This chapter reviews key concepts that contribute to the aging process of the skin, steps to avoid future skin damage, basic treatment options for over the counter, and prescribed therapeutic options in the nondermatology setting.
BEAUTY AT A GLANCE
In the past decade, the aesthetic dermatology marketplace has undergone an explosive expansion. Despite recent and increasingly difficult economic times, the demand for cosmetic procedures to enhance, rejuvenate, or maintain beauty standards continues to grow. Since 2000, the Food and Drug Administration (FDA) has approved three neurotoxins and over twenty dermal filler devices, which are indicated for the treatment of soft tissue augmentation and temporary improvement of wrinkles associated with muscle movement and volume loss. The American Society of Plastic Surgeons (ASPS) reported that 1.1 billion dollars was spent on cosmetic procedures in 2012, which is a 5.5% increase from 2011, and office procedures performed by plastic surgeons grew by 10%. According to the ASPS, an estimated 14.6 million cosmetic procedures were performed in the United States in a medical office setting. Of the total estimated procedures, 1.6 million were defined as cosmetic surgical procedures, 13 million as cosmetic minimally invasive procedures (Table 23-1), and 5.6 million reconstructive procedures. Men and women, 40 to 54 years of age, are the largest demographic groups of the minimally invasive procedures, accounting for 48% of the cosmetic procedures. A 3% increase from 2011 was noted in minimally invasive procedures in females from the ages of 13 to 39. Females represent 91% of the paying consumers seeking cosmetic procedures, and males represent 9% of cosmetic procedures.
The accelerated growth of the overall beauty industry and the recent increase in the FDA approval of medical devices, dermal fillers, and neurotoxins have blurred the lines between traditional medical interventions, elective procedures, and beauty services. The brisk influx of products and services to the marketplace and the ever-increasing use of off-label indications of approved devices and therapies present a unique educational dilemma to establish competency for providers of aesthetic products and services.
The Dermatology Landscape
The specialty of dermatology has undergone a dramatic evolution over the past decade, including the introduction of aesthetic medicine. It is common for medical and surgical specialties, as well as individual providers, to claim expertise and ownership of lucrative cash-based aesthetic procedures and services. While there is no question that the demand for these services is present and the financial gains are obvious, it is imperative to have formal training, core competencies, and credentialing for providers to ensure safe and efficacious practice. Regardless of the clinician’s educational pedigree, the lack of competency specific to aesthetic services equates to an increased risk for poor outcomes and decreased safety for patients.
The science and art of aesthetics goes beyond the knowledge and skills of procedures and requires that clinicians assess and discern patients who are at risk for, or are suffering from, a psychiatric disorder. Patients seeking multiple aesthetic procedures have the highest risk for depression, anxiety, mood disorders, personality disorders, and body dysmorphia (BDD).
BDD is characterized by preoccupation with perceived appearance defect(s), with excessive concern over any slight physical anomaly, as well as significant distress or impairment in functioning that is not accounted for by a diagnosis such as anorexia nervosa. Because these patients have unyielding negative perceptions about their appearance, they are at risk for poly-procedures from multiple providers. When the clinician does not perceive the same defect or severity as the patient, it is a hallmark warning for BDD. Patients’ intrusive obsessions about their physical appearance can occupy an inordinate amount of their time and focus. The pervasive distortion can magnify poor self-image, esteem, avoidance, and interference with daily living. This can lead to extreme behaviors where they seek multiple procedures from different specialists. It can also include suicidal ideation.
Cosmetic Minimally Invasive Procedures Performed in the United States |
PROCEDURE | NO. OF PROCEDURES IN 2012 | CHANGE FROM 2011 (%) |
Botulinum Toxin Type A | 6.1 Million | 8 |
Soft Tissue Filler | 2 Million | 5 |
Chemical Peel | 1.1 Million | 2 |
Laser Hair Removal | 1.1 Million | 4 |
Microdermabrasion | 947,000 | 8 |
Adapted from American Society of Plastic Surgeons (2012).
When assessing a patient at risk for BDD, remember that he or she will engage in camouflaging behaviors such as body position and use of hats, hair, makeup, glasses, etc. Patients will often be distracted during an examination to gaze at themselves in reflective surfaces such as spoons, mirrors, or windows. Other patients may avoid mirrors as their reflection is so disturbing to them. Other obsessive compulsive behaviors, including skin picking, excessive exercising, and changing clothes repeatedly throughout the day, may be reported.
Clinicians must establish safe and strong boundaries with patients who have BDD by limiting their procedures. Be aware that patients may seek drastic alternatives such as buying products from the black market in an attempt to self-treat (Figure 23-1). Hence, a safe and successful aesthetic practice begins with a careful assessment of the patient’s motivation to enhance or modify their appearance long before the initiation of any procedure. Depression and anxiety screening tools can be incorporated into an assessment if there is any suspicion for BDD. A collaborative approach, including psychiatry and counseling, is recommended.
Clinicians practicing aesthetics should take note that despite high quality education, training, and good patient screening, aesthetic patients are known to be high risk for litigious actions. The result is increased premiums for professional malpractice insurance for clinicians providing cosmetic services.
FDA Intervention in Aesthetic Devices
In 2008, the device arm of the FDA convened a panel of dermatology experts to examine the increasing trends of adverse events (AEs) and serious adverse events (SAEs) reported as a result of soft tissue augmentation devices. Most of the AEs and SAEs reported were from off-label use of products (Dang, Francis, Durfor, Mirsaidi, & Shoaibi, 2008). The FDA advisory panel has recommended changes in the clinical trials process of products and the AEs reporting system. It also acknowledged that dermatology, as a specialty, had been scrutinized when in reality these devices were being used by many nondermatology physicians, nurse practitioners, physician assistants, and nurses. One of the panel’s recommendations was that manufacturers restrict the sale of their products to dermatologists and plastic surgeons. Many manufacturers require that a clinician have a valid Drug Enforcement Agency number and a state medical license to purchase their products.

FIG. 23-1. This patient was diagnosed with BDD and under a written agreement for treatment with both her treating dermatology clinician and psychologist. A: She presented with complications after purchasing 1 mL of dermal filler from the internet black market and self-injecting. The patient had an acute foreign body reaction to the unknown substance. B: Four weeks later, the swelling and inflammation have subsided but resulted in residual post inflammatory hyperpigmentation.
FDA Labeling
The reality of aesthetic services is that most procedures for soft tissue augmentation and neurotoxins are performed off label and lack the data or evidence required by the FDA to approve the product or device for both safety and efficacy. Although manufacturers may have clinical data that have been gathered and studied outside of the FDA approval processes, use of the product or device is still considered off label. It is both cost prohibitive and time sensitive for manufacturers to submit every indication to the FDA for approval. Accordingly, one must carefully weigh the risk versus benefits before deciding to perform procedures outside of FDA-labeled indications. This includes black-box warnings, contraindications, other warnings, and precautions. In the event of an adverse outcome, the assumption of legal risk is compounded.
ANATOMIC AND PHYSIOLOGIC IMPACTS ON THE AGING PROCESS
The skin ages in two distinct and biologically different processes. The intrinsic process refers to slow tissue degeneration that is uniquely influenced by an individual’s genetics and the process of time. This natural concept accounts for the differences in how individuals age. It usually begins during our mid-20s and continues throughout the life span (Figure 23-2).

FIG. 23-2. Wrinkles, gray hair, and “age spots” result from changes to the integumentary system that occur with aging, as shown across three generations of a family. Genetics, time, and extrinsic factors are key elements that influence an individual’s aging process. Although there is little ability to change the intrinsic factors, the impact of ultraviolet radiation on the skin can be reduced.
Intrinsic aging is characterized by several features (Table 23-2). Fibroblasts are the connective tissue cells that produce and secrete collagen (commonly referred to the scaffolding of our skin) and elastin fibers present in the dermis. Aging means changes in fibroblasts that result in the degeneration of elastin, which affects the skin’s ability to “stretch and recoil,” as well as maintains and repairs healthy cells. Decreased collagen synthesis and fragmentation cause dermal atrophy and loss of structure and elasticity. These changes are realized as wrinkles and textural changes in aging skin.
The loss of hydration also contributes to the process of aging skin. Hyaluronic acid, touted as a valuable ingredient in many commercially available moisturizers, is a large molecule in the dermis that has the ability to attract and hold water. It is described as being akin to a sponge that is able to hold over a thousand times its weight in water. Decreased levels of hyaluronic acid account for the changes in texture and elasticity and the wrinkles that come with age.
Extrinsic aging is a result of environmental factors and repeated exposures. The greatest influence on the degree of extrinsic aging is ultraviolet light radiation (UVR), which accounts for the classic appearance of “age spots” (Figure 23-3). Other external factors that prematurely age our skin include repetitive facial expressions (frowning, squinting, smiling, laughing); smoking; and pollution, gravity, and chemical exposures (Figure 23-4).
ULTRAVIOLET RADIATION
Understanding photobiology is essential to appreciating the role of UVR in photoaging, skin cancer, immunosuppression, and cataract formation. The sun emits energy over a wide range of spectrums. Unlike infrared radiation (visible light), UVR is neither seen by the naked eye nor felt. It has a shorter wavelength and possesses more energy than visible light. Other artificial sources of UVR exist and will be discussed.
There are three bands of UV radiation: UVA, UVB, and UVC. The stratospheric layer, or ozone, acts as a layer of protection from most of the sun’s UV exposure. UVC is completely absorbed by the ozone layer, while UVB is partially filtered, and UVA is without any filtration (Figure 23-5). Exposure to all types of UVR can have both beneficial and adverse effects on human health (Figure 23-6). This has led to vigorous debate in the scientific community as to the amount of UVR that is considered healthy. The U.S. Department of Health and the World Health Organization have classified UVR emitted from both natural and artificial light (sun and tanning beds) as a human carcinogen. The American Academy of Dermatology and Dermatology Nurses’ Association have taken a consistent stand on the harmful effects of tanning beds and are actively advocating for legislative limitations and regulations for the tanning industry.
Tanning is a form of self-defense against UVR. Depending on the individual’s skin type, there is an increase in melanin in the skin when exposed to moderate levels of radiation. The function of melanin is to absorb UVR and disperse the energy, minimizing the damaging effects to the skin (Figure 23-7). Yet the common urban myth of getting a base tan to reduce the risk of sunburn before an intense exposure (i.e., vacation) is a fallacy. It is important to note that a tan from UVA, such as tanning beds, will provide a tan by oxidizing that which was already present in the skin and signals the release of additional melanin from surrounding melanocytes. The resulting tan from UVA is cosmetic in nature and does not protect the skin from UVB exposure and sunburn. Unfortunately, the myth of the prevacation tan safety gives individuals a false sense of protection, leading to extended periods of sun exposure and risk.
Classification of Photoaging |
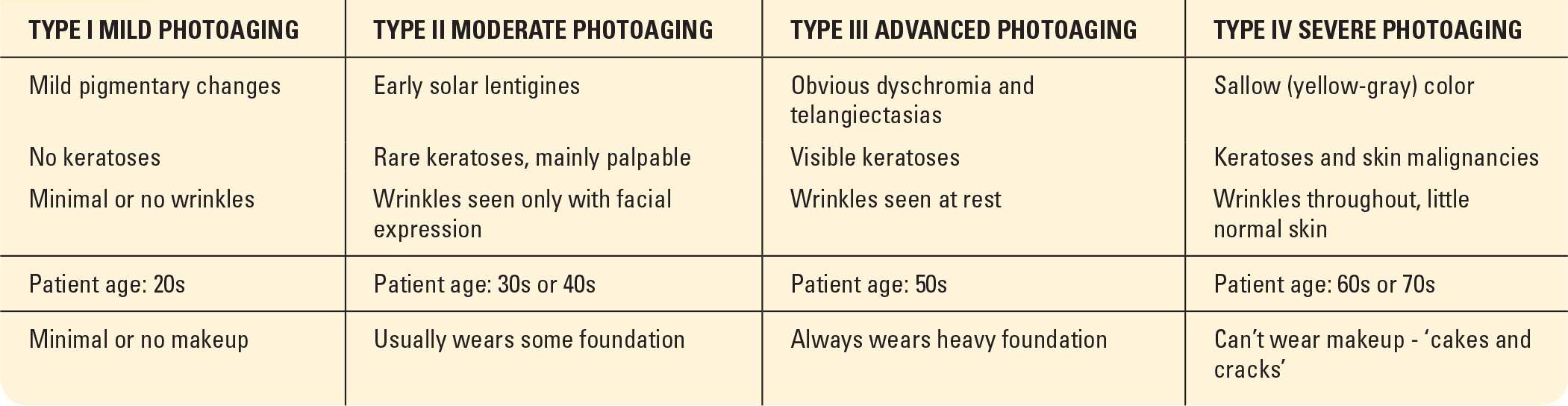
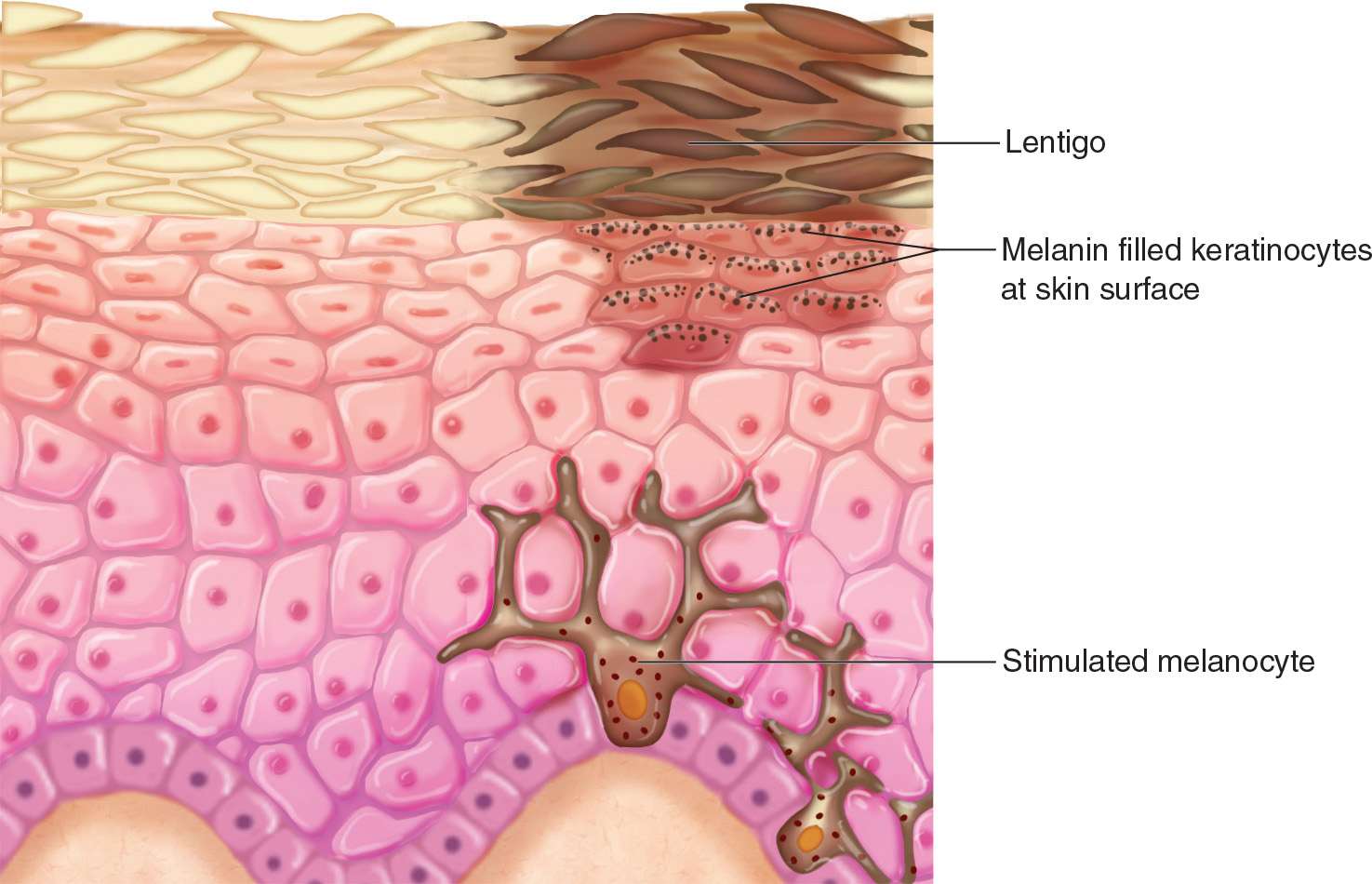
FIG. 23-3. Solar lentigos, also known as liver spots or age spots, typically appear on sun-exposed areas. Although they are characterized as age-associated skin changes, they can develop at a younger age with excessive ultraviolet radiation exposure.
Pathophysiology of Photoaging
Photoaging occurs when UVR activates the elastin promoter, which leads to an acceleration of abnormal elastin biosynthesis and accumulation in the dermis. Repeated UVR exposure impairs the biosynthesis of new collagen and increases the expression of matrix metalloproteinase (MMP) enzymes that break down collagen. UVA and UVB exposure also causes a vitamin A (retinol) deficiency which accelerates the aging process of skin. Histologically, UV-exposed skin reveals thickened and irregularly-shaped collagen bundles in the dermis. The physical manifestations of this change are referred to as solar or actinic elastosis.
Photoaging occurs over decades. With repeated exposure to the sun, the skin looses the ability to repair itself, and the damage accumulates. The resulting volume loss, skin laxity, fragility, and thinning are evident by the presence of fine lines and wrinkles, thinning skin, loss of underlying fat pads, loss of skin tone, and dry skin (Figure 23-8).
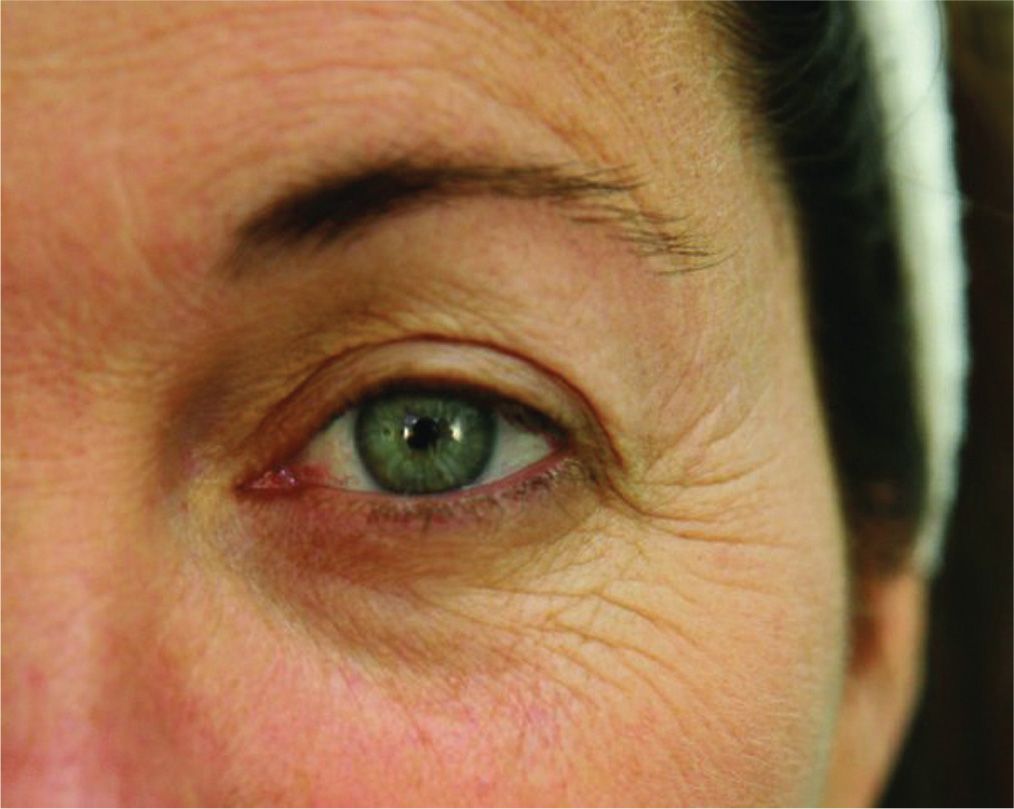
FIG. 23-4. Extrinsic aging from years of squinting manifests in rhytides, commonly called “crow’s-feet,” which are present at rest.
The patterns of photoaging are predictable, mostly on the sun-exposed areas of the hands, forearms, face, shoulders, chest, and upper back. Other clinical manifestations of photoaging are xerosis (rough and dry skin), mottled or spotty pigmentation, telangiectasias, static and dynamic lines, volume loss, follicular plugging, and the presence of benign or malignant neoplasms (Table 23-3). Altered elastin formation can cause the deposition of abnormal, yellow amorphous material that is incapable of forming functioning elastic fibers in the skin. The amount of photoaging that develops depends on a person’s skin color and their history of long-term or intense exposure. Individuals with fair skin that have a history of UV radiation develop more signs of photoaging than those with darker skin coloring. In darker skin, the signs of photoaging are usually limited to fine wrinkles and a mottled complexion.
Sun protection
While halting or arresting chronological aging is not yet scientifically possible, photoaging can be diminished with UV avoidance and sun-protection habits. Currently, there is no accurate way to measure UVA radiation blockage clinically because UVA alone does not cause the presence of erythema in the skin, which is a key component of sun protection factor (SPF) measurements. Despite this, it is important that effective sunscreens are broad spectrum and block both UVA and UVB to reduce the risk of skin cancers and premature aging (discussed in chapters 2 and 8).
Vitamin D synthesis
It is well known that UVB is needed for the synthesis of vitamin D, which is important for our health. However, research has not established the amount of sun exposure necessary to maintain adequate vitamin D levels. Many experts recommend 5 to 30 minutes of sun exposure on unprotected skin twice a week for adequate levels. The risk of carcinogenesis must always be weighed against the benefits of even limited amounts of UVA and UVB exposure.
Other Damaging Effects from UVR
Ocular damage
The most common cause of blindness in the world is due to cataracts. Evidence supports that UVR, especially UVB, is a known risk factor for developing cataracts. UVR also contributes to formation of pterygiums, skin cancers near the eye, and macular degeneration. The skin on the eyelid is the thinnest skin and is also the most susceptible to the effects of extrinsic aging (Figure 23-9
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree






