Introduction4
INTRODUCTION
Tissue reaction patterns
Patterns of inflammation
MAJOR TISSUE REACTION PATTERNS
THE LICHENOID REACTION PATTERN (‘INTERFACE DERMATITIS’)
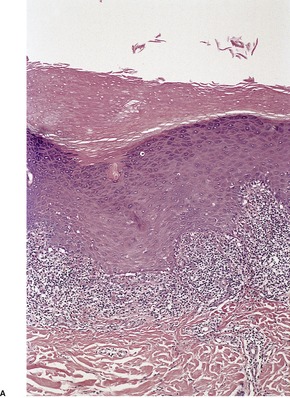
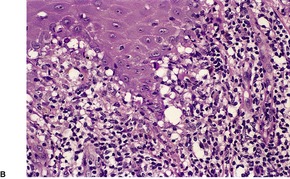
Fig. 1.1
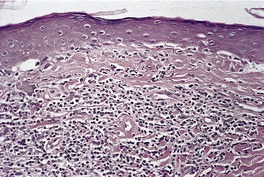
Fig. 1.2
Diseases marked * may have a true interface pattern.
Lichen planus
Lichen planus variants*
Lichen nitidus
Lichen striatus
Lichen planus-like keratosis
Lichenoid drug eruptions*
Fixed drug eruptions*
Erythema multiforme and variants*
Superantigen ‘id’ reaction*
Graft-versus-host disease*
Subacute radiation dermatitis*
Eruption of lymphocyte recovery
AIDS interface dermatitis
Lupus erythematosus*
Dermatomyositis
Poikiloderma congenita(le)*
Kindler’s syndrome
Congenital telangiectatic erythema (Bloom’s syndrome)
Lichen sclerosus et atrophicus
Dyskeratosis congenita
Poikiloderma of Civatte
Pityriasis lichenoides*
Persistent viral reactions
Perniosis
Polymorphic light eruption (pin-point type)
Paraneoplastic pemphigus
Lichenoid purpura
Lichenoid contact dermatitis
Still’s disease (adult onset)
Late secondary syphilis
Porokeratosis
Drug eruptions
Phototoxic dermatitis
Prurigo pigmentosa
Erythroderma
Mycosis fungoides
Regressing warts and tumors
Regressing pityriasis rosea
Lichen amyloidosus
Vitiligo
Lichenoid tattoo reaction
THE PSORIASIFORM REACTION PATTERN
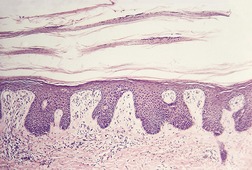
Fig. 1.3
Psoriasis
Psoriasiform keratosis
AIDS-associated psoriasiform dermatitis
Pustular psoriasis
Reiter’s syndrome
Pityriasis rubra pilaris
Parapsoriasis
Lichen simplex chronicus
Benign alveolar ridge keratosis
Subacute and chronic spongiotic dermatitides
Erythroderma
Mycosis fungoides
Chronic candidosis and dermatophytoses
Inflammatory linear verrucous epidermal nevus (ILVEN)
Norwegian scabies
Bowen’s disease (psoriasiform variant)
Clear cell acanthoma
Lamellar ichthyosis
Pityriasis rosea (‘herald patch’)
Pellagra
Acrodermatitis enteropathica
Glucagonoma syndrome
Secondary syphilis
THE SPONGIOTIC REACTION PATTERN
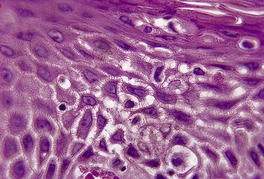
Fig. 1.4
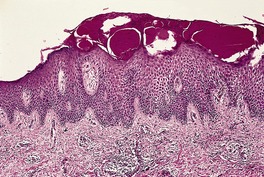
Fig. 1.5
Neutrophilic spongiosis
Pustular psoriasis/Reiter’s syndrome
Prurigo pigmentosa
IgA pemphigus
Infantile acropustulosis
Acute generalized exanthematous pustulosis
Palmoplantar pustulosis
Staphylococcal toxic shock syndrome
Neisserial infections
Dermatophytosis/candidosis
Beetle (Paederus) dermatitis
Pustular contact dermatitis
Glucagonoma syndrome
Amicrobial pustuloses
Periodic fever syndromes
Eosinophilic spongiosis
Pemphigus (precursor lesions)
Herpetiform pemphigus
Pemphigus vegetans
Bullous pemphigoid/cicatricial pemphigoid
Herpes gestationis
Idiopathic eosinophilic spongiosis
Eosinophilic, polymorphic, and pruritic eruption
Allergic contact dermatitis
Protein contact dermatitis
Atopic dermatitis
Arthropod bites
Eosinophilic folliculitis
Incontinentia pigmenti (first stage)
Drug reactions
‘Id’ reaction
Still’s disease
Wells’ syndrome
Miliarial spongiosis
Miliaria (may look pityriasiform on random section)
Follicular spongiosis
Infundibulofolliculitis
Atopic dermatitis (follicular lesions)
Apocrine miliaria
Eosinophilic folliculitis
Follicular mucinosis
Infectious folliculitides
Perioral dermatitis
Pityriasiform spongiosis
Pityriasis rosea
Pityriasiform drug reaction
Erythema annulare centrifugum
Allergic contact dermatitis
Nummular dermatitis
Lichen striatus (uncommonly)
Gianotti–Crosti syndrome (sometimes)
Other spongiotic disorders
Irritant contact dermatitis
Allergic contact dermatitis
Nummular dermatitis
Sulzberger–Garbe syndrome
Seborrheic dermatitis
Atopic dermatitis
Papular dermatitis
Pompholyx
Unclassified eczema
Hyperkeratotic dermatitis of the hands
Juvenile plantar dermatosis
Vein graft donor-site dermatitis
Stasis dermatitis
Autoeczematization (‘id’ reaction)
Dermal hypersensitivity reaction/urticarial dermatitis
Pityriasis rosea
Papular acrodermatitis of childhood
Spongiotic drug reactions
Autoimmune progesterone dermatitis
Estrogen dermatitis
Chronic superficial dermatitis
Perioral dermatitis
Blaschko dermatitis
Psoriasis (spongiotic and site variants)
Light reactions (particularly polymorphic light eruption)
Dermatophytoses
Arthropod bites
Grover’s disease (spongiotic variant)
Toxic shock syndrome
PUPPP
Herpes gestationis (early)
Erythema annulare centrifugum (not always pityriasiform)
Figurate erythemas
Pigmented purpuric dermatoses
Pityriasis alba
Eczematoid GVHD
Allograft rejection
Eruption of lymphocyte recovery
Lichen striatus
Lichen simplex chronicus
Sweet’s syndrome
Erythroderma
Mycosis fungoides
Acrokeratosis paraneoplastica
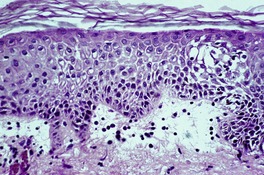
Fig. 1.6
Arthropod bites and bite-like reactions in lymphoma
Cercarial dermatitis/larva migrans
PUPPP
Autoeczematization
Superantigen ‘id’ reaction
Allergic contact dermatitis (‘dermal type’)
Contact urticaria, papular urticaria
Dermal hypersensitivity/urticarial dermatitis
Erysipelas, erysipeloid
Dermatophytoses
Prebullous pemphigoid
Sweet’s syndrome
Wells’ syndrome
Miliaria rubra
Pompholyx
Polymorphic light eruption
Spongiotic drug reactions (including estrogen/progesterone dermatitis) ![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


An approach to the interpretation of skin biopsies
Dermatopathology requires years of training and practice to attain an acceptable level of diagnostic skill. Many have found this process an exciting and challenging one, well worth the expenditure of time and intellectual effort. To the trainee, there seems to be an endless number of potential diagnoses in dermatopathology, with many bewildering names. However, if a logical approach is adopted, the great majority of skin biopsies can be diagnosed specifically and the remainder can be partly categorized into a particular group of diseases. This learning process can be enhanced under the tutelage of a skilled mentor and by ‘optical mileage’, a term used for the self-examination and diagnosis of large amounts of day-to-day material; such cases invariably differ from ‘classic’ examples of an entity found in teaching sets. It should not be forgotten that the histopathological features of some dermatoses are not diagnostically specific and it may only be possible in these circumstances to state that the histopathological features are ‘consistent with’ the clinical diagnosis.
The interpretation of many skin biopsies requires the identification and integration of two different, morphological features – the tissue reaction pattern and the pattern of inflammation. This is a crude algorithmic approach; more sophisticated ones usually hinder rather than enhance the ability to make a specific diagnosis.
Tissue reaction patterns are distinctive morphological patterns which categorize a group of cutaneous diseases. Within each of these histopathological categories there are diseases which may have similar or diverse clinical appearances and etiologies. Some diseases may show histopathological features of more than one reaction pattern at a particular time or during the course of their evolution. Such cases may be difficult to diagnose. In this edition, an attempt has been made to list diseases which characteristically express more than one tissue reaction pattern (see below).
The pattern of inflammation refers to the distribution of the inflammatory cell infiltrate within the dermis and/or the subcutaneous tissue. There are several distinctive patterns of inflammation (see below): their recognition assists in making a specific diagnosis.
Some dermatopathologists base their diagnostic approach on the inflammatory pattern, while others look first to see if the biopsy can be categorized into one of the ‘tissue reactions’ and use the pattern of inflammation to further categorize the biopsy within each of these reaction patterns. In practice, the experienced dermatopathologist sees these two aspects (tissue reaction pattern and inflammatory pattern) simultaneously, integrating and interpreting the findings in a matter of seconds. For trainees in dermatopathology, the use of tissue reaction patterns, combined with the mnemonic for diseases with a superficial and deep inflammatory pattern, appears to be the easiest method to master.
The categorization of inflammatory dermatoses by their tissue reactions will be considered first.
There are many different reaction patterns in the skin, but the majority of inflammatory dermatoses can be categorized into six different patterns. For convenience, these will be called the major tissue reaction patterns. Occasionally, diseases express more than one major pattern, either ab initio or during their evolution. They are dealt with separately in the ‘Combined reaction patterns’ section. There are a number of other diagnostic reaction patterns which occur much less commonly than the major group of six, but which are nevertheless specific for other groups of dermatoses. These patterns will be referred to as minor tissue reaction patterns. They will be considered after the major reaction patterns.
There are four patterns of cutaneous inflammation characterized on the basis of distribution of inflammatory cells within the skin:
1. superficial perivascular inflammation
2. superficial and deep dermal inflammation
3. folliculitis and perifolliculitis
4. panniculitis.
There are numerous dermatoses showing a superficial perivascular inflammatory infiltrate in the dermis and a limited number in the other categories. Sometimes panniculitis and folliculitis are regarded as major tissue reaction patterns, because of their easily recognizable pattern.
A significant number of inflammatory dermatoses can be categorized into one of the following six major reaction patterns, the key morphological feature of which is included in parentheses:
1. lichenoid (basal cell damage; interface dermatitis)
2. psoriasiform (regular epidermal hyperplasia)
3. spongiotic (intraepidermal intercellular edema)
4. vesiculobullous (blistering within or beneath the epidermis)
5. granulomatous (chronic granulomatous inflammation)
6. vasculopathic (pathological changes in cutaneous blood vessels).
Each of these reaction patterns will be discussed in turn, together with a list of the dermatoses found in each category.
The lichenoid reaction pattern (‘interface dermatitis’) (see Ch. 3, pp. 35–70) is characterized by epidermal basal cell damage, which may be manifested by cell death and/or basal vacuolar change (known in the past as ‘liquefaction degeneration’). The basal cell death usually presents in the form of shrunken eosinophilic cells, with pyknotic nuclear remnants, scattered along the basal layer of the epidermis (Fig. 1.1). These cells are known as Civatte bodies. They are undergoing death by apoptosis, a morphologically distinct type of cell death seen in both physiological and pathological circumstances (see p. 36). Sometimes the basal cell damage is quite subtle with only an occasional Civatte body and very focal vacuolar change. This is a feature of some drug reactions.
The lichenoid reaction pattern. (A) There are shrunken keratinocytes with pyknotic nuclear remnants (Civatte bodies) in the basal layer. These cells are undergoing death by apoptosis. (B) There is also focal vacuolar change. (H & E)
In the United States, the term ‘interface dermatitis’ is used synonymously with the lichenoid reaction pattern, although it is not usually applied to the subtle variants. Its use in other countries is by no means universal. At other times, it is used for the morphological subset (see below) in which inflammatory cells extend into the basal layer or above. The term is widely used despite its lack of precision. It is warmly embraced as a diagnosis, but it is nothing more than a pattern, encompassing many clinical entities with diverse presentations, etiologies, and treatments.
A distinctive subgroup of the lichenoid reaction pattern is the poikilodermatous pattern, characterized by mild basal damage, usually of vacuolar type, associated with epidermal atrophy, pigment incontinence, and dilatation of vessels in the papillary dermis (Fig. 1.2). It is a feature of the various types of poikiloderma (see p. 66).
The poikilodermatous variant of the lichenoid reaction pattern. It is characterized by mild vacuolar change of the basal layer of the epidermis, mild epidermal atrophy, and dilatation of vessels in the papillary dermis. (H & E)
The specific diagnosis of a disease within the lichenoid tissue reaction requires an assessment of several other morphological features. These include:
2. the distribution of the accompanying inflammatory cell infiltrate (the infiltrate touches the undersurface of the basal layer in lichen planus and its variants, early lichen sclerosus et atrophicus, and in disseminated superficial actinic porokeratosis; it obscures the dermoepidermal interface (so-called ‘interface dermatitis’) in erythema multiforme, paraneoplastic pemphigus, fixed drug eruptions, acute pityriasis lichenoides (PLEVA), acute graft-versus-host disease (GVHD), one variant of lupus erythematosus, and reactions to phenytoin (Dilantin) and other drugs; and it involves the deep as well as the superficial part of the dermis in lupus erythematosus, syphilis, photolichenoid eruptions, and some drug reactions);
3. the presence of prominent pigment incontinence (as seen in drug reactions, the poikilodermas, lichenoid reactions in dark-skinned people, and some of the sun-exacerbated lichen planus variants, e.g. lichen planus actinicus); and
4. the presence of satellite cell necrosis (lymphocyte-associated apoptosis) – defined here as two or more lymphocytes in close proximity to a Civatte body (a feature of graft-versus-host reaction, regressing plane warts, subacute radiation dermatitis, erythema multiforme, and some drug reactions).
The diseases showing the lichenoid reaction pattern are listed in Table 1.1.
From a morphological viewpoint, the psoriasiform tissue reaction (see Ch. 4, pp. 71–91) is defined as epidermal hyperplasia in which there is elongation of the rete ridges, usually in a regular manner (Fig. 1.3).
The psoriasiform reaction pattern showing epidermal hyperplasia with regular elongation of the rete processes. There are several layers of scale resulting from intermittent ‘activity’ of the process. (H & E)
It is acknowledged that this approach has some shortcomings, as many of the diseases in this category, including psoriasis, show no significant epidermal hyperplasia in their early stages. Rather, dilated vessels in the papillary dermis and an overlying suprapapillary scale may be the dominant features in early lesions of psoriasis. Mitoses are increased in basal keratinocytes in this pattern, particularly in active lesions of psoriasis.
The psoriasiform reaction pattern was originally defined as the cyclic formation of a suprapapillary exudate with focal parakeratosis related to it. The concept of the ‘squirting dermal papilla’ was also put forward with the suggestion that serum and inflammatory cells escaped from the blood vessels in the papillary dermis and passed through the epidermis to form the suprapapillary exudate referred to above. This ‘concept’, though outmoded, is useful in considering early lesions of psoriasis in which dilated vessels and surface suprapapillary scale are often the only features. The epidermal hyperplasia which also occurs was regarded as a phenomenon secondary to these other processes.
The spongiotic reaction pattern (see Ch. 5, pp. 93–122) is characterized by intraepidermal intercellular edema (spongiosis). It is recognized by the presence of widened intercellular spaces between keratinocytes, with elongation of the intercellular bridges (Fig. 1.4). The spongiosis may vary from microscopic foci to grossly visible vesicles. This reaction pattern has been known in the past as the ‘eczematous tissue reaction’. Inflammatory cells are present within the dermis, and their distribution and type may aid in making a specific diagnosis within this group. This is the most difficult reaction pattern in which to make a specific clinicopathological diagnosis; often a diagnosis of ‘spongiotic reaction consistent with …’ is all that can be made.
The spongiotic reaction pattern. There is mild intercellular edema with elongation of the intercellular bridges. (H & E)
The major diseases within this tissue reaction pattern (atopic dermatitis, allergic and irritant contact dermatitis, nummular dermatitis, and seborrheic dermatitis) all show progressive psoriasiform hyperplasia of the epidermis with chronicity (Fig. 1.5). This change is usually accompanied by diminishing spongiosis, but this will depend on the activity of the disease. Both patterns may be present in the same biopsy. The psoriasiform hyperplasia is, in part, a response to chronic rubbing and scratching.
The spongiotic reaction pattern in a lesion of some duration. Psoriasiform hyperplasia coexists with the spongiosis. (H & E)
Six patterns of spongiosis can be recognized:
1. neutrophilic spongiosis (where there are neutrophils within foci of spongiosis);
2. eosinophilic spongiosis (where there are numerous eosinophils within foci of spongiosis);
3. miliarial (acrosyringial) spongiosis (where the edema is related to the acrosyringium);
4. follicular spongiosis (where the spongiosis is centered on the follicular infundibulum);
5. pityriasiform spongiosis (where the spongiosis forms small vesicles containing lymphocytes, histiocytes, and Langerhans cells); and
6. haphazard spongiosis (the other spongiotic disorders in which there is no particular pattern of spongiosis).
The diseases showing the spongiotic reaction pattern are listed in Table 1.3(a).
A seventh pattern, which is really a variant of haphazard spongiosis, combines epidermal spongiosis with subepidermal edema (Fig. 1.6), which can vary from mild to severe, even forming subepidermal blisters. Its causes are listed in Table 1.3(b).
Epidermal spongiosis combined with subepidermal edema. This combination characterizes a certain group of diseases. (H & E)






