Chapter 5 Analysis of Anterior Cruciate Ligament Injury-Prevention Programs for the Female Athlete
Introduction
Since the passage of the Title IX Educational Amendment, there has been an exponential increase of female participation in sports at both the collegiate (fivefold increase over the last 30 years)1 and high-school (tenfold increase over the last 30 years)2 levels. Although participation in organized sports has many physical and psychological benefits, including decreases in obesity, hypertension, diabetes mellitus, and coronary heart disease, this increase has subsequently led to an increase in sports-related injuries.3 While identifying risk factors with regard to sports-related injury, researchers have found an increased rate of ligamentous knee injuries, especially of the ACL, in female athletes compared with their male counterparts participating in similar activities.4–9 Among athletes in pivoting and jumping sports, adolescent females face a fourfold to sixfold increased risk of ACL injury compared with their male counterparts.6,10,11
The ACL is at risk for injury during activities that require pivoting, decelerating, or landing from a jump, such as soccer, basketball, volleyball, and team handball, as well as American football and downhill skiing.12 An estimated 80,000 to 250,000 ACL injuries occur annually in the United States alone.12,13 The highest incidence of these injuries occurs typically in young athletes between the ages of 15 to 25, which constitutes nearly 50% of all reported ACL injuries.3 Furthermore, the incidence among female athletes exceeds their male counterparts by a twofold to eightfold frequency12,13,14 Arendt and Dick examined the increased incidence of ACL injury among NCAA Division I athletes participating in basketball and soccer over a 5-year period.15 These two sports were chosen due to the fact that there is a strong similarity between the men’s and women’s games with regard to rules, training and development, style of play, type of playing surface, and the intensity of the competition. The injury rate was recorded and analyzed per athlete-exposure, where one practice session or game was defined as one exposure. The average ACL injury rate was 0.31 per 1000 athlete-exposures for female soccer and 0.29 per 1000 athlete-exposures for female basketball, compared with 0.13 for male soccer and 0.07 for male basketball per 1000 athlete-exposures. These epidemiological data for ACL injury rates statistically signify the blatant discrepancy that exists between genders.6
ACL rupture is a severe ligamentous knee injury, leading to functional instability in the short term and degenerative joint disease in the long term. Injury to the ligament can lead to prolonged absence from both work and sport and can initiate the early onset of degenerative osteoarthritis.15,16 Although ACL reconstructive procedures are readily available, the injury is painful and costly and can be debilitating. In the United States, at least 50,000 ACL reconstructions are performed each year at a cost of about $17,000 per procedure.14,17 The direct medical cost for reconstructive surgeries alone is just under $1 billion per year ($850,000,000). This figure does not include initial treatment costs of all ACL injuries, the rehabilitation costs after reconstruction, or the costs of conservative treatment and rehabilitation of those injuries that are not repaired.18 Complete ACL injuries can lead to chronic knee pathology, including instability, secondary injury to the menisci and articular cartilage, and an early onset of osteoarthritis. Approximately 66% of all patients with complete ACL injury incur damage to the menisci and the articular cartilage of the femur, patella, and/or tibia. This injury, coupled with the risk of secondary injury, can significantly decrease the ability of patients to complete their activities of daily living and affect their quality of life. The surgical reconstruction of a ruptured ACL can significantly reduce the risk of secondary injury. Seitz et al18a noted that 65% of ACL deficient patients sustained a secondary meniscal injury within 2.5 years of the initial date of injury.
Data show that despite surgical treatment of this injury, patients frequently develop posttraumatic arthritis of the knee.* Despite the most earnest efforts of orthopaedic surgeons to preserve the integrity of the knee joint during ACL reconstructive surgery, ACL reconstructed individuals continue to report with early onset of osteoarthritis. Lohmander et al completed a 12-year longitudinal study to follow up on female athletes who previously underwent ACL reconstruction after sustaining an injury while playing soccer.10 They found that 55 women (82%) had radiographic changes in their index knee and 34 (51%) fulfilled the criterion for radiographic knee osteoarthritis. The mean age for the subjects involved with this study was 31.
Gillquist et al noted that the prevalence of radiographic knee gonarthrosis is significantly higher in the injured knee compared with the unaffected contralateral limb.16 The implications of this research are ominous—hence the increased need for the prevention of these injuries from occurring in the first place.7
A multidisciplinary meeting was held in Hunt Valley, Maryland, in 1999 involving biomechanists, physicians, certified athletic trainers, and physical therapists to delineate specific risk factors thought to be directly correlated to the increased incidence of ACL injuries in the female athlete.5 The identified risk factors included anatomy, hormones, environment, and biomechanics. This meeting spurred the development of various ACL injury-prevention programs and led to increased interest and financial funding in this area of research. This group of researchers reconvened in Atlanta, Georgia, in January 2005 to reevaluate the identified risk factors and to determine what progress has been made since the inaugural meeting in 1999.
Anterior cruciate ligament Injury-Prevention Studies
A growing number of injury-prevention programs targeted at reducing the risk of ligamentous knee injury in general and ACL injury in particular have been reported in the literature. Although a number of risk factors for ACL injury have been proposed, only the biomechanical risk factors have been examined in sufficient depth to support the design and evaluation of prevention interventions.2,14
During passive motion, tension in the ACL decreases from 0 to 35 degrees and then increases again with further flexion.5 Thus, a combination of maximal ACL tension and anterior tibial translation force occurs with quadriceps firing and joint compressive loading at or near full extension. Contraction of the hamstrings decreases ACL strain in all positions. However, co-contraction of the hamstrings is not enough to overcome the strain produced by the quadriceps.7
As the knee moves into extension, female athletes take a significantly longer time to activate their hamstrings than do their male counterparts.8,9 At initial contact, males take approximately 150 ms to achieve their peak flexion angle compared with females, who take approximately 200 ms. Landing from a jump, in-line deceleration, and pivoting all involve eccentric contraction of the quadriceps to prevent the extended knee from collapsing into flexion. In laboratory studies, multiple authors4–6 have demonstrated significant anterior translation of the tibia with quadriceps contraction, particularly at 0 to 45 degrees of flexion. This anterior translation force is even greater when the quadriceps contraction is combined with a joint compressive force.4 These findings are the basis for ACL prevention strategies that emphasize proper biomechanics to address proper landing kinematics (hip and knee flexion while avoiding genu valgum), increase peak flexion angles, and improve hamstring activation and strength.
Nevertheless, a number of common elements tie these programs together. Most include one or more of the following: traditional stretching, strengthening, awareness of high-risk positions, technique modification, aerobic conditioning, sports-specific agility, proprioceptive and balance training, and plyometrics. The relation of these components to specific risk factors for ACL injury has been summarized in Table 5-1.
Table 5-1 Potential Biomechanical Deficits and Suggested Interventions
| Position | Intervention Strategy | Method of Intervention |
|---|---|---|
| Extended knee at initial contact | Knee flexion | Concentric hamstring control and soft landing |
| Extended hip at initial contact | Hip flexion | Iliopsoas and rectus femoral control and soft landing |
| Knee valgus with tibial-femoral loading | Address dynamic control, decrease dynamic valgus | Lateral hip control upon landing |
| Balance deficits | Proprioception drills | Dynamic balance training |
| Skill deficiency | Improve agility | Agility drills to address deceleration techniques and core stability |
Results of Studies Published to Date
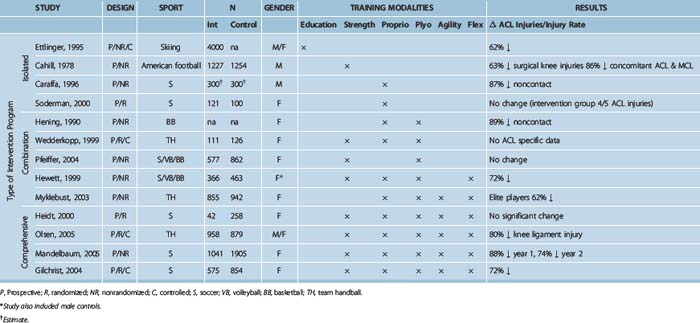
In an attempt to analyze existing ACL prevention programs, the studies are grouped and reviewed by their approach to injury prevention, beginning with the more global interventions and working up to the more comprehensive programs. Ettlinger et al25 looked at the effectiveness of an educational program to prevent ACL injury among downhill skiers by increasing awareness of injury mechanism and avoidance. Several studies have looked at the effect of isolated proprioception training on ACL injury risk, whereas a slightly more involved approach included neuromuscular training in landing and cutting techniques. Another pair of studies looked at the efficacy of technique training coupled with strengthening. Several more studies used a combination of neuromuscular training modalities. Finally, a number of studies have used a comprehensive approach to prevention of ACL injury, working on strength, flexibility, and agility as well as proprioception and plyometric training. The studies to date are summarized in Table 5-2.
Education
Ettlinger et al25 used a relatively simple approach to prevention of ACL injury in downhill skiers, attempting to modify high-risk–related behavior through education and increased awareness. In this prospective nonrandomized trial, 4000 on-slope alpine ski instructors and patrollers in 20 ski areas completed training and reporting requirements during the 1993–1994 ski season. The training kit included a 19-minute ACL awareness training videotape that showed 10 recorded ACL injuries sustained by alpine skiers of various levels, as well as various written materials. The videotape used guided discovery, allowing viewers to visualize carefully selected stimuli and incorporate this information into their skiing to avoid high-risk behavior and manage high-risk situations to reduce the risk of ACL injury. Participants also underwent an awareness training session that included proper body positioning, understanding of the phantom-foot ACL injury mechanism, and strategies to avoid high-risk positions as well as effective reaction strategies.
Isolated Strengthening and Conditioning
Cahill and Griffith26 looked at the effect of incorporating weight training into preseason conditioning for high-school American football teams. Over the 4 years of the study, they noted a reduction in reported knee injuries and knee injuries that required surgery in the intervention group.
Isolated Proprioceptive Training
Two studies have looked at the effect of isolated proprioceptive training on ACL injury risk, both in soccer players. Caraffa et al27 conducted a nonrandomized prospective study with 600 semi-professional and amateur soccer players in Umbria and Marche, Italy. Twenty teams (10 amateur and 10 semi-professional teams; Group A) underwent proprioceptive preseason training in addition to their regular training session. The control group (Group B) consisted of 20 teams (10 amateur and 10 semi-professional teams) and continued training in their usual fashion. The intervention group (A) was subjected to a five-phase progressive balance training program consisting of the following: no balance board, rectangular balance board, round balance board, combination (rectangular/round), and a biomechanical ankle platform system (BAPS) board (Camp Jackson, MI). The duration/frequency was 20 minutes per day for 2 to 6 days per week, including a minimum of 3 times per week during the season. The groups were followed for 3 years, and the senior author evaluated all players with a potential knee injury.
Soderman et al28 conducted a randomized, prospective controlled trial looking at the effectiveness of a balance board training program to reduce injuries in female soccer players. A total of 13 teams in the Swedish second and third division participated in the study, with seven teams (N = 121 players enrolled, 62 completed) in the intervention group and six teams (N = 100 players enrolled, 78 completed) in the age- and skill-matched control group through one outdoor season. The intervention consisted of a 10- to 15-minute balance board training program in addition to regularly scheduled games and practices. The players were instructed to complete the program daily for 30 days and continue with three sessions per week thereafter. Injuries were assessed with regard to number, incidence, type, and location.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree