Anatomy and Functional Anatomy of the Hand In their biological taxonomy and status as “higher-level mammal—homo sapiens,” humans owe their distinction from primates to the miraculous structure of the hand. With its 19 degrees of freedom and its opposing thumb, the hand is a highly developed and complex grasping organ. This enables a wide range of movement combinations while simultaneously allowing adaptation of force, speed, and facileness. Moreover, the hand also features a highly specific sensory and tactile organ that human beings use to perceive and assess themselves and their surroundings. Owing to its capacity for making gestures, the hand plays an important role in interpersonal communication. In writing, music, and the visual arts, the hand acts as a means of expression for the human mind.229 These gross and fine motor skills, along with sensory capacities, enable humans to take care of and nourish their bodies, as well as communicate and shape their environment. With all these possibilities, the hand also plays a major role in self-expression and in developing the human mind, and significantly contributes to modifying human motor capacities.202 The mobilizing of this functionality requires exceptional interaction between the central control system and anatomical structures such as bones and joints, muscles and tendons, nerves and blood vessels, making the hand an extremely complex organ. The distal area of the lower arm consists of the distal radioulnar joint, the thumb and finger carpometacarpal (CMC) joints, the palm, and the fingers. In total, there are 27 bones with 36 articulations and 39 active muscles. In order for the hand to translate its wide range of fine and gross motor capabilities into its complex range of motion, these structures must all be coordinated. The forearm skeleton consists of two bones: the ulna (elbow bone) and the radius. These two bones form two radioulnar joints, one near the elbow (proximal radioulnar joint) and one near the wrist (distal radioulnar joint) ( ▶ Fig. 1.1). Pronation and supination movements are performed by these two joints with a contribution from the shoulder joint ( ▶ Fig. 1.2).233 During this movement, the radius takes a conical path, in which the rotation axis courses from the radial head through to the distal end of the ulna.3 In so doing, the radial head rotates around itself within the anular ligament (wide ringlike band) in the proximal radioulnar joint, while the radius simultaneously moves around the ulna (ulnar head) in the distal radioulnar joint. During supination, the radius and ulna are parallel, whereas these two cross during pronation, with the radius overlying the ulna. The range of the forearm’s rotational motion is between 140° and 150°.190 During pronation, the ulna glides more toward the dorsal aspect, and during supination it glides more toward the palmar aspect,262 which extends the movement to 180°.229 The range of motion from the neutral zero position for pure pronation and supination is therefore approximately 80° to 90°–0–80° to 90°, or an average of 85° supination and 90° pronation.233 With the contribution of the shoulder joint (continued movement), this range can increase to up to 230°.256 These possibilities of additional and substitute movements can simulate movements in the radioulnar joint by means of “pseudo-movements.”149 The hand must follow these movements, since the proximal condyloid wrist joint does not allow any compensatory movements.149 Fig. 1.1 Distal and proximal radioulnar joints. Fig. 1.2 Pronation and supination of the hand. In functional terms, the proximal radioulnar joint is a pivot joint. It consists of the convex surface of the articular circumference of the radius and the concave surface of the radial notch of the ulna. The distal radioulnar joint, also functionally a pivot joint ( ▶ Fig. 1.3), consists of the convex semicylindrical surface of the articular circumference of the ulna, which is completely covered with cartilage, and the associated concave joint surface of the ulnar notch on the distal radius. The joint is enclosed by a thin connective-tissue capsule that has no stabilizing properties.49 Its loose structure, with deep recesses (e.g., the sacciform recess), lines the joint cavity with a synovial membrane and provides the joint with enough leeway for a total of 180° pronation and supination.160 Fig. 1.3 Functionally, the distal radioulnar joint is a pivot joint. Rotation in the distal radioulnar joint takes place around the ulna, which acts as a static reference point about which the radius rotates with the hand.233 Functionally, the radius sweeps across the surface of a conical segment.233 The greatest possible congruence of the joint surfaces occurs in the neutral zero position. In pronation and supination, the joint surfaces of the ulnar head and the ulnar notch of the radius have less contact.233 Practical Tip In the case of immobilization, the joint capsule of the distal radioulnar joint is unlikely to degenerate to the point where it will cause a restriction in movement. Even if the capsule shrinks, the only symptom will be a slightly limited range of motion. For this reason, it is usually not necessary to mobilize the joint.160 The proximal radioulnar joint is stabilized in the area of the radial head by the anular ligament of the radius and the oblique cord. In the area of the shaft, it is stabilized by the interosseous membrane of the forearm. Moreover, the radius and ulna are firmly attached to the interosseous membrane, which regulates the ulna’s relative lengthening during pronation and its relative shortening in supination.53 This means that during supination, the radius deviates distally and during pronation it deviates proximally.160 The distal radioulnar joint is stabilized on the palmar side by the pronator quadratus muscle,99 the tendon and tendon sheath of the extensor carpi ulnaris muscle145 and for the most part, by the triangular fibrocartilage complex (TFCC).112,145 The anular ligament of the radius encircles the proximal radioulnar joint (ligamentous “bracketing” between the radial head and the ulna229), guides the radial head, and absorbs pressure ( ▶ Fig. 1.4). This ring-shaped band, approximately 1 cm wide, inserts in front of and behind the radial notch at the ulna. It is funnel-shaped distally and surrounds the neck of the radius.157 Proximally, the anular ligament of the radius is fused to the collateral radial ligament200 and the collateral ulnar ligament; deeper below, it is fused with the elbow joint capsule.160 Together, they operate as a functional unit. The anular ligament consists of strong connective tissue; additional cartilage cells are present in the radial notch area78 for absorbing pressure.200 The anterior part of the ligament is under tension during supination; during pronation, the posterior part of the ligament is under tension.157 However, this tension is unlikely to restrict range of motion.160 According to Morris (1879),173 the interosseous membrane, oblique cord, ligaments of the basal joint and distal radioulnar joint, and various antebrachial muscles are more likely to serve as control structures between pronation and supination. Fig. 1.4 Anular ligament of the radius, front view. (From THIEME Atlas of Anatomy, General Anatomy and Musculoskeletal System. 2nd ed. © Thieme 2014, illustration by Karl Wesker.) Practical Tip If axial deviation persists, for example after a radial head fracture, the anular ligament of the radius may become prematurely malformed during pronation and supination. According to Matthijs et al (2003),160 however, this is not enough to restrict motion. Slipping of the radial head during rotation may explain why functionality remains intact. This small, bandlike structure arises below the radial notch of the ulna and attaches directly below the radial tuberosity.78 It is a flat, fibrous band at the proximal end of the interosseous membrane, which acts as a stabilizing ligament229 and runs in the opposite direction ( ▶ Fig. 1.5). In combination with the extensor carpi ulnaris muscle and the palmar radioulnar ligament229 it is another key contributor to decelerating supination,19,200 and with the interosseous membrane, it prevents the radius from deviating distally relative to the ulna.278 In contrast, the tendon of the biceps brachii muscle, which wraps around the radius during pronation, contributes to deceleration of pronation.200 Fig. 1.5 Oblique cord und interosseous membrane of forearm. (From THIEME Atlas of Anatomy, General Anatomy and Musculoskeletal System. 2nd ed. © Thieme 2014, illustration by Karl Wesker.) This interosseous membrane originates approximately 1 cm below the radial tuberosity and inserts shortly before the distal radioulnar joint ( ▶ Fig. 1.6), with several fibers extending into the joint capsule.91 Near the center of the radius, it reaches its maximum thickness of approximately 1 mm. It consists of strong connective tissue whose tensile strength reaches 84% that of the patellar ligament.160 This sheet of connective tissue holds together the radius and ulna.200 Functionally, it serves to protect the two bones from longitudinal shifts and acts as a surface from which various muscles originate.200 Fig. 1.6 Interosseous membrane of forearm. (From THIEME Atlas of Anatomy, General Anatomy and Musculoskeletal System. 2nd ed. © Thieme 2014, illustration by Karl Wesker.) Moreover, the interosseous membrane of the forearm contains two types of oblique collagen fibers, which Zancolli (1992)282 referred to as oblique A (OA) fibers and oblique B (OB) fibers. The OA fibers occupy the entire interosseous space and in general run from the proximal radius to the distal ulna. The OB fibers form two separate palmar bundles (one proximal and one distal) and run in the exact opposite direction.160 The OA fibers become taut in neutral position and in supination, while the OB fibers become taut in pronation. In each case, the opposing fiber is relaxed. Furthermore, Gabl et al (1998)70 described a dorsal stabilizing ligament of approximately 8 mm width, 30 mm length, and 1 mm thickness. It stabilizes the capsule of the distal radioulnar joint, and during pronation holds the ulnar head like a sling. Its opposing fiber is a falciform septum approximately 2 mm in thickness on the palmar aspect of the membrane. Measuring about 3 mm wide, this structure arises from the far distal portion of the membrane beneath the deep muscular portion of the pronator quadratus muscle.229 The interosseous membrane therefore delimits or decelerates pronation and supination. Its tissue also contains gaps through which vessels can traverse91 and it has a large share of mechanoreceptors.205 Practical Tip Since most of the interosseous membrane is relaxed during maximum pronation and supination, it is usually not considered to be a possible source of pronation and supination disturbances.160 However, with respect to oblique A and oblique B fibers, it may be deduced that the interosseous membrane may be involved in this type of restriction in the case of fracture-related instability, for example.119 This is particularly the case for instability of the triangular fibrocartilage complex (TFCC). This means that only angular techniques (rotation) may be used for traction. Translatoric movements could intensify the pathological process of the TFCC, since this structure is largely responsible for stabilizing pronation and supination.160 Thus, prior to any kind of treatment, the exact cause needs to be established. The triangular fibrocartilage complex (TFCC) ( ▶ Fig. 1.7) is formed from the following structures: The ulnocarpal disc The ulnocarpal meniscus homologue187 The ulnar collateral ligament of the wrist joint The sixth tendon compartment The ulnocarpal ligaments (dorsal and palmar radioulnar ligaments as well as the ulnolunate and ulnotriquetral ligaments) Fig. 1.7 Triangular fibrocartilagenous complex. (a) Palmar view. (b) Dorsal view. The TFCC therefore extends from the distal ulnar end of the radius to the base of the fifth metacarpal.92 During surgical dissection, it is very difficult to separate these elements, since they merge continuously.229 The functions of the TFCC include stabilization of the distal radioulnar joint (i.e., during pronation and supination) and the carpal side of the ulna (with its supporting ligaments) for movements in the proximal and distal wrist, as well as regulation of pressure in the wrist.231 The tendon sheath of the extensor carpi ulnaris muscle and the muscle itself decelerate supination, while the dorsal and plantar radioulnar ligaments of the TFCC decelerate pronation. The arrangement of the joint capsule is relatively flaccid.229 The task of distributing impacts and pressure is assumed by the ulnocarpal disc22—that is, with approximately 84% assumed by the radius and approximately 19% by the ulna.86 Occasionally, the ulna is shortened (“negative ulnar variance”) or lengthened (“positive ulnar variance”) in relation to the radius due to trauma or genetic predisposition ( ▶ Fig. 1.8). Fig. 1.8 Positive and negative ulnar variances. (a) Post-traumatic positive ulnar variance. (b) Post-traumatic negative ulnar variance. Practical Tip Unphysiological differences in the length of the radius and the ulna cause disturbed pressure relationships in the proximal radiocarpal joint and can therefore lead to severe pathologies. For example, negative ulnar variance causes pressure to increase near the articulation of the distal radius, which can contribute to necrosis of the lunate (Kienbock’s disease) ( ▶ Fig. 1.8a).113,120 Positive ulnar variance leads to an ulnar impingement syndrome, that is, degenerative tears in the TFCC combined with chondral lesions of the lunate and triquetrum ( ▶ Fig. 1.8b).36,94,160 Furthermore, variations in the length of the ulna and in relation to the radius influence the form and orientation of the joint surfaces in the distal radioulnar joint,66 whose incongruences (e.g., due to trauma) lead to degenerative changes of the joint.213 The supporting ligaments of the TFCC stabilize the proximal and distal radiocarpal joint. The following outline and description based on Schmitt (2007)231 describes the structure and function of the individual structures of the TFCC. The ulnocarpal disc ( ▶ Fig. 1.9) arises from the hyaline joint cartilage of the radius at the level of the ulnar notch and in most cases inserts broadly at the tip of the ulnar styloid process with one fascicle and at the base with another fascicle. The base of the ulnocarpal disc is located in the plane of the distal ulna. At its radial insertion, it is approximately 2 mm thick, and at the ulnar insertion, it is around 5 mm thick,160 in contrast to its thinner center, which is responsible for its biconcave form. In patients with negative ulnar variance, the ulnocarpal disc is thicker and in those with positive ulnar variance, it is thinner. The insertion segments are highly vascularized, while the much larger central and radial parts are avascular. The ulnocarpal disc is the most important part of the TFCC, with the involvement of the palmar and dorsal radioulnar ligaments.160 It primarily contributes to transferring axial compression from the hand to the ulna (“shock absorber”), extends the joint surface between the radius and the ulna, and stabilizes the ulnar side of the wrist.235 Fig. 1.9 Ulnocarpal disc in the distal view. (From THIEME Atlas of Anatomy, General Anatomy and Musculoskeletal System. 2nd ed. © Thieme 2014, illustration by Karl Wesker.) The ulnocarpal meniscus homologue consists of a synovial mucosal fold and loose connective tissue. It arises at the margin from the ulnocarpal disc or the ulnar notch and inserts obliquely at the ulnar styloid process palmarward, as well as at the palmar side of the triquetrum and hamate and the bases of the fourth and fifth metacarpals. The ulnocarpal meniscus homologue helps stabilize the ulnar wrist and the distal pisotriquetral joint. The palmar and dorsal radioulnar ligaments, the ulnolunate ligament, and the ulnotriquetral ligament are fused with the lateral side of the ulnocarpal disc. Note Since the ulnocarpal meniscus homologue also contains synovial tissue, it is vulnerable to inflammatory processes, especially in patients with rheumatoid arthritis,160 which can result in continued damage of the TFCC tissue. An inflamed dorsal synovial fold is enough to cause load-dependent pain symptoms similar to that of a disc lesion. Here, synovial villi form on the dorsal aspect of the ulnocarpal wrist joint, which causes painful impingement. The palmar radioulnar ligament arises from the palmar aspect and the dorsal radioulnar ligament originates from the dorsal aspect of the distal, ulnar and very compact portion of the radius within the joint capsule of the distal radioulnar joint. Their fibers blend together and form a type of ring that is firmly attached to the ulnar head and the ulnocarpal disc. These two ligaments are considered to be guiding ligaments and stabilizers for pronation and supination. During supination, the extensor carpi ulnaris muscle and the palmar radioulnar ligament tighten, and during pronation the dorsal radioulnar ligament tightens.229 These two ligaments are therefore important parts of the TFCC and secure all pronation and supination movements of the distal radioulnar joint ( ▶ Fig. 1.10). Fig. 1.10 Ligaments of the TFCC. Left: dorsal view; Right: palmar view. These two ligaments are considered to be stabilizing ligaments of the TFCC for the proximal radiocarpal joint. They both originate from the palmar radioulnar ligament either in isolation or together. The first stabilizing ligament (ulnolunate ligament) inserts onto the palmar horn of the lunate (there is frequently also a connection to the lunotriquetral ligament) and the second stabilizing ligament (ulnotriquetral ligament) inserts onto the palmar aspect of the triquetrum. Both ligaments contribute to stabilizing the radioulnar and radiocarpal joints. According to Taleisnik (1985)251 and De Leeuw (1962),142 this ligament is a component of the extensor retinaculum, the tendon sheath of the extensor carpi ulnaris muscle, and of the joint capsule. It contributes to stabilizing radius deviation in the proximal radiocarpal joint. During this movement, the carpal bones are displaced toward the ulnar side, and this displacement is decelerated by this ligament.109 The tendon sheath of the extensor carpi ulnaris muscle with its retinaculum of the extensor muscles is an integral component of the dorsal portion of the TFCC. It runs in a troughlike groove on the dorsal aspect of the ulnar head and, with several tendon fibers, inserts onto the triquetrum,251 pisiform, pisometacarpal ligament, and the base of the fifth metacarpal.229 Functionally, it decelerates supination in the radioulnar joint ( ▶ Fig. 1.11) and acts to stabilize radial deviation with the ulnar collateral ligament synergistically.229 Fig. 1.11 Pronation and supination declerator. Distal view. The ulnocarpal disc is not depicted. Practical Tip The TFCC is frequently the site of traumatic and degenerative processes. Most cases of traumatic disc lesions involve a tear in the disc at the ulnar insertion, in some cases combined with avulsion of the ulnar styloid process. If the distal radioulnar joint becomes unstable, arthroscopically assisted refixation is recommended. Furthermore, there will be disc perforations in the avascular zone, that is, at the radial insertion or in the center of the disc. Moreover, the ulnocarpal ligaments can tear off. Impaction syndromes often cause chronic disc lesions. In some cases, a major central lesion can be visualized arthroscopically ( ▶ Fig. 1.12). Injuries of the radioulnar ligaments always result in instability of the distal radioulnar joint. If the palmar radioulnar ligament is affected, the radius will become dislocated toward the palmar aspect, and if the dorsal radioulnar ligament is affected the radius will become dislocated toward the dorsal aspect. Ruptures of the ulnolunate and radiocarpal ulnotriquetral ligaments can promote structural disturbances of the arrangement of the carpal bones with associated degeneration.231 Fig. 1.12 Arthroscopic image of a tear of the ulnocarpal disc on the radial side. The most important muscles for pronation and supination are located in the upper arm and forearm. Pronation is carried out by the pronator teres and pronator quadratus muscles: The powerful two-headed pronator teres muscle belongs to the superficial layer of the flexors ( ▶ Fig. 1.13). With its larger head (humeral head), it originates from the medial epicondyle and from the medial intermuscular septum. With its smaller, deep-seated head (ulnar head), it originates from the coronoid process. The common insertion is located laterally in the center of the pronator tuberosity (shaft of the radius). It is covered by the brachioradialis muscle at the insertion site.60 The pronator quadratus muscle, which is square and very flat and is also located in the deep layer of the palmar flexors, courses in the area of the distal forearm bones. It originates from the margin of the ulna and inserts onto the volar surface of the radius. Functionally, it pulls the radius toward the ulna and contributes to stabilizing pronation. Note The pronator quadratus muscle is the more important pronator, since it is involved in all inward rotations, while the pronator teres muscle becomes active only during rapid movements and against resistance.256,259 To a limited extent, the flexor carpi radialis muscle, for example, is involved in pronation. Fig. 1.13 Pronator teres and supinator muscles. (From THIEME Atlas of Anatomy, General Anatomy and Musculoskeletal System. 2nd ed. © Thieme 2014, illustration by Karl Wesker.) Supination is carried out by the biceps brachii and supinator muscles: The two-headed biceps brachii muscle originates from the supraglenoid tubercle with its long head and from the coracoid process with its short head. The two heads generally unite at the level of the deltoid tuberosity. The biceps brachii muscle inserts onto the radial tuberosity with a thick tendon (in association with the bicipitoradial bursa). A second flat tendon develops into the bicipital aponeurosis (lacertus fibrosus) and radiates into the antebrachial fascia. Its supination effect increases with increasing flexion in the elbow. The supinator muscle belongs to the deep layer of extensors ( ▶ Fig. 1.13). Its shape is that of a trapezoidlike, 1-cm thick muscle plate. It originates from the olecranon of the ulna, the lateral medial epicondyle of the humerus, the radial collateral ligament and the anular ligament of the radius. The supinator muscle inserts at the radius between the radial tuberosity and the insertion of the pronator teres muscle. As an outward rotating muscle, the supinator muscle is much stronger and more important than the biceps brachii muscle, since the supinator is able to work in all positions of the arm at the same strength.256 This means that even if the biceps brachii muscle is paralyzed due to trauma, a supination movement is still possible. In the reverse scenario, however, the biceps brachii muscle is not able to take over. When the elbow is flexed at a 90° angle, the supinators are much stronger than the pronators. For this reason, it is much easier to perform actions such as turning a screwdriver if the elbow is flexed. The brachioradialis muscle is not involved in pronation or supination. It only returns the forearm to mid-position. In this position, it also serves as a flexor. As a one-headed muscle located on the surface, it originates from the lateral supra-epicondylar ridge and the lateral intermuscular septum. It inserts onto the radial surface of the radial styloid process. With the involvement of the ulnocarpal meniscus homologue, the collateral ulnar carpal ligament is considered to be one of the decelerators of radial deviation of the wrist.106 The TFCC is therefore a key factor for the inclusion of the distal radioulnar joint in the function of the wrist joint. The wrist joint is thus composed of the radiocarpal joint, the midcarpal joint and the carpometacarpal joint (as a bridge to the carpal bones22), in cooperation with the distal radioulnar joint. Hand movements take place as follows256: The rotation movements pronation and supination are carried out in the proximal and distal radioulnar joint in cooperation with the shoulder joint ( ▶ Fig. 1.14). The wrist joint is not involved in these movements and is more or less carried along. However, the selective movements in the plane of the hand and the marginal movements are controlled by the wrist joint alone. Movements in the plane of the hand include extension (bending the back of the hand toward the forearm) and flexion (bending the palm toward the forearm). Marginal movements include radial deviation (moving the hand toward the thumb) and ulnar deviation (moving the hand toward the little finger). Circumduction ( ▶ Fig. 1.15) is a combination of the two degrees of freedom: 1) extension and flexion; and 2) radial and ulnar deviation. This circling movement of the wrist can be supported by pronation and supination to some extent. Pure rotation movements are only passively possible.149 Fig. 1.14 Movement axes of the wrist joint. Fig. 1.15 Circumduction of the hand (circling the wrist). In functional terms, the wrist is considered to be a single joint. Morphologically, however, it consists of two separate joints: the proximal and the distal wrist joints. These two joints have two degrees of freedom and are composed of eight carpal bones (seven “regular” bones and one sesamoid bone; ▶ Fig. 1.16). The proximal row contains the scaphoid, lunate, triquetrum, and pisiform, while the distal row contains the trapezium, trapezoid, capitate, and hamate. In the section below, the characteristics of the individual carpal bones are discussed. Fig. 1.16 Carpal bones. (a) Right hand and palm in the palmar view. (b) Right hand and palm in the dorsal view. The scaphoid is around 16 mm long and around 28 mm wide,215 making it the largest of the four proximal carpal bones. It is somewhat curved toward the distal and ulnar aspect. One-quarter of the total area has no cartilage and serves as the entry portal for various vessels229—that is, the area of insertion of the radial collateral ligament and the tubercle of the scaphoid.160 The flexor retinaculum, palmar radioulnar ligaments, and abductor pollicis brevis muscle insert onto this tubercle, whose palmar distal aspect is somewhat radially oriented. It is located below the tendon of the flexor carpi radialis muscle and serves it as a hypomochlion.229 With its convex joint surfaces, the scaphoid has contact to the radius, the trapezium, and the trapezoid. It has contact to the capitate with its concave surface and to the lunate with its flat surface. According to Linscheid (1986),148 this bone located on the radial side is not actually part of the proximal carpal row but rather serves to connect the proximal and distal carpal rows. Practical Tip Pseudarthrosis is a post-traumatic pathological condition involving an unstable scaphoid fracture. The instability can result from a proximal fracture or a humpback deformity or it can occur if the fracture gap is more than 1 mm wide. It is the result of inadequate fracture healing with the formation of connective tissue in the fracture gap.15 This leads to a false joint, which allows movement between the bone fragments and in turn leads to tilting. This malalignment leads to progressive arthrosis, which successively affects various joint segments, culminating in scaphoid nonunion advanced collapse (SNAC). The condition is classified by stage: Stage 1: Arthrosis of the styloid process due to palmar malalignment of the distal scaphoid fragment Stage 2: Extension to the joint surface between the distal fragment and the radius Stage 3: Additional midcarpal arthrosis (between the lunate and capitate) due to dorsal positioning of the lunate and proximal positioning of the capitate. If the retrograde blood flow to the scaphoid is disrupted in a proximal fracture, this frequently results in osteonecrosis of the proximal pole. This carpal bone is wedge-shaped, with the dorsal surface smaller than the palmar surface. The lunate is around 19 mm long, around 18 mm wide, and around 13 mm thick.215 It is located in the center of the proximal wrist joint and articulates equally in the wrist joint abutting the radius with a convex joint surface and in the midcarpal joint abutting the capitate with a concave surface. Two flat articular facets of the bone also articulate with the triquetrum and scaphoid. Sixty-five percent of individuals have an additional fifth medial facet that articulates with the hamate.155 Among the few vessels supplying the lunate, the proximal portion of the joint surface is the most poorly vascularized. This plays a particularly important role for the wrist, since it is involved in all movements, both longitudinally and transversally.229 In these movements, it controls flexion with the radius and, in conjunction with the radius and the scaphoid, all other functions.242 Additional Information In 44% of the individuals studied with a joint between the lunate and hamate, chondromalacia was found in this fifth medial facet.155 In addition to a negative ulnar variance involving an articular connection between the lunate and hamate,110,117 venous congestion in the lunate may cause lunate necrosis. The circulatory disorder may be triggered by overextension of the wrist and simultaneous increased pressure by the flexor tendons, increased capsule tension, and compression of the lunate by the radial margin and of the hamate. One of the suspected causes continues to be microtrauma of the hand. The triquetrum is the ulnar part of the radiocarpal bones. It is around 14 mm long and around 19 mm wide.215 It articulates with the ulnocarpal complex with a proximal convex joint surface and articulates with the lunate with a facet that is smooth on the proximal and radial aspect, with a noncartilaginous ulnar dorsal facet for insertion of the ulnar collateral ligament of the wrist joint, and it articulates the hamate with a spiral-shaped ulnar distal facet. Although it is not actually a sellar joint, the ulnar distal facet has a convex and a concave segment, which enables spiral movement during ulnar deviation.160 Moreover, on the palmar aspect there is a slightly concave-shaped joint surface on which the pisiform lies.229 The radial surface of this bone forms the ulnar part of the ulnar canal, which allows passage of the ulnar nerve through the wrist joint. The pisiform as a sesamoid bone inserts into the triquetrum with a flat facet. A sesamoid bone is a circumscribed ossification of a tendon caused by pressure or friction.160 The pisiform is firmly integrated into the tendon of the flexor carpi ulnaris muscle and its carpal continuations of the pisohamate and pisometacarpal ligaments.229 The extensor and flexor retinaculum, the tendon from which the abductor digiti minimi muscle originates, and distal continuations of the meniscal homologue also insert at the pisiform. Together these structures exert a stabilizing influence toward the distal aspect of the wrist. The pisiform therefore resembles the hub of a wheel from which the fibrous attachments extend in all directions like spokes holding the bone in place on the triquetrum yet allowing it to move.186 Navarro (1935)177described these two carpal bones as functionally counteracting the scaphoid. The trapezium is around 17 mm long and around 24 mm wide.215 As the first carpal bone of the distal wrist, it is located behind the scaphoid. The palmar, radial, and dorsal aspects of the bone are rough and free of cartilage.229 At the level of the scaphoid tubercle, this bone has on its palmar aspect a tubercle and a groove containing the flexor carpi radialis muscle. The radial collateral carpal ligament of the wrist inserts onto the radial aspect. The trapezium can be clearly recognized owing to the concave and convex saddle-like joint surface on the radiodistal aspect. It articulates with an oppositely rotating curved surface of the first metacarpal. The carpometacarpal joint of the thumb is firmly integrated in the wrist and is one of the most important joints, since it is the opposition of the thumb that enables the wide range of hand movements possible in the first place. The adjacent ulnodistal aspect of the trapezium is firmly attached to the second metacarpal with a flat square facet. Proximally, the concave surface articulates with the scaphoid. Medially, this carpal bone faces the trapezoid with its second-largest, slightly concave160 and spiral surface.229 After the pisiform as a sesamoid bone, the trapezoid is the smallest carpal bone. It is around 12 mm long and around 17 mm wide. This bone articulates a convex and concave facet distally with the second metacarpal. In 34% of cases, it also articulates with the third metacarpal.50 The ulnar facet articulating with the capitate is slightly concave to irregularly shaped, while the radial aspect articulating with the trapezium is flat to slightly convex; the proximal aspect articulating with the scaphoid has a slightly concave shape. Owing to it its wedgelike shape, it is the least mobile carpal bone. The capitate is the largest carpal bone. It is around 24 mm long and around 16 mm wide.215 Proximally, its convex head fits into the concave surface of the scaphoid and lunate. Distally, it articulates with the third metacarpal with a nearly flat surface. The distal radial aspect has a slightly concave facet to the second metacarpal and a convex surface to the trapezoid. On the distal ulnar aspect there are two flat facets to the fourth metacarpal and on its side to the hamate. All of the joint surfaces are fully covered with cartilage. This carpal has the shape of a pyramid. It is around 21 mm long and around 16 mm wide.215 Its base is directed toward the metacarpals and its apex is directed toward the lunate. On the palmar aspect in the distal area, the hook of hamate is located, with its concave curve toward the radial aspect. Proximally, there may be a convex facet to the lunate on the radial aspect (in 65% of cases155), and on the ulnar aspect there is a screw-shaped articular surface that articulates with the triquetrum. Distally, there are two more joint surfaces toward the fourth and fifth metacarpals, respectively. In the proximal radiocarpal joint, these carpal bones form an ovoid or ellipsoid joint ( ▶ Fig. 1.17) and in the distal radiocarpal joint a more or less functional ball-and-socket joint.136,137 Furthermore, all of the carpal bones form flexible, amphiarthrotic connections to each other, namely the carpal joints.229 Fig. 1.17 Wrist joint, ellipsoid joint. (a) Proximal wrist joint, two-axis ellipsoid joint. (b) Distal wrist joint, proximal joint surface. The proximal wrist joint connects the hand to the two bones of the forearm, the radius and the ulna, with involvement of the ulnocarpal disc ( ▶ Fig. 1.18). The two bones together form the proximal biconcave socket, in the first place, from the bifaceted radial surface (scaphoid and lunate facets) and, in the second place, from the concave surface of the ulnocarpal disc (ulnar notch233). Three-quarters of this surface corresponds to the radius and one-quarter to the ulna.233 The angle of deviation of the radius in the sagittal plane can amount to as much as 20°,58 and the dorsopalmar angle of deviation can amount to as much as 15° ( ▶ Fig. 1.19).229 While deviations contribute to deceleration of flexion and ulnar deviation by the bones, they can also promote dislocation in both directions. Fig. 1.18 Proximal wrist joint. (From THIEME Atlas of Anatomy, General Anatomy and Musculoskeletal System. 2nd ed. © Thieme 2014, illustration by Karl Wesker.) Fig. 1.19 Radial deviation (From Hochschild J. Functional Anatomy for Physical Therapists. Stuttgart: Thieme; 2016.) The distal ovoid convex joint head is formed by the scaphoid, lunate, and triquetrum and is covered with hyaline cartilage. These bones are held together by short ligaments (scapholunate and lunotriquetral ligaments), which are fully enclosed by these carpal bones and therefore give the false impression that the cartilage covering is uniform.272 The pisiform is not involved in the actual arthrokinematics but rather serves as a sort of sesamoid bone that stabilizes the joint by means of ligaments and muscles. Between the two articulating joint surfaces, there is thus an incongruity because the convex joint head (in the shape of a curved arch) is much larger than the socket (approx. 1:1.5 in the radioulnar direction222 and approx. 1:2 in the dorsopalmar direction91). The scaphoid abuts the lower end of the radius while the lunate partially abuts both the radius and the ulnocarpal disc. The triquetrum is in contact with the ulnar collateral ligament of the wrist joint on the ulnar side beyond the ulnocarpal disc.256 About 48 to 50% of compressive stresses transferred when the wrist joint is in neutral zero position occur by means of the scaphoid fossa, 35 to 40% through the lunate fossa, and 12 to 15% through the ulnocarpal disc.72,82,229 It is therefore understandable that during trauma with the arm extended, the delicate ulna is less often damaged than the much more robust radius.256 The end of the proximal radiocarpal joint is formed by a relatively wide, thin capsule secured by a strong ligament system. The range of motion of this joint is always measured taking the midcarpal joint into account, since the two joints are in a direct reciprocal relationship.229 This results in extension of around 80°, flexion of around 80°, radial deviation of around 15 to 25°, and ulnar deviation of around 40 to 50°.229 Over the course of evolution, the carpus lost contact to the ulnar styloid process, which enabled the hand to have a stable torsional movement.169 The distal wrist is formed from the proximal and distal row of the carpal bones ( ▶ Fig. 1.20). In contrast to the arc-shaped proximal wrist, the distal carpal row (i.e., compared to the proximal row) runs in a straighter, undular direction (S-shaped). The scaphoid begins radially with a convex curvature, across from which a socket formed by the trapezium and trapezoid is located. Toward the ulnar aspect, the capitate and hamate protrude against it, similar to a joint head. Both bones are embedded in the socket formed by the scaphoid, lunate, and triquetrum.229 Forty-six percent of all individuals have additional joint surfaces in the proximal hamate and in the distal lunate. These additional joint surfaces can trigger degenerative processes.266 This arch leads to a certain interlocking of the two carpal rows256 with a narrow intra-articular space.22 With the involvement of stable ligament connections, this creates more limited mobility compared with the proximal radiocarpal joint (with the exception of dorsal extension of 50% due to the very mobile lunate106). This stability of the distal carpal row also impacts the palm (which is a functionally rigid unit) and helps stabilize the palmar arch. Fig. 1.20 Distal wrist joint. (From THIEME Atlas of Anatomy, General Anatomy and Musculoskeletal System. 2nd ed. © Thieme 2014, illustration by Karl Wesker.) The individual carpal bones are flexibly interconnected (amphiarthroses). Owing to the different bony formations and the rigid interosseous ligament connections, functional range of motion is limited. The respective joint capsules are stabilized by the small interosseous ligaments. The greatest mobility occurs in the proximal row between the lunate and scaphoid in the form of rotation movements. Between the triquetrum and pisiform, there is also an independent intercarpal joint with a thin rigid capsule. In terms of function, the triquetrum is centered, stabilized and also guided by the pisiform229 and counteracts the pulling action of the flexor carpi ulnaris muscle.60 With the involvement of fibers of the extensor carpi ulnaris muscle and the extensor retinaculum running palmarward,229 this results in a nearly extra-articular spin132 that contributes to the rotational stability of the wrist.229 It also counteracts palmar dislocation of the wrist and is involved in the formation of the ulnar canal (allows passage of the ulnar nerve).38 The second to fifth carpometacarpal (CMC) joints connect the distal carpus and the bases of the metacarpals, thus connecting the carpus with the metacarpus ( ▶ Fig. 1.21). The carpal articular surfaces are slightly convex and the bases of the metacarpals are concave.135 Parts of the bases of the second to fifth metacarpals are positioned on the carpal bones in a conical fashion.229 The second metacarpal interlocks with the trapezoid bone with the involvement of the trapezium and capitate. In a similar fashion, the third metacarpal juts into the space between the trapezoid and capitate with its styloid process in a conical manner. The second and third metacarpals therefore form a firm bony connection with the opposing carpal bones. The fourth and fifth metacarpals abut the hamate together. A Y-shaped ligament of the third metacarpal (attached to the capitate and hamate), as well as the palmar and dorsal carpometacarpal ligaments, demonstrate the close connection between the carpus and the metacarpals, the so-called amphiarthroses with only limited mobility.229 The greatest range of motion occurs in the fourth and fifth CMC joints, in particular in the fifth CMC joint, whose joint surface has a sellar shape in 60% of people.229 Functionally, however, the only possible movement is flexion, which supports the opposition of the little finger toward the thumb. Fig. 1.21 Second to fifth CMC joints and intermetacarpal joints. The entire carpus is a concave structure and forms the shape of a palmar arch, namely the carpal tunnel (space for the tendons of the hand and the median nerve). The carpus is stabilized by several muscles and, in particular, by its complex ligament system. There are 33 different ligament structures in the carpal area,24 most of which are firmly attached to the joint capsule (capsular stabilizers). The aspects facing the joints are covered by a synovial membrane, while the lateral aspects have a fibrous layer.160 During dissection, it is nearly impossible to expose all the ligaments separately.229 The distal part of the ligament structure is much stronger than the ulnar part, which is evident reciprocally in terms of mobility. This is also true for the stronger palmar ligaments compared to the weaker dorsal ligaments, which have more densely packed collagen fibers.160 The axial compression on the carpus and the oblique joint surface between the radius and the proximal carpal row (i.e., dorsal and distal to palmar and proximal) tend to translate the carpus in a palmar direction. The palmar ligaments are therefore subjected to higher load and must therefore be more stable.160 The oblique course of the joint surface (i.e., from radial and distal to ulnar and proximal) and the axial compression cause the carpal bones to deviate ulnarward. For this reason, an additional ligament system extends from radial and proximal to ulnar and distal, and therefore compensates for this translatoric process.160 Each carpal bone is in contact with another carpal bone, more or less directly or indirectly.160 The carpal ligament system is assigned the tasks of stabilizing the wrist as well as inhibiting and limiting extreme movements.256 Lichtman et al (1981)146 and Fisk (1984)63 described this complex carpal region as a dynamic ring system of carpal bones that is under constant tension. These bones must be held together tightly by ligaments,229 which are also important components of proprioception of the wrist.160 The ligaments of the hand are arranged in three dorsal and three palmar layers.109 Schmidt and Lanz (2003)229 classified this ligament system into superficial, middle, and deep layers (three-layer structure200). The superficial layer consists of the flexor retinaculum and the extensor retinaculum. The retinacula are responsible for positioning and guiding the tendons.229 In addition, the flexor retinaculum centers the pisiform on the triquetrum and in so doing prevents it from slipping ulnarward.229 The extensor retinaculum contributes to the carpal stability. Proximal to the palmar carpal region, the antebrachial fascia is continuous with the superficial (palmar carpal ligament) and deep stabilizing ligaments of the flexor retinaculum.229 The palmar carpal ligament spans between the tendon of the flexor carpi ulnaris muscle and the tendon of the palmaris longus muscle. The radial aspect of the latter muscle is attached to the flexor retinaculum ( ▶ Fig. 1.22). Fig. 1.22 Flexor retinaculum. (From THIEME Atlas of Anatomy, General Anatomy and Musculoskeletal System. 2nd ed. © Thieme 2014, illustration by Karl Wesker.) The flexor retinaculum spans between the ulnar (pisiform and hook of hamate) and the radial eminences of the wrist (tubercle of trapezium and tubercle of scaphoid) and forms the roof of the carpal tunnel.200 The fibers of the retinaculum resemble a woven structure and are firmly fused.87 Schmidt and Lanz (2003)229 described this rigid ligament system as an important component of the finger flexor pulley system. The ligament also prevents bowstringing during wrist flexion.179,180 However, it does not appear to have a great influence on the stability of the wrist joint, since dissecting the flexor retinaculum has little impact on carpal stability.229 Additional Information Several segments of the distal portion of the retinaculum form an aponeurosis that is positioned between the thenar and hypothenar muscles.160 Changes in the tension of the flexor retinaculum and its attachment to the thenar muscles may be responsible for reducing the range of motion of the thumb during wrist extension. However, an important task of these fibers involves transmitting proprioceptive information of the wrist.158 The extensor retinaculum arises together with the palmar carpal ligament from the deep fibrous layers of the antebrachial fascia and radiates into the dorsal fascia of the hand without any sharp delineation ( ▶ Fig. 1.23). Proximally, it is around 51 mm long on average and distally around 54 mm. On the radial side, it is around 15 mm wide, in the center around 26 mm, and on the ulnar side around 20 mm.227 It is divided into superficial supratendinous and deep infratendinous layers250: The supratendinous layer arises from the palmar antebrachial fascia with the inclusion of the palmar carpal ligament, the tendon of the flexor carpi radialis muscle, the radial styloid process, and the thenar fascia. The fibers on the ulnar side extend across the tendon of the extensor carpi ulnaris muscle and ultimately radiate into the antebrachial fascia. There are additional insertions at the triquetrum and pisiform, and distally into the fascia of the hypothenar muscles.229 The infratendinous layer is thin and short and occurs only in the area of the fourth and fifth extensor tendon compartments. This layer is fused to the joint capsule of the distal radioulnar joint, extends below the sixth extensor tendon compartment, and inserts together with the joint capsule of the wrist and the superficial layer onto the palmar surface of the triquetrum.229 Fig. 1.23 Extensor retinaculum. (From THIEME Atlas of Anatomy, General Anatomy and Musculoskeletal System. 2nd ed. © Thieme 2014, illustration by Karl Wesker.) As a result, the extensor retinaculum stabilizes the extensor carpi ulnaris muscle without direct contact with the ulna. The mobility of the bone during pronation and supination is therefore not affected.160 The extensor retinaculum is responsible for forming six vertically positioned connective tissue septa that are fused to the periosteum at the radius, the capsule of the carpal and radioulnar joints, and the TFCC.229 The ensuing six osteofibrous tendon compartments serve to provide passage for the extensor tendons of the thumb, wrist, and fingers. The extensor retinaculum prevents bowstringing and extensive radial and ulnar lateral slipping of the extensor tendons,188 and supports the TFCC.229 This layer comprises the radial collateral carpal ligament of the wrist, various palmar and dorsal radiocarpal ligaments, the TFCC, and the dorsal intercarpal ligament. The palmar ligaments are thicker than the dorsal ligaments.231 These ligaments limit and stabilize radial and ulnar deviation, as well as extension and, in particular, flexion. They also play a key role in physiological pressure distribution in the carpus. The middle layer is composed of three groups of ligaments. This ligament is actually more part of the palmar ligament apparatus than the radial ligament system.251 It arises from the palmar border of the radial styloid process and extends in an oblique direction across the carpal articular space toward the scaphoid tubercle and toward the sheath wall of the tendon of the flexor carpi radialis muscle229 up to the trapezium.78 One of the ligament’s important functions involves the transmission of proprioceptive stimuli from the ligament’s area of origin and insertion.193 These ligaments run in a thin, superficial layer above a strong, thick, deep intracapsular fibrous layer.229 The superficial parts of the ligaments arise from the palmar surface of the radial styloid process and insert at the capitate and lunate. The deep parts arise together from the radial styloid process, or broad-based from the volar lip of the radius, and are divided into three fibrous tracts: the radioscaphocapitate ligament, and the long and short radiolunate ligaments. The radioscaphocapitate ligament runs across the waist of the scaphoid and spans the distal wrist160 with an insertion at the capitate, while at the ulnar side of this ligament, the long and short radiolunate ligaments run in a flat and somewhat oblique direction toward the lunate.229 Together with the scaphotrapezoid ligament and the arcuate ligament (triquetrocapitoscaphoid ligament), the radioscaphocapitate ligament forms the distal palmar V-shaped ligament (V ligament). The long and short radiolunate ligaments, together with the ulnolunate ligament and the ulnotriquetral ligaments, form the proximal palmar V-shaped ligament.231 Radioscaphocapitate ligament This ligament primarily serves to stabilize the joint between the lunate and capitate.147 It can be stretched by around 30%.150 The ligament becomes stretched during ulnar deviation and during extension with radial deviation of the distal carpal row—which is what enables extension across two joints in the first place.162 Furthermore, during radial deviation, the ligament controls palmar flexion of the scaphoid, which is associated with extension of the capitate.160 It also works together with the long radiolunate ligament to stabilize the proximal pole of the scaphoid.17 Note If the proximal half of the scaphoid is fractured, the radioscaphocapitate ligament can fold into the fracture gap and lead to scaphoid pseudarthrosis.231 Arcuate ligament The ulnar side of the distal group of V-shaped ligaments is formed by a ligament with an arching course (“deltoid ligament”231). The arcuate ligament (TCSL: triquetrocapitoscaphoid or radiate ligament, deltoid ligament154) arises on the palmar aspect of the triquetrum, extends in a bow shape over the tip of the hamate, and terminates on the palmar side of the distal third of the scaphoid.231 As a fairly loose ligamentary connection, the arcuate ligament permits the triquetrum to slide over the spiral-shaped joint surface of the hamate, which is responsible for the high and low triquetral positions during radial and ulnar deviation.231 Tighter sections of the ligament prevent flexion of the proximal carpal row. In many cases, the central fibers to the lunate are absent, which creates a weak point in the wrist (the space of Poirier161,229). Scaphotrapeziotrapezoid ligament In a wider sense of the term, the scaphotrapeziotrapezoid ligament also belongs to the ligaments of the “distal V”231 and the deep layer of the ligament system.160 This V-shaped ligament connects the scaphoid with the trapezium and the trapezoid.160 Function of the palmar “distal V” The main function of this palmar ligament complex is to hold the scaphoid in place like a hypomochlion, and to fixate and stabilize the capitate.231 The radiocarpal ligaments also include the long and short radiolunate ligaments. Together with the ulnolunate and ulnotriquetral ligaments, they form the palmar “proximal V” ( ▶ Fig. 1.24). Fig. 1.24 Carpal ligament structures in the palmar view. Red = palmar V-shaped ligaments. (From THIEME Atlas of Anatomy, General Anatomy and Musculoskeletal System. 2nd ed. © Thieme 2014, illustration by Karl Wesker.) Radiolunotriquetral ligament (long and short radiolunate ligaments) The long part of the radiolunate ligaments tightens during radial and ulnar deviation160 and is able to be stretched by approximately 30%.150 Since it courses across the distal pole of the scaphoid, it may control palmar flexion of the scaphoid during radial deviation.160 In contrast, the short radiolunate ligament can stretch by around 47% and during flexion, by around 55%.216 The long radiolunate ligament courses first to the lunate and continues to the triquetrum, therefore corresponding to the radiolunotriquetral ligament.231 Together, they form the radiopalmar leg of the proximal V and are considered to be the wrist’s strongest radiocarpal ligaments.160 These ligaments perform the important function of preventing the carpus from slipping along the joint surface of the radius, which has a 25° angle of inclination to the ulnar aspect.231 Because of their alignment with the ulnar inclination of the radial joint surface and their function of keeping the carpus in a stable position, the radiolunotriquetral and dorsal radiotriquetral ligaments are also known as the “extra-articular slingshot.”231 Ulnolunate ligament and ulnotriquetral ligament The ulnar leg of the proximal V consists of the palmar ligamentary structures of the triangular fibrocartilage complex (TFCC), that is, the ulnolunate and the ulnotriquetral ligaments. They originate on the palmar radioulnar ligament and proceed to the anterior horn of the lunate and/or to a depression on the palmar side of the triquetrum.231 The two ligaments are key components of the TFCC and are important stabilizers of the distal part of the carpus and prevent nondissociative forms of instability. Function of the palmar “proximal V” ligament The function of the proximal V-shaped ligament ( ▶ Fig. 1.24) involves the longitudinal transference of force between the ulna and the carpus and fixation of the proximal carpal row, especially the lunate as the most important intermediate element of movement (“intercalated segment”).231 One of the dorsal radiocarpal ligaments is the radiotriquetral ligament located on the dorsal aspect. Together with the dorsal intercarpal ligament, it forms the dorsal V-shaped ligaments ( ▶ Fig. 1.25). While the two ligaments are stabilized by the joint capsule, they are weaker than the palmar ligaments.231 Fig. 1.25 Carpal ligament structures in the dorsal view. Red = dorsal V-shaped ligaments. (From THIEME Atlas of Anatomy, General Anatomy and Musculoskeletal System. 2nd ed. © Thieme 2014, illustration by Karl Wesker.) Dorsal radiotriquetral ligament The dorsal radiotriquetral ligament arises from the dorsal border of the radius, immediately distal to Lister’s tubercle (dorsal tubercle160). Its course crosses the proximal scaphoid pole and the posterior horn of the lunate and ultimately inserts onto the dorsal aspect of the triquetrum.231 The ligament is about 20 mm long; proximally it is 5 mm wide and distally around 5 mm wide.265 Dorsal intercarpal ligament This ligament originates at the dorsal side of the triquetrum and after taking a horizontal course, inserts with one fascicle on the back of the scaphoid and with another fascicle on the back of the trapezium and at the radial collateral carpal ligament.231 It is approximately 36 mm long and 6 mm wide.265 Function of the “dorsal V” ligament Since both dorsal ligaments cover the middle carpal column, the lunate is stabilized by the dorsal radiotriquetral ligament and the capitate is stabilized by the dorsal intercarpal ligaments, which hold the two bones in colinear alignment.231 Neither flexion nor extension is compromised.160 In synergy with the radiolunotriquetral ligament on the palmar side, the dorsal V-shaped ligament prevent the carpus from sliding along the radial joint surface, which slopes to the ulnar side.231 In terms of function, it resembles an accordion, viz. during extension, the dorsal V becomes narrower, and during flexion it becomes wider.160 This configuration permits extensive movement while ensuring stability at the same time, since the ligaments hardly need to become longer.160 As one of the “slingshot” ligaments it is therefore among the most important carpal structures providing stability.231 Summary All in all, the V-shaped ligaments provide the functional connection between all pillars of carpal kinematic function. The distal V-shaped ligament stabilizes the capitate and decelerates the scaphoid, while the proximal V-shaped ligament helps to regulate the proximal transfer of force between the ulna and the carpus and stabilizes the proximal carpal row, with the lunate as the intermediate element of movement.231 The dorsal V-shaped ligament and the ulnotriquetral ligament on the palmar side (part of the TFCC) prevent the carpus from sliding along the radial joint surface, which slopes to the ulnar side (“slingshot ligaments”).231 The dorsal V ligament also stabilizes the lunate and the capitate and holds them in colinear alignment, since their fascicles span the middle carpal column.231 These V-shaped ligaments function as key decelerators of wrist movement, especially for radial and ulnar deviation and, with the involvement of intermediate ligaments, for extension and flexion. Moreover, they coordinate and center individual carpal bones and thus contribute to physiological transfer of force. The palmar V- and the dorsal V-shaped ligaments work in synergy to stabilize radial and ulnar deviation, with individual ligaments alternating as agonists and antagonists.233 During ulnar deviation, the radioscaphocapitate, radiolunotriquetral, and dorsal radiotriquetral ligaments tighten and the ulnolunate, ulnotriquetral, arcuate, and dorsal intercarpal ligaments relax. The opposite is true for radial deviation.233 During extension, the palmar ligaments between the radius and the triquetrum, pisiform as well as hamate and the dorsal ligaments between the hamate and the triquetrum are subjected to tension, while the dorsal ligaments relax the dorsal connections of the radius and ulna with the triquetrum. The opposite is true for flexion.91 Note Ruptures of the proximal palmar V-shaped ligament can therefore promote dorsiflexed intercalated segment instability (DISI) and ruptures of the distal V-shaped ligament can promote rotational malalignment of the scaphoid. A tear in the dorsal V predisposes to ulnar translocation.231 The TFCC is separated into the following components: the ulnocarpal disc, the palmar and dorsal radioulnar ligaments, the ulnolunate ligament, the ulnotriquetral ligament, the palmar and dorsal ulnocarpal ligaments, the ulnar collateral ligament of the wrist joint, and the tendon sheath of the extensor carpi ulnaris muscle. As described above, as the key element of stabilization for the distal radioulnar joint and the wrist, the TFCC serves to regulate pressure in the carpus and operates as an important decelerator of radial deviation. The course of these ligaments is from the triquetrum to the scaphoid. They are involved in the formation of the dorsal V-shaped ligament (see section on “Dorsal V Ligament”). The structure of the radiate carpal ligament varies among individuals.229 It usually has fibers that fan out from the capitate to the triquetrum, lunate, and scaphoid. However, frequently the central fibers to the lunate are absent, which creates a weak point for this carpal bone (the space of Poirier161; ▶ Fig. 1.26). Fig. 1.26 TFCC from the dorsal view (left) and the palmar view (right). Red = space of Poirier. The palmar, dorsal, and interosseous intercarpal ligaments efficiently connect the carpal bones into a functional unit ( ▶ Fig. 1.27). Some of these ligaments are aligned toward each other on both sides and between the skeletal elements (e.g., palmar, dorsal, and interosseous trapeziotrapezoid ligaments). These small ligaments have a membranous attachment to the articular cartilage and some cross the cartilage and insert directly onto the bone as Sharpey’s fibers.231 The fibers take a longitudinal course between the radius and the scaphoid and lunate or run transversely between the two carpal rows.231 The ligaments described below are particularly important. Fig. 1.27 Deep ligaments of the wrist joint. These ligaments connect the trapezium with the trapezoid and the trapezoid with the capitate. The superficial and middle parts of the ligament are connected and provide only a minimum of freedom of movement between these carpal bones.160 The greatest range of motion of the distal carpal bones occurs between the hamate and the capitate. There is a maximum displacement of 9°.210 The ligament decelerates the slight co-movement between the capitate and the hamate during the movements of the wrist, thus permitting homogeneous interaction of the proximal and distal wrist.210 Note The strong, short trapeziotrapezoid, trapezoidocapitate, and hamatocapitate ligaments consolidate the distal carpal row into a more or less uniform structure160 and contribute to mobility of the proximal carpal bones. The lunotriquetral ligament connects the lunate and triquetrum, allowing the triquetrum to be displaced from proximal to distal during ulnar deviation.267 Its stability is reinforced by interosseous fibrocartilage.229 The scapholunate ligament establishes the functional unit between the scaphoid and the lunate. It is one of the most important mechanical components in the carpus. It permits gliding and torsional movements of the two bones against each other. At the same time, the joint surfaces allow functional interaction between the proximal and distal wrist ( ▶ Fig. 1.28). This enables the important homogeneous movements between extension and flexion and, in particular, radial and ulnar deviation. This very strong ligament consists of short dorsal fiber bundles, medium-to-long obliquely oriented bundles, and long palmar bundles. The dorsal bundles are stronger and thicker than the palmar bundles (ratio of 3:1 mm).16 Fig. 1.28 Scapholunate and lunotriquetral ligaments. Practical Tip Their lesser thickness may be why injury to the palmar ligaments is more common than to the dorsal ligaments (scaphoid dislocation) or complete ligamentous injuries (dorsiflexed intercalated segment instability (DISI) position40).258 In addition to trauma, carpal ganglia may also trigger this type of injury.258 This pathology always leads to degenerative arthrosis of the wrist, and can even result in carpal collapse, or scapholunate advanced collapse of the wrist (SLAC wrist).269 The condition is classified by stage: Stage 1: Flexion position of the scaphoid with arthritis between the proximal pole and the scaphoid fossa Stage 2: Extension to the entire scaphoid facet of the radius Stage 3: Additional mediocarpal arthrosis (between the lunate and capitate) due to dorsal position of the lunate and proximal position of the capitate This type of injury occurs more often than is commonly assumed.22 Wrist arthroscopy of 183 radius fractures confirmed scapholunate dissociation in 10.4% of cases ( ▶ Fig. 1.29).241 Fig. 1.29 Typical scapholunate dissociation with signet ring sign of the scaphoid. The strong scaphotrapezial ligament allows the trapezium (and, to some extent, also the trapezoid) to glide on the distal surface of the scaphoid and permits the scaphoid to take a position flexed palmarward during radial deviation.41 This ligament runs from the radius and inserts at the scaphoid and lunate and the interosseous scapholunate ligament, stabilizing the two bones during extension and radial deviation. The ligament is highly vascularized and contains terminal branches of the anterior antebrachial interosseous nerve18 and may be involved in proprioception of the hand.229 In summary, the 33 ligaments of the hand coordinate all complex displacements of the individual carpal bones and provide the stability needed for the wide range of possible movements ( ▶ Fig. 1.30). Stability and complex movement patterns at the carpus are possible only if the carpal ligaments are intact.231 Fig. 1.30 Structure of the carpal ligament systems. (Based on Schmidt HM, Lanz U. Surgical Anatomy of the Hand. Stuttgart: Thieme; 2003 and Schmitt R, Lanz U, eds. Bildgebende Diagnostik der Hand. 2nd ed. Stuttgart: Thieme; 2004.) Practical Tip A genetically predisposed loose ligament system or trauma-induced ligament injury can cause structural damage between the carpal bones (“snap phenomenon” as described in Ref. 229). This results in the lack of congruency and premature degenerative processes in the carpus.143 Many post-traumatic pathological ligament-related conditions are overlooked during clinical examination and conventional radiographic diagnostics. Lack of treatment usually leads to static instability of the carpus, culminating in arthrosis.231 For this reason, injuries to the scapholunate, lunotriquetral, and radioscaphocapitate ligaments, as well as to the TFCC, play an important role in diagnostics. They require the examiner to be well-versed in anatomical circumstances, to understand biomechanical processes, to have a great deal of sensitivity for conservative tests with respect to specific symptoms, and to be able to handle the wide range of options for diagnostic imaging. In contrast to radial and ulnar deviation of the hand, extension and flexion are largely stabilized by the ligamentary structures. The proximal and distal wrist is always involved in extension and flexion to various degrees. This is because, in the normal position of the hand, the cartilage of the joint head in the radiocarpal joint extends beyond the socket, especially palmarward, and in the midcarpal joint extends more dorsalward. For this reason, flexion occurs for the most part in the radiocarpal joint, while extension occurs for the most part in the midcarpal joint.135 According to Kummer (2005)135 during radial and ulnar deviation of the hand, the muscles also play a key role with respect to stability, pressure regulation, and kinematics of the wrist. During radial deviation, all of the radial muscles have extension or flexion components. Therefore, during pure radial deviation, the flexion components must neutralize each other. Thus the typical combination would involve the interaction of the flexor carpi radialis muscle with the long and short extensor carpi radialis muscles. Furthermore, all muscles whose long tendons are located radial to the radial–ulnar deviation axis (e.g., the long thumb muscles) can participate in radial deviation. During ulnar deviation too, only muscle combinations in which the flexion components neutralize each other are possible. This condition is primarily met when the extensor and flexor carpi ulnaris muscles contract simultaneously. In addition, the long flexors and extensors of the fingers are involved in a limited ulnar deviation component. In supination, the antebrachial muscles take a proximal to distal course in a nearly conical form, while in pronation, the course is circular, owing to the fact that the radius crosses over the ulna. The muscle bellies of the flexors, which are thicker and stronger than the extensors, are located more in the proximal area of the forearm. As a result of this position, long tendons are formed up to the carpus or up to the distal interphalangeal (DIP) joints, which has the effect of a drive belt. Owing to the tight space of the forearm, the muscles arise from bony parts, from the antebrachial interosseous membrane or from a part of the antebrachial fascia. It is this arrangement that permits the delicate design with all of the possibilities for fine motor movement of the wrist and the finger joints.256 The carpal muscles are divided into two groups: those involved in flexion and ulnar deviation, and those involved in extension and radial deviation as well as joint rotation. The most important muscles involved in flexing the wrist are the flexor carpi ulnaris and flexor carpi radialis, along with the palmaris longus muscle. The muscle primarily responsible for ulnar deviation is the extensor carpi ulnaris, with the involvement of the flexor carpi ulnaris and the extensor digitorum communis muscles. Some of the finger flexor muscles are also involved in these movements to some extent ( ▶ Fig. 1.31). Fig. 1.31 Palmar antebrachial muscles. (From THIEME Atlas of Anatomy, General Anatomy and Musculoskeletal System. 2nd ed. © Thieme 2014, illustration by Karl Wesker.) The flexor carpi ulnaris muscle arises with two heads. The humeral head originates from the medial epicondyle of the humerus and the antebrachial fascia, and the ulnar head originates from the dorsal aspect of the olecranon and the proximal two-thirds of the posterior border of the ulna. Its muscle belly is around 25 cm long, 4 cm wide, and 1 cm thick.256 Of all the antebrachial muscles, the flexor carpi ulnaris is located the most ulnarward in the superficial area of the muscle layers. The muscle inserts at the pisiform (easily palpable and visible) and in the further course, inserts with one part (with the involvement of the pisohamate ligament) at the hook of hamate and with the other part (with the involvement of the pisometacarpal ligament) at the palmar base of the fifth metacarpal. It is the strongest wrist flexor and is involved in ulnar deviation (with the involvement of the extensor carpi ulnaris and extensor digitorum muscles). The insertion fibers of the flexor carpi ulnaris muscle also contribute to forming the ulnar canal (“Guyon’s canal”), which allows passage of the ulnar nerve and ulnar artery.229 This area is frequently the site of compression of the ulnar nerve (“ulnar tunnel syndrome” or “Guyon’s canal syndrome”).200 In terms of function, during ulnar deviation, the pisohamate ligament supports the hamate with moving toward the ulnar styloid process, which holds the triquetrum and lunate in a position that is stable for this movement. This allows the flexor carpi ulnaris muscle via the pisohamate ligament to set these carpal bones into motion either directly or indirectly. As a result, ulnar deviation is involved in flexion and flexion is involved during ulnar deviation.160 Moreover, during ulnar deviation, the distal carpal row rotates ulnarward and the proximal carpal row rotates toward the radius with a slight rotation into extension.231 The flexor carpi radialis muscle also originates from the medial epicondyle of the humerus, the lateral and medial intermuscular septa of the upper arm, and the superficial antebrachial fascia. Its muscle belly, a semipennate muscle structure that is about 15 cm long and 1 to 2 cm thick, blends into its tendon (approx. 14 cm long) at about the mid-forearm (becomes visible during flexion.256) The radial artery runs lateral to the tendon. In this area, the artery is very easy to palpate. It is also part of the superficial muscle layer and is located radial to the palmaris longus muscle. In the area of the wrist joint, the flexor carpi radialis muscle moves into a tendon sheath up to the scaphoid tubercle and exits below the tubercle of trapezium into a narrow bony groove in the form of an osteofibrous canal.229 This canal is firmly attached to the capsuloligamentous structures225 and in this area becomes a gliding tunnel owing to the flexor retinaculum.229 The flexor pollicis longus muscle crosses over this tendon between the scaphoid and the trapezium. The muscle inserts palmar to the base of the second metacarpal. In rare cases, it also inserts at the third metacarpal with several fibers.60 In synergy with the flexor carpi ulnaris and palmaris longus muscles, it performs flexion in the wrist and at the same time, stabilizes the carpus. During radial deviation by the extensor carpi radialis longus muscle, the flexor carpi radialis muscle counteracts together with the second metacarpal and in so doing centers the carpal bones in the joint.43 During radial deviation, the distal carpal row rotates toward the radius, and the proximal carpal row rotates ulnarward, with a palmarward rotation.231 The palmaris longus muscle is no longer present in around 12.8% of the population,208 with women making up the majority of the cases.74 It also arises from the medial epicondyle and courses between the flexor carpi ulnaris and flexor carpi radialis muscles in the superficial muscle layer. It is one of the structures with the greatest variation in terms of shape, attachment, and bilateral occurrence.229 Its tendon, which is wide and flat, and on average 11.7 cm long and 0.4 cm wide, radiates into the flexor retinaculum and with some fibers into the palmar aponeurosis.229 In addition to producing weak flexion, it helps to stabilize the carpus and can increase the tension in the palmar fascia.256 This muscle arises with two heads, with the humeral head from the lateral epicondyle, the radial collateral ligament and the anular ligament of radius, as well as with the ulnar head, from the olecranon, the posterior surface of the ulna, the posterior border of the ulna, and the antebrachial fascia. It takes a superficial ulnarward course from the extensor digitorum muscle, continues lateral to the ulnar head (i.e., in the passage between the ulnar head and the styloid process), then extends into its tendon sheath (approx. 5 cm long) via the sixth tendon compartment.121 Some tendon fibers run palmarward and insert at the pisiform bone, the pisometacarpal ligament, and at the base of the fifth metacarpal. The tendon compartment, tendon sheath, and the tendon itself are firmly attached to the TFCC and are thus part of the whole structure. In functional terms (apart from enabling weak wrist extension200), it is the strongest marginal mover for ulnar deviation. In addition to its dynamic properties, it has an important influence on the ulnar head.229 During rotation of the hand, the muscle participates in guiding the joint bodies in the distal radioulnar joint250 and decelerates supination via the palmar radioulnar ligament.229 It also limits and stabilizes the movement of radial deviation and is involved in regulating pressure in the carpus via the TFCC. The flexor digitorum superficialis and profundus muscles are also involved in flexion of the wrist (see chapter on “Extrinsic Flexors of the Finger”). The extensor carpi radialis brevis and extensor carpi radialis longus muscles are the most important wrist extensors. In contrast, radial deviation is performed only by the extensor carpi radialis longus muscle.256 These two muscles are supported to some extent by the extensor digitorum muscle (see chapter on “Extensor Apparatus of the Finger”) and the extensor carpi ulnaris muscle ( ▶ Fig. 1.32). Fig. 1.32 Dorsal antebrachial muscles. (From THIEME Atlas of Anatomy, General Anatomy and Musculoskeletal System. 2nd ed. © Thieme 2014, illustration by Karl Wesker.) The extensor carpi radialis longus muscle arises distal to the brachioradialis muscle from the lateral supraepicondylar ridge of the humerus, the lateral intermuscular septum of the upper arm, and the lateral epicondyle of the humerus. It courses in the superficial muscle layer and is easily visible and palpable during contraction. The muscle belly already ends in its tendon in the upper part of the forearm. In the area of the distal radial epiphysis (on the dorsal aspect), together with the extensor carpi radialis brevis muscle, it then glides through the approximately 2.3-cm long second tendon compartment with the associated tendon sheath.229 The two structures are attached at the lateral aspect of the dorsal tubercle of the radius (Lister’s tubercle)229 which ensures the passage of the tendons. In addition, the tendon forms the floor and the deep-lying ulnar boundary of the anatomic snuffbox (tabatière anatomique). In its further course, the extensor carpi radialis muscle finally inserts at the base of the second metacarpal. This muscle originates from the lateral epicondyle (covered by the fibers of the extensor carpi radialis longus muscle60), the radial collateral ligament, and the anular ligament of the radius. In the area in which it originates, the muscle belly of the long wrist extensor covers the muscle belly of the short wrist extensor.256 It also courses in the superficial muscle layer (with a somewhat more lateral course than the extensor carpi radialis longus muscle) and also ends in its tendon in the upper part of the forearm. Via the second tendon compartment, it then inserts at the third metacarpal and the process of the third metacarpal. All of the structures of the extensor carpi radialis brevis and longus muscles are easy to palpate and visualize. Arthrokinematics is understood to mean the implementation of spatial osteokinematic movements in a joint, meaning between two articulating joint partners with more or less similarly curved joint surfaces. Typical arthrokinematic movements include rolling, gliding, traction, and compression.234 In contrast, osteokinematics describes the active and passive movements of the associated extremity in space as an angular movement (rotation) or a movement of the bone in space without rotation (translation).234 According to Kaltenborn’s convex–concave rule, during arthrokinematics, when moving the concave joint partner, there is gliding of the joint surface in the same direction in relation to the movement of the bone in space. When moving the convex joint partner, the joint surface glides in the opposite direction in relation to the movement of the bone in space.234 The kinematics of the wrist joint is a true masterpiece of Nature, whose biomechanical functions are still not fully understood today. The basis of the wide range of movement functions is the form of the individual carpal bones, the radioulnar joint, and the proximal and distal wrist joint, along with the many different ligaments. These structures together are responsible for counteracting the shifts in the positions of the carpal bones occurring as a result of muscle contraction, and therefore play a key role in stabilizing the wrist. According to Schmidt and Lanz (2003),229 in terms of joint mechanics, the carpal ligament systems can be divided into three ligament chains: The carpal retinacula, which may be regarded as “extra-articular slingshots.” Their oblique fiber structure not only stabilizes the distal radioulnar joint, but also counteracts ulnar displacement of the wrist.229 The “articular slingshot” is formed by ligaments with high tensile strength that arise from the radius and extend in palmar and dorsal directions, inserting at the triquetrum. The palmar slips are formed by the more transverse radiolunate and lunotriquetral ligaments. On the dorsal aspect, the dorsal radiotriquetral ligament passes around the ulnar margin of the radius and inserts obliquely into the triquetrum. With the triquetrum as the stone in the slingshot, the ulnar forces caused by the inclination of the radius are brought under control.133 The slingshot controls the range of motion in the proximal and distal wrist joints during both radial and ulnar deviation.229 It also acts as an ulnar support in flexion and extension of the hand.191 In a wider sense, the radioscaphocapitate ligament also belongs to the articular slingshot.233 It arises from the palmar lip of the radius, extends across the scaphoid, and inserts at the capitate. This ligament primarily serves to couple the movements of the lunate and capitate229 and to stabilize the joint between the lunate and capitate.147 The articular slingshot is therefore primarily formed via the triquetrum of the ulnar column and in synergism, via the scaphoid of the radial column, in order to provide the central T-shaped column, described by Taleisnik (1985),251 with the stability it requires for movements between the lunate and the capitate. The palmar support band (V-shaped ligaments) encompasses the middle and deep palmar fibrous structures. It serves to stabilize the capitate and prevents palmar displacement of the carpal bones in extension.229 The wrist joint can be regarded as a modified condyloid joint whose “condyle” is composed of eight carpal bones.233 However, the defined coordinated movements of the carpal bones are not based on a static condyle, but on a mobile system of joints that can adapt its form to correspond to the prevailing spatial and force requirements according to the principle of “variable geometry.”233 The spatial arrangement in the moving carpus is coordinated by the alignment of the joint surfaces and also by the control of the carpal ligaments. The eight carpal bones may be divided into two horizontal rows and three vertical columns according to their spatial configuration ( ▶ Fig. 1.33). The horizontal rows are formed by the proximal carpal bones (from radial to ulnar = scaphoid, lunate, triquetrum, and pisiform) and the distal carpal bones (from ulnar to radial = hamate, capitate, trapezoid, and trapezium). The range of motion between the proximal elements is relatively large. The range of motion is small between the elements of the distal row, which are strongly attached by ligaments233 to the second to fifth metacarpals (as a solid block of bone).229 According to Taleisnik (1985),251 the three vertical columns are divided into a radial column, which is formed by the scaphoid, an ulnar column formed by the triquetrum and pisiform229 ( ▶ Fig. 1.33c). The third, central column is T-shaped, whereby the distal carpal row with the trapezium, trapezoid, capitate, and hamate is connected to the radius via the lunate. This gives rise to two degrees of freedom with extension–flexion and radial and ulnar deviation. If the proximal and distal radioulnar joints are also taken into account, pronation and supination are also possible as a third degree of freedom. Fig. 1.33 Column models of the hand. (a) Navarro (1937). (b) Lichtman (1981). (c) Taleisnik (1985).
1.1 Introduction
1.2 Structure and Function of the Proximal and Distal Radioulnar Joints
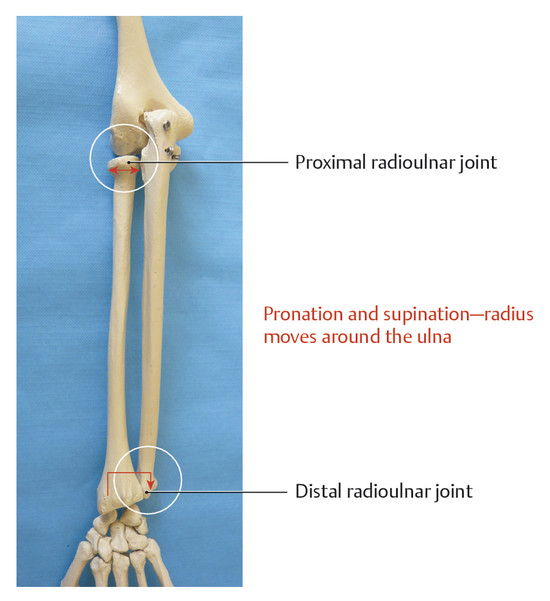
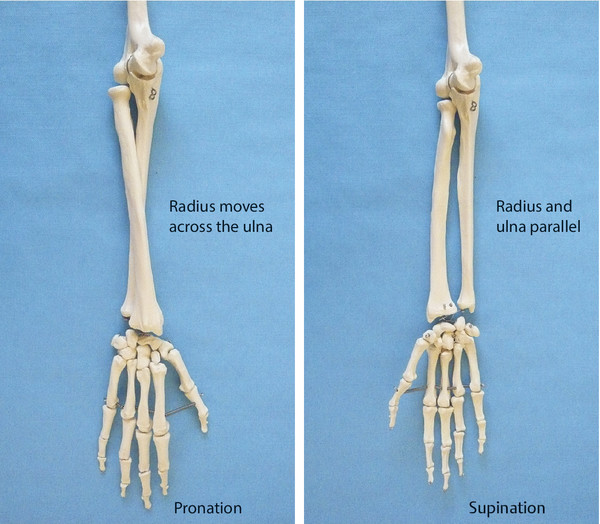
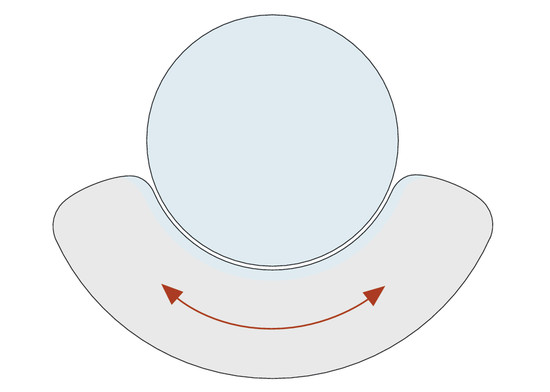
1.2.1 Anular Ligament of the Radius
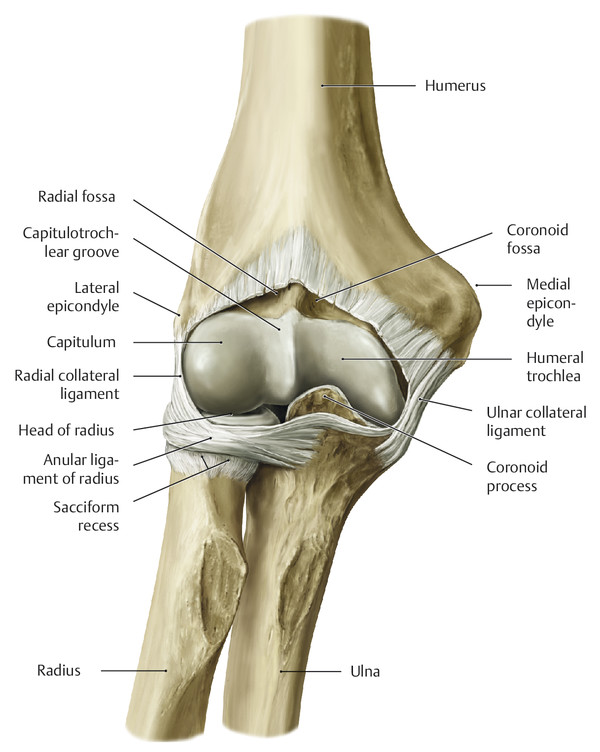
1.2.2 Oblique Cord
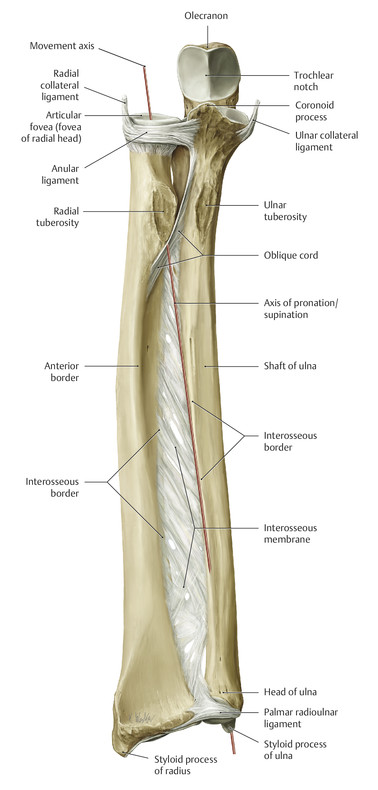
1.2.3 Interosseous Membrane of the Forearm
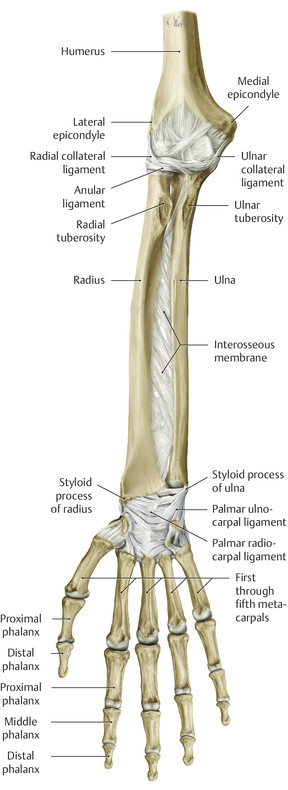
1.2.4 Structure and Function of the Triangular Fibrocartilage Complex
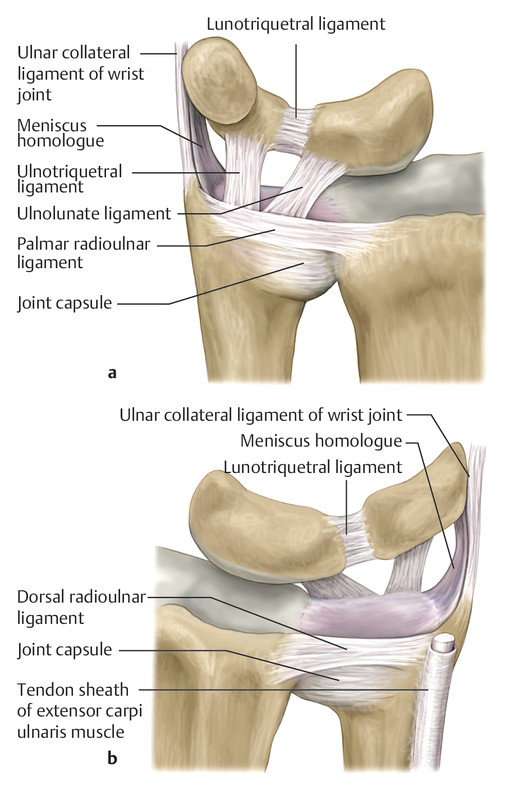

Ulnocarpal Disc and Meniscal Homologue
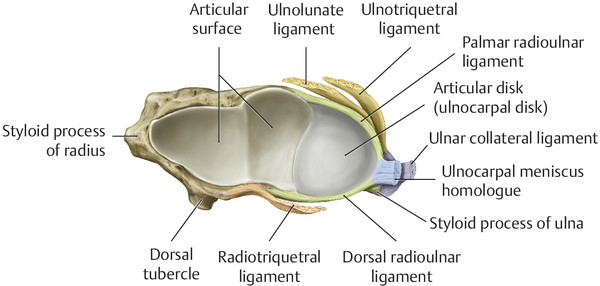
Palmar and Dorsal Radioulnar Ligaments
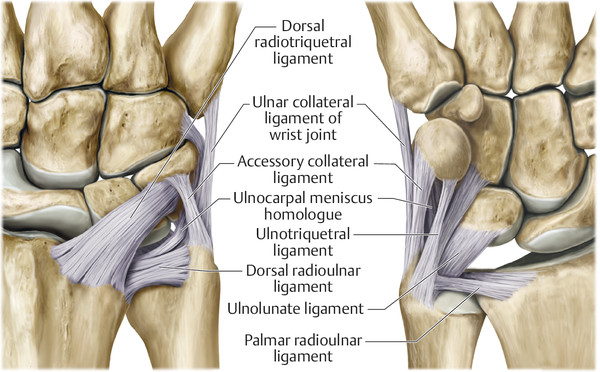
Ulnolunate and Ulnotriquetral Ligaments
Ulnar Collateral Ligament of Wrist Joint
Tendon Sheath of the Extensor Carpi Ulnaris Muscle
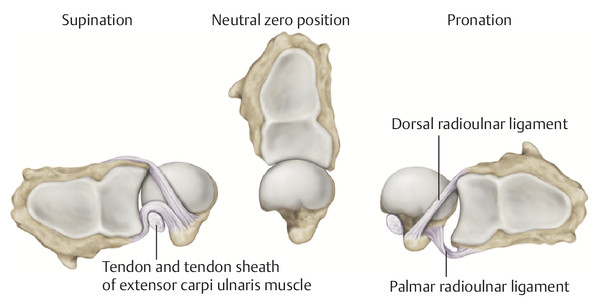
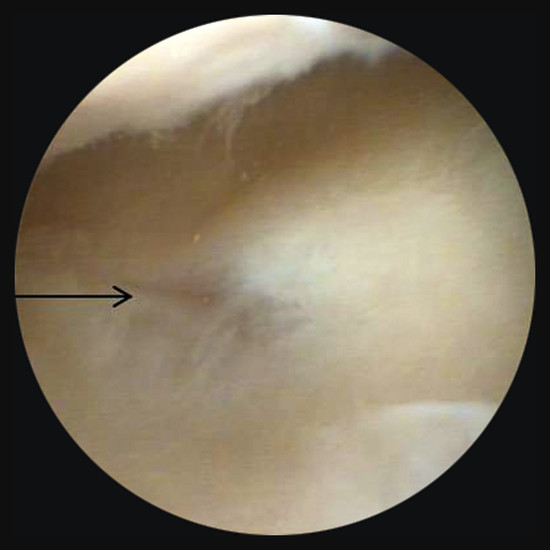
1.2.5 Muscles of the Radioulnar Joint—Pronation and Supination
Pronator Muscles
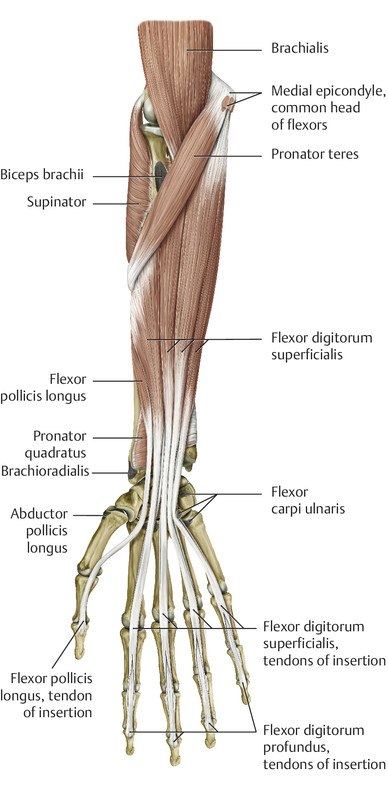
Supinator Muscles
1.3 Wrist and Movement Axes
1.3.1 Movement Axes
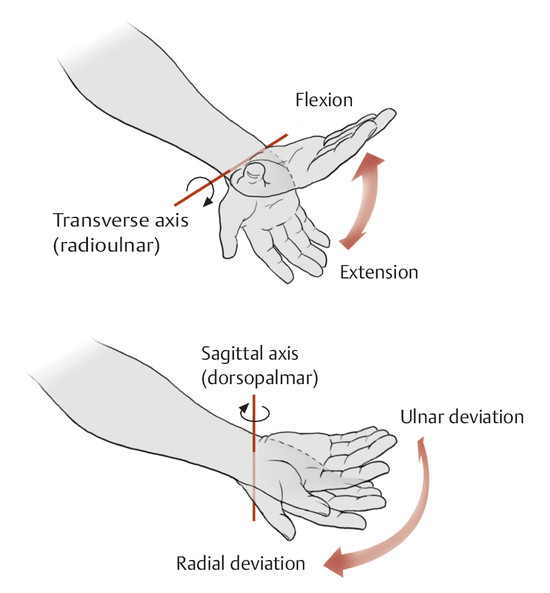
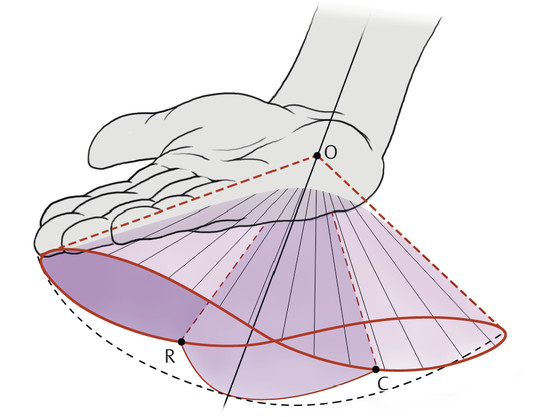
1.3.2 Structure and Function of the Wrist Joint
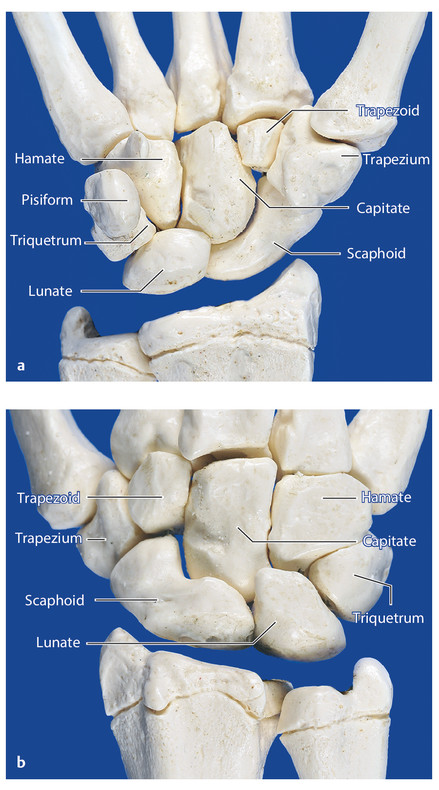
Carpal Bones
Scaphoid
Lunate
Triquetrum
Pisiform
Trapezium
Trapezoid
Capitate
Hamate
Joints
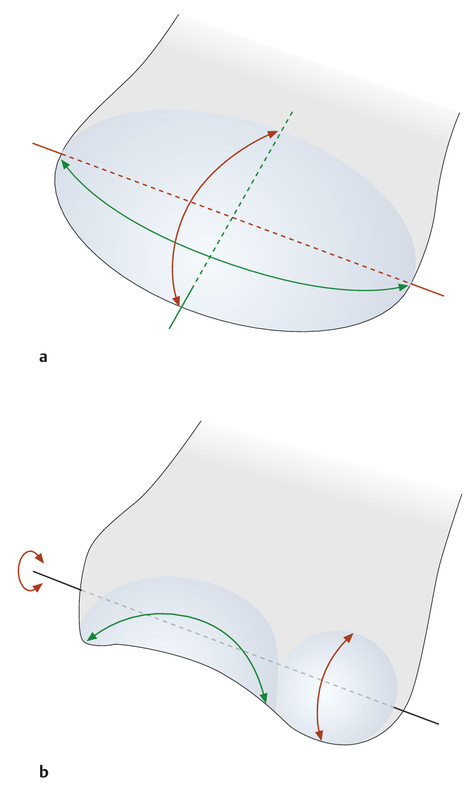
Wrist Joint
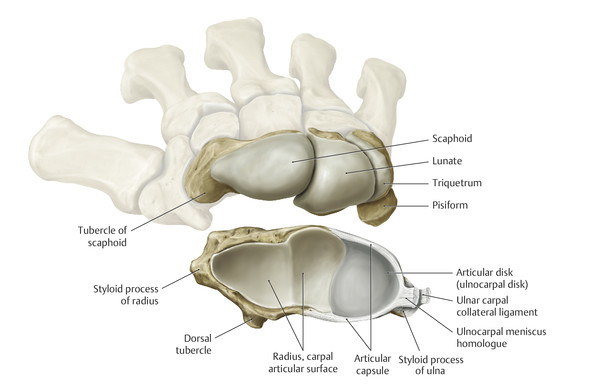
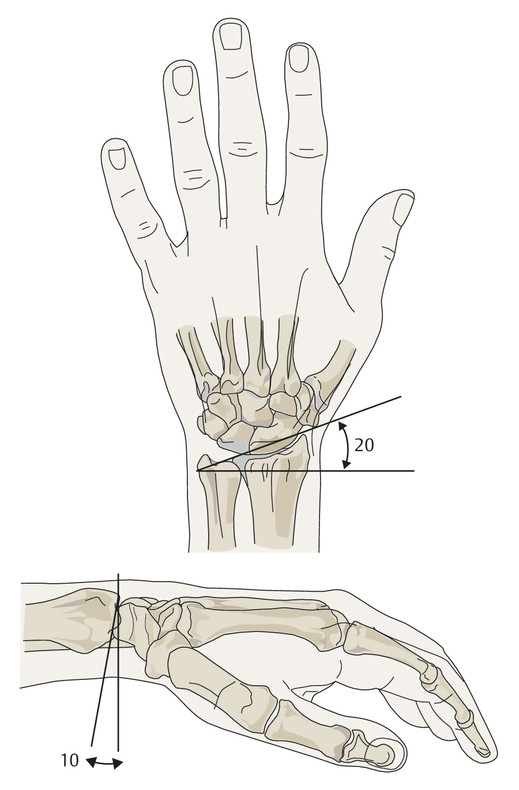
Midcarpal Joint
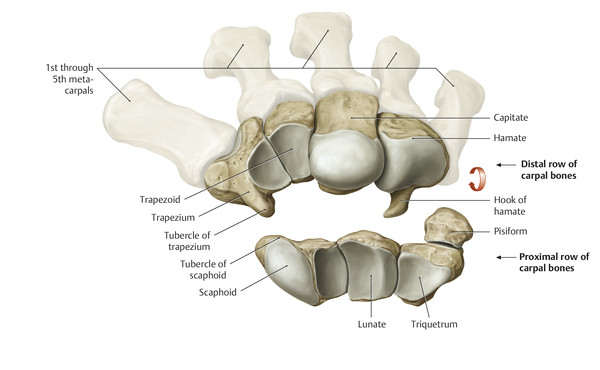
Carpal Joints
Second to Fifth Carpometacarpal Joints and Intermetacarpal Joints
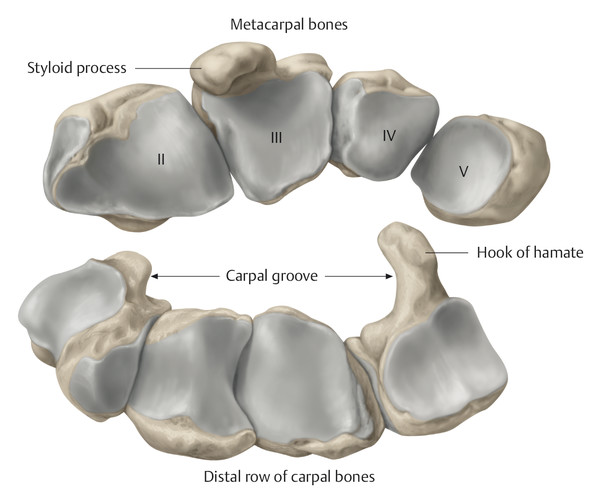
1.3.3 Ligament System and Wrist Stability
Superficial Layer of the Ligaments of the Wrist
Flexor Retinaculum

Extensor Retinaculum
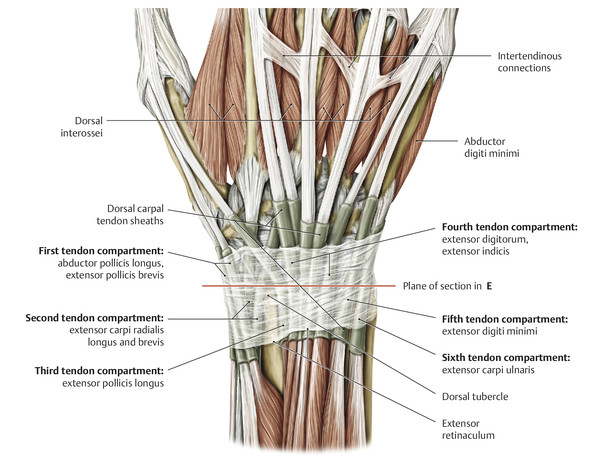
Middle Layer of Ligaments of the Hand
Radial Collateral Carpal Ligament
Dorsal and Palmar Radiocarpal Ligaments
Ligaments of the “Distal V”
Ligaments of the Palmar “Proximal V”
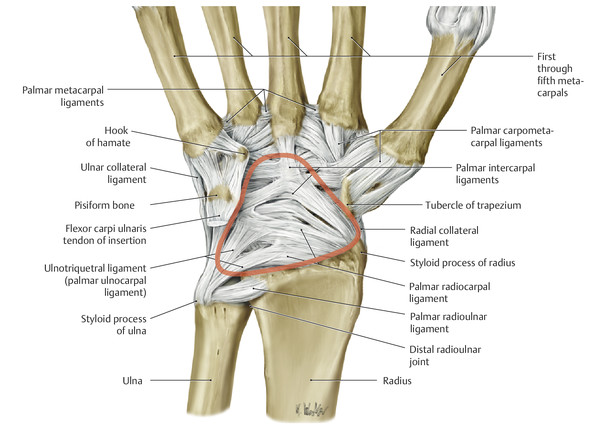
“Dorsal V” Ligament
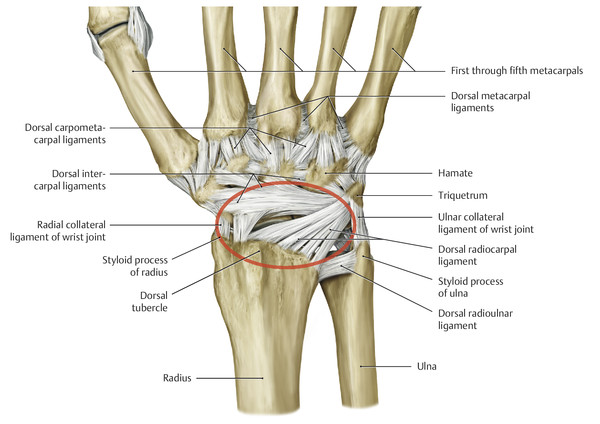
Interaction of the V-shaped Ligaments
Triangular Fibrocartilage Complex (TFCC)
Dorsal Intercarpal Ligaments
Radiate Carpal Ligament
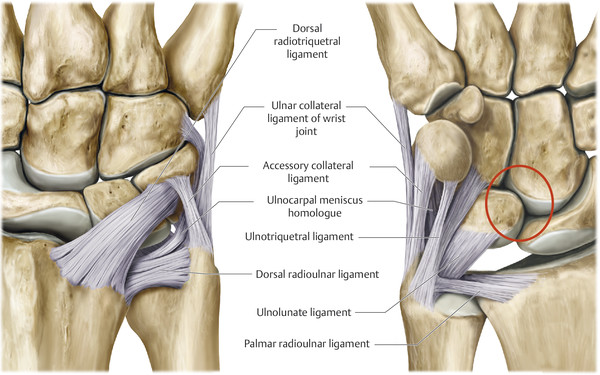
Deep Layer of the Ligaments of the Hand
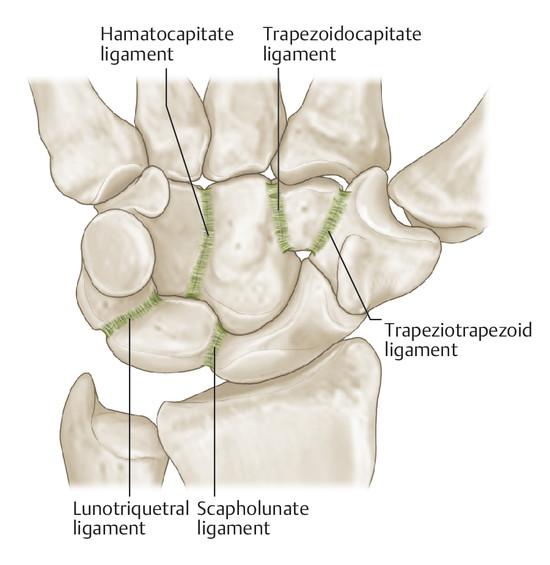
Trapeziotrapezoid Ligament and Palmar, Dorsal, and Interosseous Trapezoidocapitate Ligaments
Palmar, Dorsal, and Interosseous Hamatocapitate Ligaments
Lunotriquetral Ligament
Scapholunate Ligament
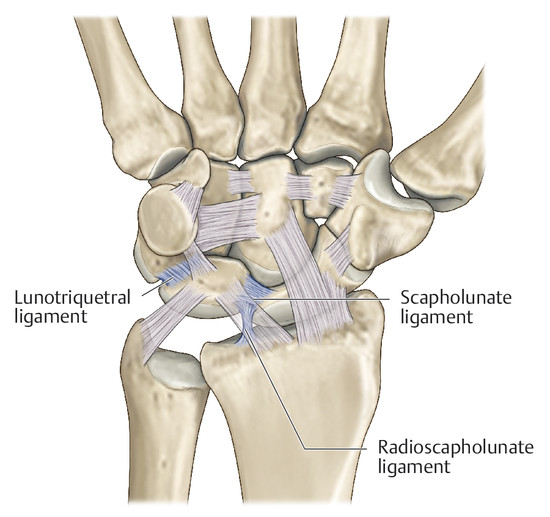

Scaphotrapezial Ligament
Radioscapholunate Ligament (Testut’s Ligament)
Conclusions
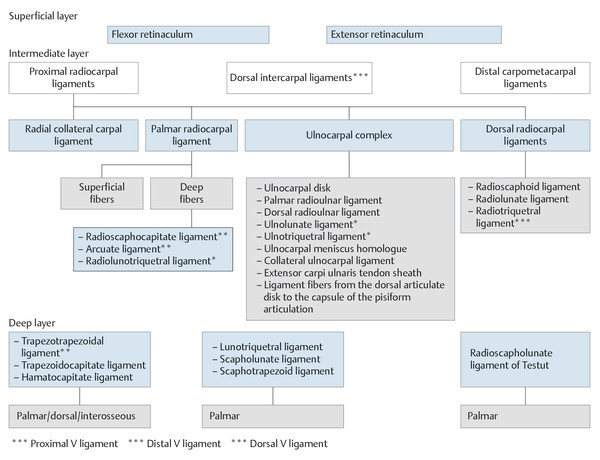
1.3.4 Muscles of the Wrist: Extension–Flexion, Radial Deviation–Ulnar Deviation, and Circumduction
Muscles Involved in Flexion and Ulnar Deviation of the Wrist
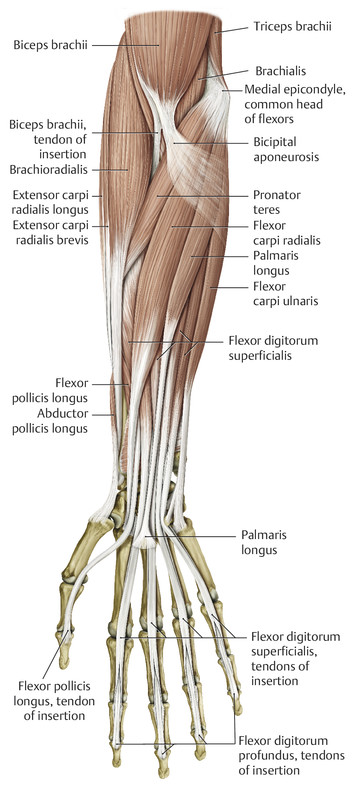
Flexor Carpi Ulnaris Muscle
Flexor Carpi Radialis Muscle
Palmaris Longus Muscle
Extensor Carpi Ulnaris Muscle
Muscles Involved in Extension and Radial Deviation of the Wrist
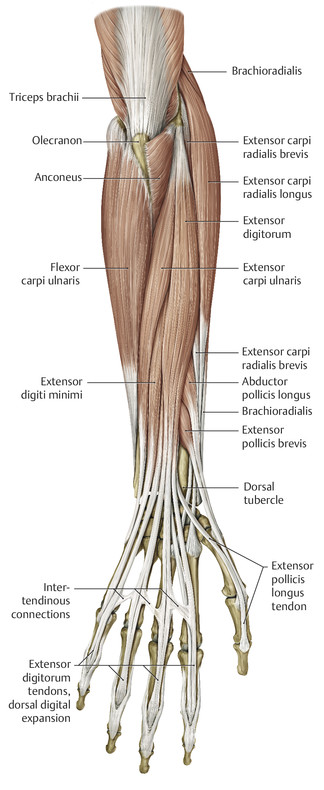
Extensor Carpi Radialis Longus Muscle
Extensor Carpi Radialis Brevis Muscle
1.3.5 Arthrokinematics of the Wrist Joint
Kinematics of the Wrist: General Aspects
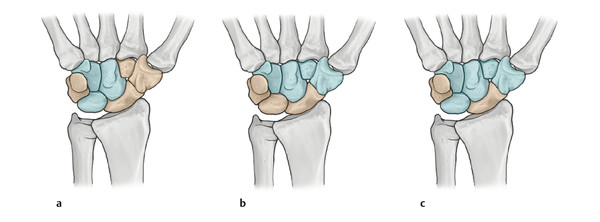
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree