Key points
• An implant-retained prosthesis has an average expected lifespan of 18-36 months.
• Successful rehabilitation with osseointegration requires the presence of viable bone in the area of reconstruction and a good surgical candidate.
• Maintaining realistic expectations of prosthetic reconstruction throughout the treatment process is crucial to the patient’s overall rehabilitation because treatment can be lengthy and has inherent technical limitations.
• Prosthetic rehabilitation requires a substantial commitment on the patient’s behalf, not only to endure the initial reconstructive treatment but also for lifetime maintenance, as prostheses are temporary devices with a relatively short lifespan and require regular replacement through the patient’s lifetime.
• Planning the placement of craniofacial implants is essential to optimize the prosthetic result.
• Planning with CT (medical CT and cone beam computed tomography [CBCT]) offers greater predictability and readiness for the surgeon because implant placement and bone can be assessed before surgery.
• Whether or not autologous reconstruction of the natural anatomy is possible, complementary, preprosthetic surgical reconstruction can augment and contribute to a more predictable and aesthetic prosthetic outcome when planned in consultation with the anaplastologist.
Introduction
While surgical reconstruction of the face is preferred, it is not always possible. In such circumstances, prosthetic reconstruction is a viable option for patients with acquired or congenital facial defects. It is essential that the surgical practitioner offering this treatment option fully appreciate the elements that contribute to successful facial prosthetic reconstruction and rehabilitation. Anaplastology is an allied health specialty that provides facial and body “somato” external prostheses (i.e., breast, nipple, fingers, toes, stents, and healing or molding devices). This chapter will focus on the provision of facial prostheses. This chapter discusses factors that are elemental to the reconstructive surgeon’s repertoire in caring for the individual requiring restoration of facial anatomy and appearance with external, artificial prostheses.
“The basics”—facial prosthetic rehabilitation
Facial prosthetic devices, such as a nose, eye, or ear, are removable devices that can be worn by the patient daily and removed each night for cleaning and skin hygiene. On average, facial prostheses last 1.5 to 2+ years with regular wear before a replacement is required (depending on the type of prosthesis and retention used). , Prostheses can be retained by bar-and-clip or magnet retention systems connected to surgically placed implants with adhesives or by mechanical means (i.e., attachment to eyeglasses). , This chapter serves as a primer for physicians in understanding the fundamentals of facial prosthetic rehabilitation as a treatment option, with emphasis on implant-retained devices and surgery ( Fig. 32.1 A, B).
How are facial prostheses made and who makes them?
The process for making a facial prosthesis is highly technical and often requires a substantial amount of time, both clinically and in the laboratory; digital technologies help reduce this time when employed with efficiency. Planning the design for a prosthesis should be considered before any surgery because the outcomes of surgical resection, subsequent reconstruction, and implantation dictate the potential for a successful facial prosthesis. Surgeons who participate in tumor resection or reconstruction of the head and face should be well-versed in facial prosthetic reconstruction as a treatment option for their patients.
The successful prosthetic device is well-planned and designed before surgery. In this way, the anaplastologist can indicate to the surgeon the requirements for the ideal tissue bed, consider retention of the prosthesis, and discuss potential surgical reconstructive options to complement the planned prosthetic design. The typical process for facial prosthetic treatment involves consultation and education; identification of the retention method; definition of the treatment plan and timing of prosthetic appointments; surgical planning (if surgery is anticipated); surgical guide design and fabrication (when indicated); design of the prosthesis by the anaplastologist; fabrication of the device (sculpting, coloration, casting, finishing, and fitting); delivery and education; maintenance; and lifetime follow-up.
How is a prosthesis retained?
A facial prosthesis can be retained with the use of an adhesive or mechanically. The use of an adhesive to retain a facial prosthesis was common before “osseointegration,” which will be the primary focus of this chapter. Today, adhesives are used when a patient is not a candidate for surgical placement of implants or may not be able to manage the lifetime maintenance of percutaneous implants ( Fig. 32.2 A, B).

Retention with adhesives can be very effective if there is a stable tissue bed with limited mobility where the prosthesis will adhere. Gross mobility of the skin, as occurs with facial expression, can cause detachment of the adhesive, which can become problematic for the patient.
Prostheses can also be retained by attachment to eyeglasses; held on with bands, straps, or tape; or retained by engaging naturally occurring undercuts or cavities in the patient’s anatomy. Although there are multiple methods to attach a prosthesis, retention by means of osseointegrated implants offers the most reliable method of retaining a facial prosthesis , (see Figs. 32.1 and 32.2 ).
Wearing an implant-retained prosthesis offers certain advantages compared with those retained with adhesives. An implant-retained prosthesis only fits on the patient in one position—an aspect of adhesive retention that often presents a challenge. When adhesive application is not required, the margins (edges) of the prosthesis can be made thinner, providing greater visual integration with the surrounding skin. Retention with implants typically enables the patient to wear the prosthesis for a longer period each day with greater reassurance that the prosthesis will not become loose or dislodged. It has also been reported that patients who wear implant-retained prostheses incorporate the prosthesis into their self-image more quickly through the concept of “osseoperception.” , A more detailed discussion of implant-retained prostheses and osseointegration follows.
How long does a prosthesis last?
A prosthesis can last as few as 6 months or as long as 6 years. Compared with an implant-retained prosthesis, an adhesive-retained prosthesis generally lasts for a shorter period due to the daily, manual removal of the adhesives and the solvents required to facilitate this. How long a prosthesis lasts depends very much on the means of retention, how frequently the prosthesis is worn, how well the patient cares for it, the cleanliness of the environment in which it is worn, exposure to the elements, and durability of the material it is made of. Adhesive-retained prostheses have a shorter life, lasting, on average, from 6 months to 18 months, whereas an implant-retained prosthesis has an average expected lifespan of 18-36 months.
Patient evaluation
Who is a candidate for a facial prosthesis?
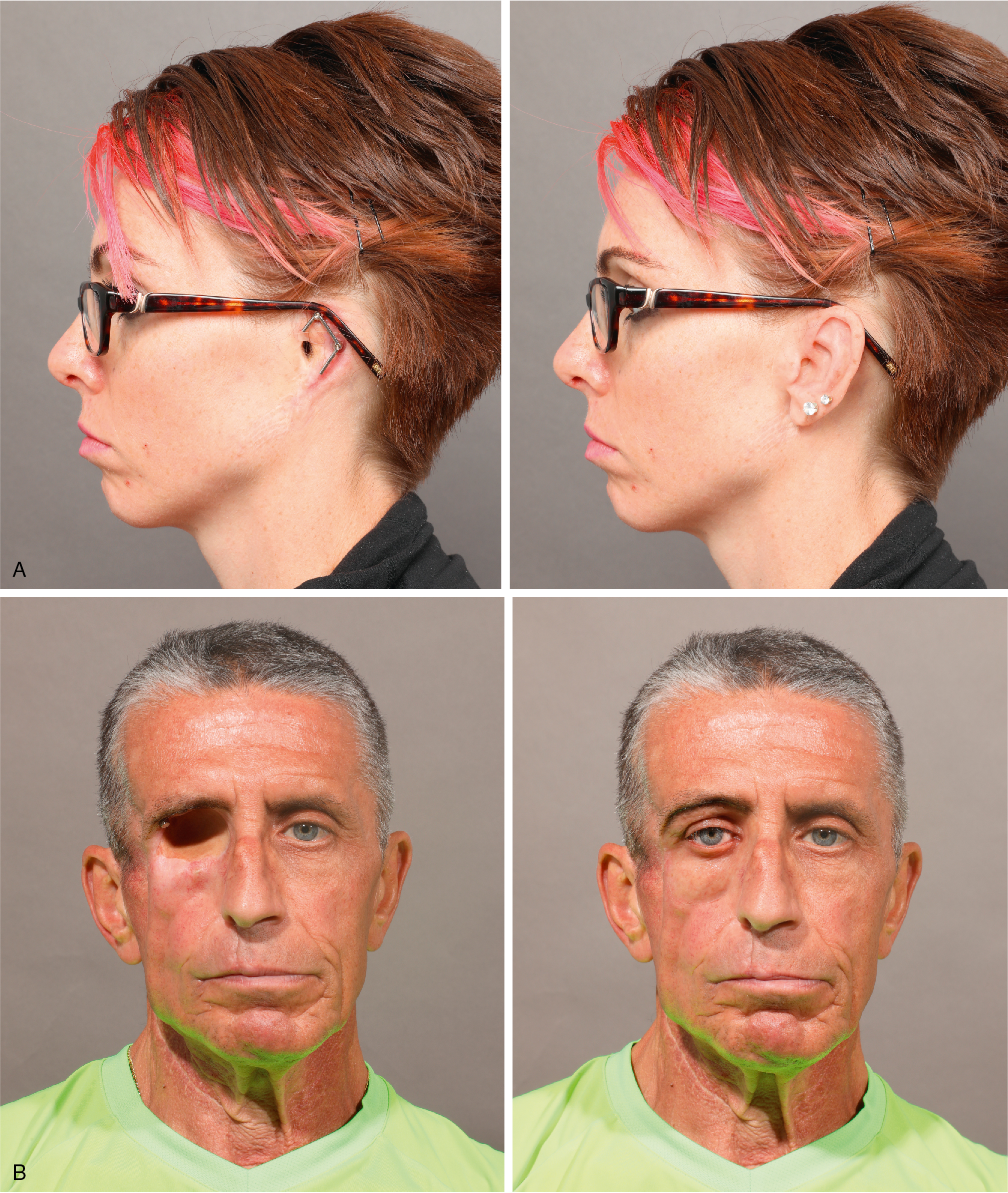
When a person is missing a part of the face or head as the result of a congenital condition, trauma, or surgical tumor removal, a removable prosthesis may be a reasonable alternative to surgery. When surgical reconstructive options have been exhausted, the prognosis is poor, or further surgery is not desired, a facial prosthesis can restore the appearance of the patient’s natural anatomy and may contribute to restored function and improvement in quality of life , ( Fig. 32.3 A–C).

Who is a candidate for osseointegration?
Most patients rehabilitated by osseointegrated facial prostheses are those with head and neck cancer. Another growing population comprises patients with congenital microtia, when autogenous reconstruction is unsuitable or has proven unsuccessful. Survivors of trauma, including motor vehicle accidents and burns, are also typically ideal candidates for osseointegration. Successful rehabilitation with osseointegration requires the presence of viable bone in the area of reconstruction and a good surgical candidate. Some relative contraindications include smoking, previous radiation therapy, religious beliefs, or lack of psychologic readiness. However, a patient is not automatically excluded from surgery for placement of implants even under these circumstances. Many patients who have undergone radiation therapy, for instance, have successfully worn implant-retained facial prostheses for many years. Additionally, adjunctive therapies, such as hyperbaric oxygen (HBO), have been employed on the presumption that it contributes to improved implant survival; however, there is some controversy over the use of this treatment. ,
Education—managing realistic expectations
It is essential that the patient and the family are well informed and educated on the options before pursuing this treatment. Maintaining realistic expectations of prosthetic reconstruction throughout the treatment process is crucial to the patient’s overall rehabilitation because treatment can be lengthy and has inherent technical limitations. Often, psychology teams are engaged early in the treatment process to assess the patient’s understanding of what is possible and to gauge the patient’s and the family’s expectations of the final outcomes. Prosthetic rehabilitation requires a substantial commitment on the patient’s behalf, not only to endure the initial reconstructive treatment but also for lifetime maintenance, as prostheses are temporary devices with a relatively short lifespan and require regular replacement through the patient’s lifetime. Having a strong, positive, and supportive network of family, friends, community, and other care providers contributes substantially to a patient’s prosthetic rehabilitation.
It is important that the patient, the family, and the care providers alike recognize and accept the limitations of prosthetic devices. At the time of this writing, prostheses are primarily artificial static devices that provide limited anatomic and physiologic functions and contribute more to psychosocial function and quality of life. , For example, at present, an oculoorbital prosthesis will not blink or move, although many research teams have pursued movable prosthetic designs. Prosthetic devices, such as intraoral or internal devices—obturators, palatal lift devices, dentures, stents, heart valve replacements, and limb prosthetics—provide clear functional, anatomic, and physiologic benefits; however, facial prosthetic devices provide function by holding up eyeglasses in the case of a prosthetic nose or ear, or by securing a stethoscope or surgical mask in the case of a prosthetic ear. A prosthetic nose or orbital prosthesis provides a barrier for mucosal tissue protecting it from external debris and also aids in keeping sensitive tissues moist in internal cavities. Current understanding of quantifiable physiologic functional gain is limited, although researchers have explored this. More often, psychosocial function, which also can be difficult to quantify, and improvement in quality of life have been extensively described as important motivators in recommending or pursuing facial prosthetic treatment. , , ,
It is important that referring specialists are careful not to overinflate a patient’s and/or family’s expectations from prosthetic reconstructive treatment. In spite of a surgical service’s access to highly skilled anaplastologists, comments made to the patient and the family in an attempt to encourage, such as “They are so natural looking,” or “No one will ever know the difference,” can create unachievable expectations, compromising a patient’s rehabilitation potential and acceptance of the prosthesis.
History
A thorough medical history and physical examination should be performed at consultation to identify the full scope of the patient’s rehabilitative needs so that the patient can be referred to the appropriate specialists and treatment can be coordinated to address all of the clinical needs in a comprehensive manner. Facial prosthetic patients are often seen by a complement of multidisciplinary specialists, including an oncologic surgeon, a reconstructive surgeon, a craniofacial surgeon, an otolaryngologist, an audiologist, an anaplastologist, a psychologist, a maxillofacial prosthodontist, an orthodontist, an ocularist, a speech language pathologist, a genetic counselor, and other specialists, as indicated.
Besides assessing for general medical and mental health, healing and recovery from surgery, adjuvant therapies, and skin allergies, the patient should be assessed for ability to manage the daily placement, removal and cleaning of the prosthesis, general hygiene, claustrophobia (if physical facial impressions are indicated), social history (including smoking), vision, manual dexterity, and some aspects of daily home and work life, including availability of a support network. Manual dexterity and absence of hand/arm tremors are also important considerations for the patient’s ability to manage the daily placement, removal, and cleaning of the prosthesis.
Congenital conditions
Patients with congenital conditions that affect facial appearance and function (e.g., microtia or anotia) may be candidates for prosthetic rehabilitation when optimal surgical reconstruction is not achievable. Clinical presentation of congenital microtia represents both functional and aesthetic considerations. Physicians must recognize that congenital conditions, such as microtia, may be evidence of other craniofacial conditions with more extensive clinical, functional, and developmental implications. Patients should be evaluated by a comprehensive craniofacial team to ensure that all aspects of the child’s functional and developmental needs are appropriately addressed. For instance, in the case of microtia, anotia, or atresia, attention to the patient’s audiologic needs are paramount, especially in the case of bilateral presentation, as can be the case with Treacher-Collins or Goldenhar syndrome, with special consideration for audiologic and speech development (see Fig. 32.3 ).
Trauma
Survivors of burns, motor vehicle accidents, or other traumatic injuries often suffer loss or disfigurement of facial features. Traumatic loss of the ear is not uncommon in these circumstances. In traumatic incidents, the skin may be badly scarred or the blood supply interrupted, presenting a situation where potential autologous reconstruction is compromised. Prosthetic rehabilitation of this patient population has proven to be a reliable treatment choice when anaplastologists are available to provide the needed treatment ( Fig. 32.4 A, B).

Disease
Head and neck and skin cancers are often the culprits when individuals lose part of the face or head due to tumor resection. Aggressive fungal infections, benign tumors, congenital hemangiomas, and arteriovenous malformations (AVMs) have also resulted in removal of parts of the face. In these circumstances, surgical reconstruction may not be possible; may involve multiple complex surgical procedures with unpredictable results; or may not be preferred to allow adequate surveillance of the defect and margins for recurrent tumor. Radiation therapy or other comorbid conditions may also compromise the potential for surgical reconstruction. For these patients, a prosthetic device may be the preferred choice by both the clinician and the patient because it requires fewer surgical procedures, is less invasive, and allows for continued tumor surveillance (see Fig. 32.2 ).
Psychologic considerations
Facial prosthetic rehabilitation offers the potential to improve the quality of life for survivors of cancer or trauma or for those who are living with congenitally missing or malformed anatomy. Quantifying this may be difficult, but observation and clinical experience have demonstrated that in the majority of cases, patients have experienced improved confidence, comfort with public interaction, and renewed motivation in their daily living. Less commonly, some patients struggle psychologically with the adaptation to wearing a prosthesis. This is often due to unrealistic expectations of what facial prosthetic treatment can provide. These unrealistic expectations can be inherent or built up by how the treatment was initially described by their care providers. It is important for patients to understand that a prosthesis will not “give them their eye back” or feel the same as their natural nose. In the majority of cases, facial prostheses are static, removable, silicone (typically) devices that do not “blink,” “move,” or “animate” with facial expression. It is the responsibility of all care providers to avoid inflating the patient’s expectations regarding this treatment. With reasonable expectations, the patient has the greatest chance of full rehabilitation through facial prosthetic treatment.
Indications and contraindications
A thorough medical history will reveal potential contraindications to prosthetic treatment. As previously discussed, psychologic readiness for treatment and the individual patient’s potential to accept prosthetic restoration are important considerations. In cases of congenital conditions, understanding the goals of both the patient and his or her parents are important to ensure successful rehabilitation. Psychologic considerations for the congenital population include issues related to “self-concept” and “bullying,” which can impact the child’s developmental learning experience.
For survivors of cancer, it is essential to factor in adjuvant chemotherapy and radiation, which can impact implant survival rates. , , Other general contraindications to surgery also apply to facial prosthetic treatment; patients who smoke are encouraged to quit in preparation for surgery (and for general health); smoking also shortens the lifespan of the prosthesis itself.
Preoperative planning
A team approach to prosthetic craniofacial rehabilitation is vital to achieve a successful outcome and to give the patient implants that are stable and free from infections. When an implant-retained prosthesis is planned, it is essential that there is collaboration between the surgeon and the anaplastologist. Although the surgery to place implants may not be considered technically complex, it is a very technique-specific procedure. It is essential that the implants be placed in the right positions and with the right trajectory appropriate for the design of the definitive prosthesis.
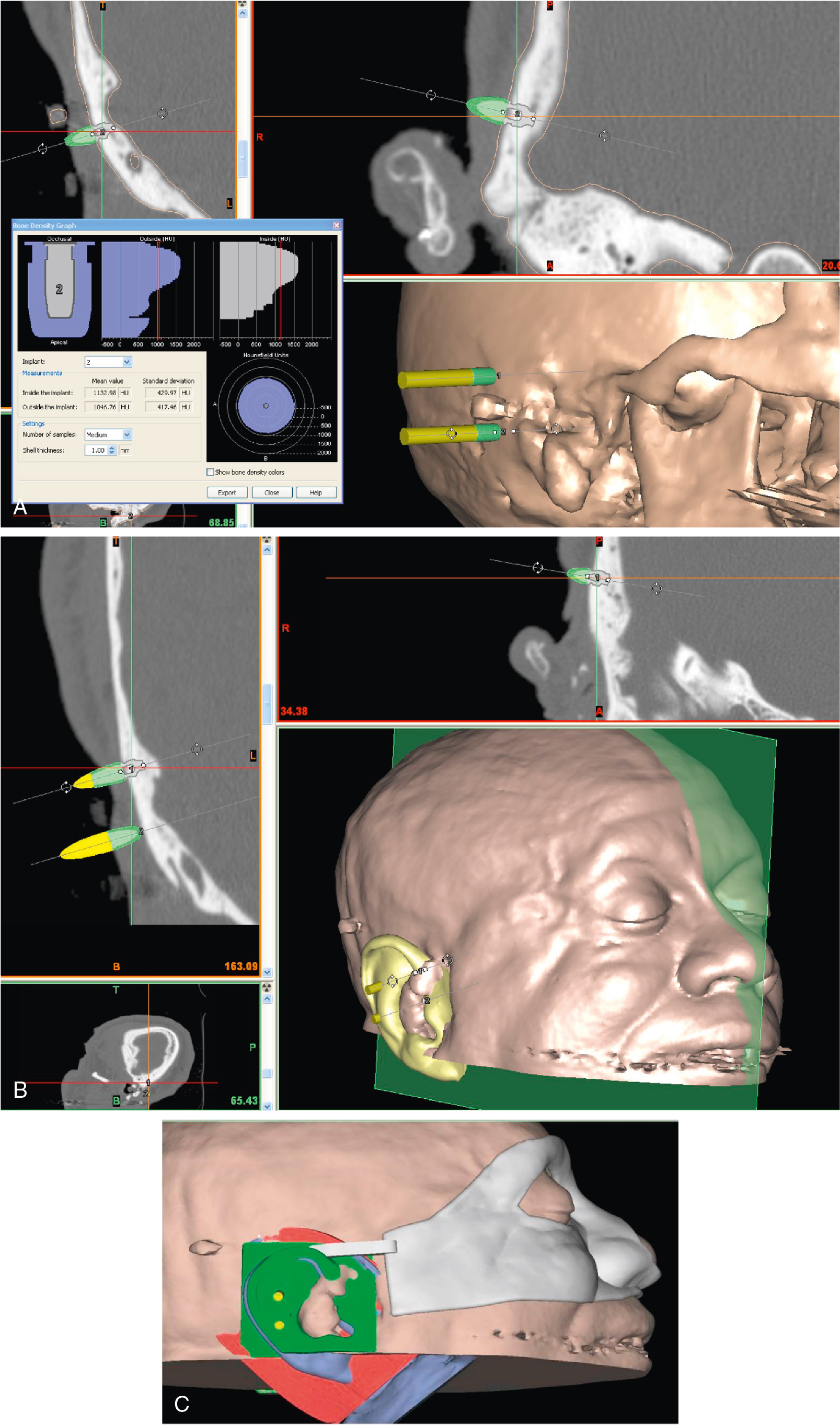
Presurgical planning is essential when placing implants for a facial prosthesis. Implants that are not placed in appropriate positions or at reasonable trajectories may result in an ill-fitting prosthesis that looks unnatural or has bulky extensions foreign to the natural anatomy. For this reason, the surgeon should ensure that proper planning is completed and that there is common understanding of the surgical goals to complement the goals of the prosthetic treatment. Typically, the anaplastologist can fabricate a guide that will be sterilized and used in the operative field to indicate ideal positions for implant placement. Alternative positions are also often indicated if the quality or volume of bone intraoperatively is found to be insufficient for implant placement. For this reason, computed tomography (CT) is used to plan implant placement preoperatively to identify bone of sufficient volume and density; however, this is not a guarantee of intraoperative results ( Fig. 32.5 A–C). The figure shows virtual planning of implant placement, using medical CT imaging and surgical planning software, which enable evaluation of bone in consideration of the planned prosthesis and virtual design of surgical guides that can be printed by 3D printing to transfer the surgical plan to the operating theater.
In recent years, the use of digital technologies has made planning possible to the submillimeter level of accuracy. However, it is the team approach as well as coordinated planning that is critical for optimal outcomes, whether digital or more conventional analog methods are employed.
Planning the placement of craniofacial implants is essential to optimize the prosthetic result. Access to available bone of sufficient depth and placement of the implant fixtures and abutments in suitable positions for prosthesis retention, while facilitating daily cleaning by the patient, warrants careful presurgical planning of appropriate implant sites. In addition, presurgical planning allows the surgeon and the anaplastologist to discuss potential challenges related to postsurgical soft tissue management with regard to planned implant positioning.
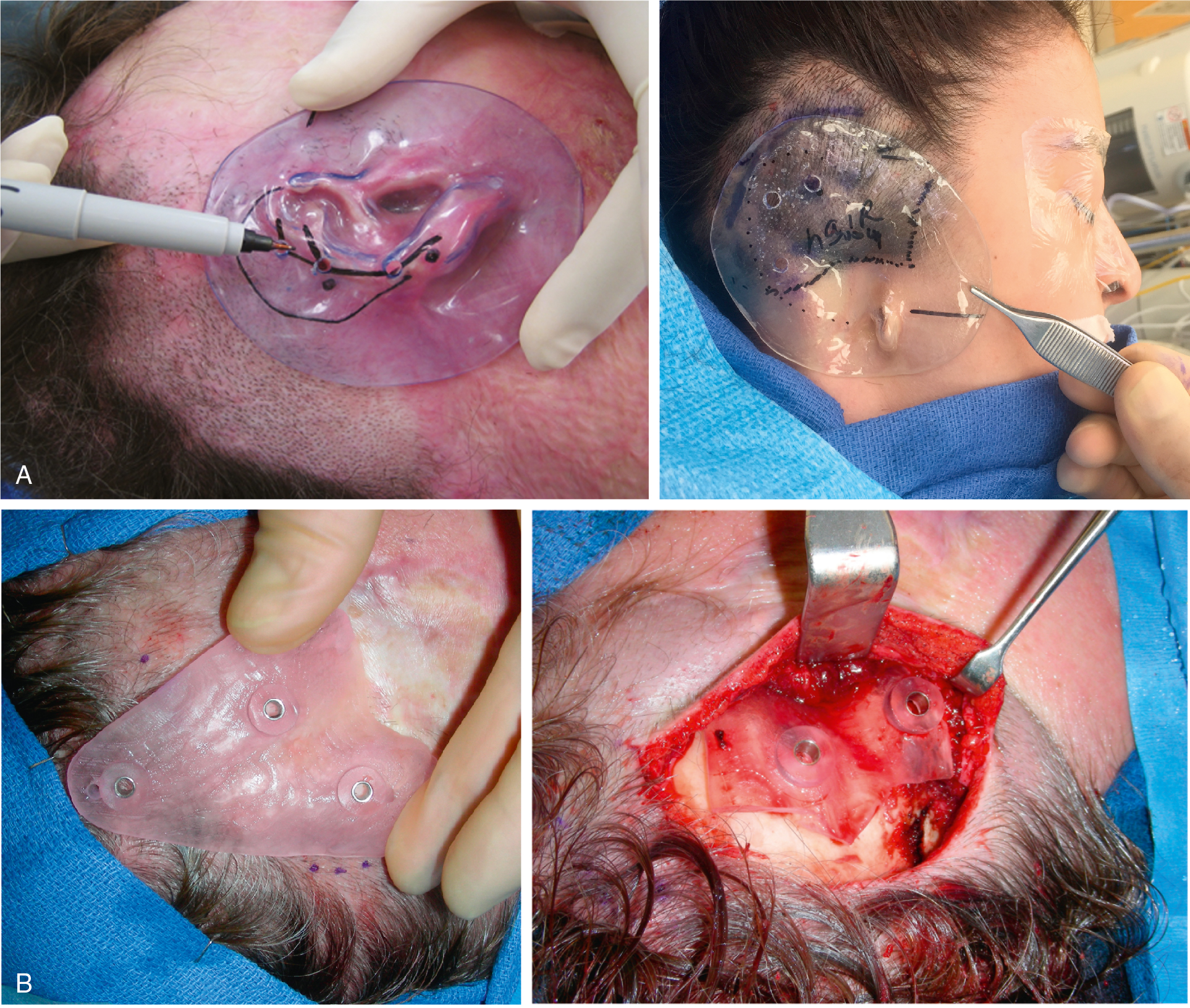
The use of templates and guides for surgery has been shown to provide accurate placement of craniofacial implants. Various designs have been proposed in publications. , Both soft tissue–fitting and bone-borne guides have been successfully used for the surgical placement of craniofacial implants (see Fig. 32.5 ; Figs. 32.6 A, B, 32.7 A, B, and 32.8 A, B). Each type of guide has its own merits, and the choice of a soft tissue–fitting guide versus a bone-borne guide should be carefully made in consultation with the anaplastologist and based on agreed-upon goals of surgery. Once sterilized, the guides can be used in the operating theater to identify ideal implant positions. Regardless of the style of guide utilized (soft tissue–fitting or bone-borne), engagement of the anatomic structures is essential for proper seating of the guide in the operating theater. Consideration should be given to whether the guide will be utilized before or after the sterile field is draped, given that the surgeon’s field of view with a tightly draped sterile field will conceal facial features that might be used for positional reference and local orientation. By making the template (guide) large enough to engage adjacent anatomic structures, accurate positioning is achievable. Soft tissue–fitting templates cannot, however, indicate the thickness or condition of the underlying bone, and the template should include optional placement sites for the fixtures (see Figs. 32.6 and 32.7 ).