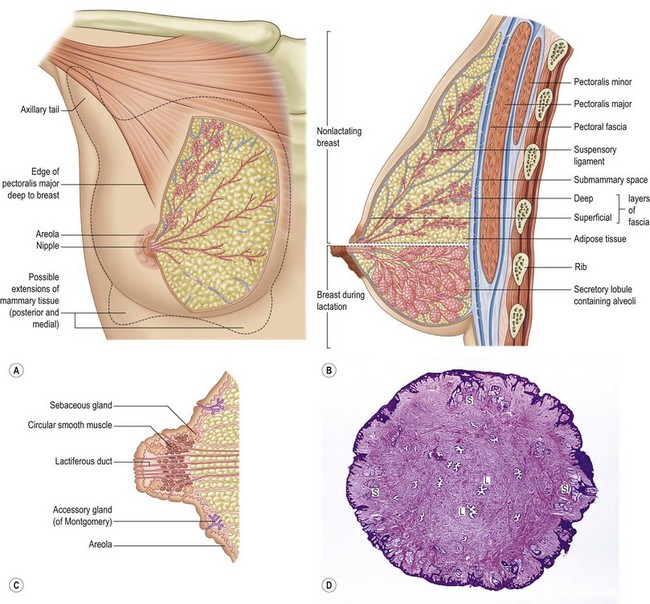
Following a brief period of activity shortly after birth in response to maternal hormones, breast development is quiescent until puberty. Onset of puberty occurs at approximately 9 years of age (Fig. 1.4). Typically, by age 14, parenchymal growth has extended to its mature borders. These include the clavicle at the superior border, the sternum at the medial border, the inframammary fold for the inferior border and the anterior border of the latissimus dorsi for the lateral border. Breast tissue can extend beyond the borders particularly medially and inferiorly. The breast tissue that extends laterally through the axillary fascia into the axillary fat pad is referred to as the “tail of Spence.” Mature breast morphology projects from the chest wall in a conical fashion with its greatest point of projection at the nipple areolar complex (Fig. 1.5).
Development of breast shape is dependent on many factors, including fat content, volume, muscular and skeletal contour and skin and connective tissue compliment. In particular, the Cooper’s ligaments provide structural support for the breast parenchyma. These structures combine to provide the final breast shape; it is dependent in large part on heredity and will change with age as the suspensory structure become lax and the breast becomes more ptotic (Fig. 1.6).
Parenchyma
The glandular tissue of the breast is dispersed through a significant amount of adipose tissue.8 The glands themselves consist of millions of lobules clustered together into 20–25 lobes. Interlobular ducts join to form approximately 20 primary lactiferous ducts that open onto the nipple areolar complex. The lactiferous ducts converge into a specialized ductile network, which stores the milk prior to lactation. The glandular parenchymal ducts are lined with cuboidal cells which transition to stratified squamous epithelium in the ductile and sinus network (Fig. 1.5).
An intricate fascial layer supports the breast tissue. The parenchyma is fixed in placed by the superficial fascial system, which extends cephalad from the abdomen, diverges into a superficial and deep component enveloping the breast tissue and maintaining its attachment to the breast wall (Fig. 1.7). The superficial fascial layer is an extension of Scarpa’s fascia, which envelopes the glandular tissue deep to the dermal layer. The superficial fascial layer and the dermis can be difficult to distinguish. Subcutaneous fatty tissue between the dermis and the superficial fascia distinguish the two layers. The deep layer diverges at the level of the sixth rib, where the inframammary fold is the inferior border of the parenchyma.
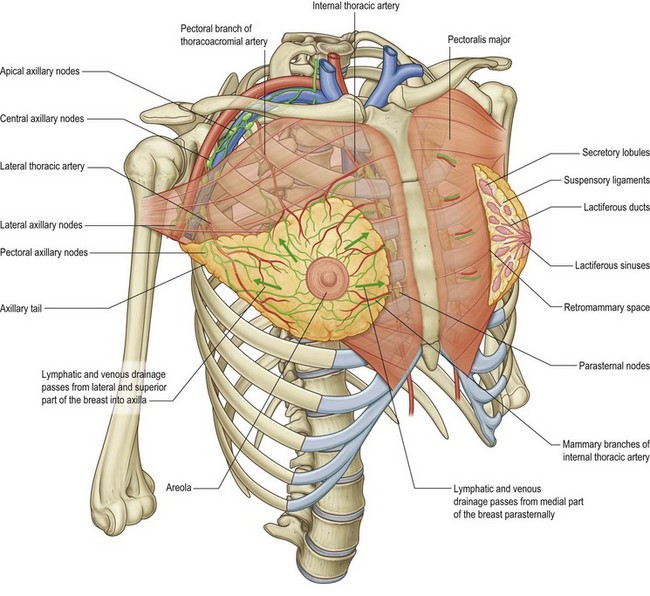
Fig. 1.7 The relations of the breast.
(Reproduced with permission from Drake et al., Gray’s anatomy for students. London: Churchill Livingstone; 2005.)
The Cooper’s ligaments provide numerous interconnections between the deep and superficial fascial layers. These ligaments pass through ad invest in the breast parenchyma securing to the pectoralis fascia. With attenuation of these support structures, breast ptosis will develop (see Fig. 1.14). Regnault delineated a classification system for mammary ptosis describing the relative positions of the nipple and the inframammary fold.9
• Mild (first-degree) ptosis is described when the nipple lies at the level of the inframammary fold.
• Moderate (second-degree) ptosis is a descent of the nipple lies below the level of the inframammary fold but it remains above the most projected portion of the breast.
• Severe (third-degree) ptosis is present when the nipple lies below the inframammary fold at the lower contour of the breast and skin brassiere.
• A separate variant, pseudoptosis is present when the inferior pole of the breast descends, but the nipple lies above the level of the inframammary fold. The areola-to-inframammary fold distance is increased. Pseudoptosis can occur naturally as well as when bottoming out of a reduced breast occurs.
• Other descriptions of ptosis include the morphologic varieties and how they affect appropriate surgical management. These include the previously mentioned true ptosis, pseudoptosis as well as glandular ptosis.
Nipple areola complex
Because the nipple is the focus of the breast, maximizing its location and maintaining its function are of critical importance when performing breast surgery of any type. Fortunately, the blood supply to the nipple, as with the breast parenchyma, is redundant and rich. The internal mammary perforator, lateral thoracic perforators, and the intercostal perforators from both the anterolateral and anteromedial origins all provide arterial supply to the subdermal plexus of the nipple.10
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree