div class=”ChapterContextInformation”>
10. Technological Advancements to Promote Adherence
Keywords
AdherenceComplianceTechnologyMobile healthSmartphoneE-healthMonitoringInterventionsDermatologyIntroduction
Non-adherence to prescribed medications costs the United States $100–$290 billion USD annually [1]. It also costs lives; an estimated 125,000 deaths and over 10% of hospitalizations are due to non-adherence [2]. Physicians, other healthcare providers, and insurers have vested interests in improving non-adherence. There has been significant research and innovation surrounding the use of various health information technologies to improve adherence [3]. In particular, dermatology has high rates of non-adherence and has a vested interest in exploring technology as a means to improve patient adherence [4, 5].
Technology has become an integral part to how medicine is practiced from the electronic medical record to online communication between providers and patients to even e-prescriptions. In this fashion, technology is ubiquitous in the day-to-day of modern medicine. However, the use of technology as it relates to improving patient adherence is a relatively new concept [6]. Physicians, innovators, and businesspersons alike have delved into this rapidly growing domain of healthcare. These technologies may utilize internet networks, telecommunications, smart phones, physical devices/technologies, and more [7, 8].
In this chapter, we present and discuss some of the technological advancements in medication adherence that can be utilized in dermatology. Such a review may help patients overcome barriers to consistent use of their medications and aid providers in helping their patients improve their health.
Methods
A systematic review was conducted using PubMed to curate studies of technology use in promoting adherence or compliance in dermatology. Literature review was performed on February 27, 2019 for studies within the last 10 years (2009–2019) keeping in line with recent literature documenting advancements in this domain. Search terms in PubMed were ‘adherence’ OR ‘compliance’ AND ‘dermatology’. Titles and abstracts of all papers were read by two independent authors (V.R. and A.C.) for inclusion: (1) full-text manuscripts; (2) interventional clinical studies; (3) studies involving dermatology conditions or skin care (e.g. sunscreen use). Articles were excluded if: (1) interventions did not involve the use of some form of technology; (2) outcomes were not measured to allow for comparison between technology-use and standard of care groups; (3) full-text manuscripts not in English. Disputes were resolved via discussion with a third author (S.R.F).
Overall, 2011 manuscripts were identified by search criteria. After applying inclusion and exclusion criteria to titles and abstracts, 26 manuscripts were deemed appropriate for full-text review. During full-text review of manuscripts, an additional 3 manuscripts were removed based on inclusion/exclusion criteria, resulting in a final count of 23 manuscripts included.
In a non-systematic fashion, newer technologies without many trial data or ancillary studies were searched in a non-systematic fashion using PubMed and Google Scholar. Additionally, Google was used to identify websites discussing various companies’ technologies functioning within the realm of patient adherence.
Mobile Phone-Based Technology (mHealth)
Cell phones have become a ubiquitous technology used by two-thirds of the world’s population, piquing the interest in healthcare researchers and entrepreneurs in utilizing the technology to improve adherence [9]. The low costs and barriers to engage patients through mobile phone-based technology (mHealth) , especially in rural or underserved areas, is particularly intriguing to providers [9]. Text message reminders and phone-based applications are some of the most common reported methods aimed at improving patient adherence. For instance, a meta-analysis of randomized clinical trials of mobile phone text message reminders for patients with chronic diseases managed by internal medicine physicians has shown a near double in odds of medication adherence [10]. Dermatology has also investigated mHealth as a way to improve adherence.
Text Reminders
A randomized controlled study compared adherence in acne patients receiving text message reminders to control in 160 adults over the course of 12 weeks. Eighty patients were randomly assigned to receive two text messages daily (morning and evening) while 80 control patients did not receive any text reminders. Evaluation of patients during the 12-week study period included digital photographs, Global Acne Grading System (GAGS), Dermatology Life Quality Index (DLQI), and Cardiff Acne Disability Index (CADI). Adherence was assessed by seven-day recall questionnaire on the last week of treatment. From beginning to end of the study period, adherence in the text message group increased from 4.10 to 6.6 days/week compared to no significant increase in the control group (4.3–4.9 days/week) (P < 0.0001). GAGS score decreased significantly in the text message group (25.3 ± 8.9 to 8.7 ± 3.6) while there was no significant change in the control group (24.7 ± 7.6 to 16.2 ± 5.6) (P < 0.0001). DQLI scores in the text message group decreased significantly (9.2 ± 2.2 to 5.4 ± 1.8) compared to no significant change in the control group (9.5 ± 1.8 to 8.0 ± 1.4) (P < 0.0001). CADI scores similarly decreased significantly in the text message group (8.6 ± 1.3 to 2.0 ± 0.8) compared to the control group 7.8 ± 1.2 to 5.0 ± 0.8) (P < 0.0001). Additionally, 65% of patients were “very much satisfied”, 30% were “quite satisfied”, 4% “not much satisfied” and 1% were “not at all satisfied” with the text message service [11].
A randomized controlled multi-institutional trial compared adherence in acne patients receiving text message reminders to control in 33 healthy patients aged 12–35 years over the course of 12 weeks. Patients were randomized to experimental (n = 15) and control (n = 18) groups. The experimental cohort received customized twice-daily text message reminders to apply acne medication (clindamycin/benzoyl peroxide 1%/5% gel in the mornings and adapalene 0.3% gel in the evenings) while the control group received no such reminder. Electronic monitoring caps were used to assess adherence, the primary outcome measure. The secondary outcome measure was IGSA score and self-reported improvement of acne severity. Mean adherence rate for the text message reminder group was 33.9% compared to control group mean adherence rate of 36.5% (P = 0.75). Despite similar baseline IGSA scores, the text message reminder group had no significantly difference change in scores (2.3 to 1.2) compared to control group (2.4 to 1.6). Furthermore, mean self-reported improvement in acne severity was 55.3% in the text message group compared to 57.5% in the control group. When both groups’ data was combined, patients with higher individual adherence demonstrated greater decrease in acne lesion count by end of the 12-week study although this finding was not statistically significant (R2 = .0613) [12].
A randomized controlled trial compared adherence in children with atopic dermatitis and their caregivers receiving educational and reminder text message reminders to control in 30 children over the course of 42 days. Parents of both groups were provided a quiz at the initial visit and final follow-up visit to assess their knowledge of atopic dermatitis. Eczema Area Severity Index (EASI) scores were also measured at initial visit and follow-up. There was no significant difference in EASI score between the text message (−53% mean decrease) and control (−58% decrease) groups. However, the group receiving text messages scores significantly higher (84% correct) than the control group (75% correct) (P = 0.04) [13]. The authors surmise that the difference in scores were due to patients reading the text message reminders. However, a subjective or objective direct measurement of adherence was not performed but inferred.
A pilot study assessed adherence in atopic dermatitis patients receiving text message reminders and condition-specific educational information texts in 25 children 14 years of age or older over the course of 6 weeks. Outcomes measured included survey of treatment adherence (via 7-day recall and questionnaire assessing how often medication use was forgotten), survey of self-care actions (14 behaviors via Likert scale), disease severity (via SCORing Atopic Dermatitis index, SCORAD) , DLQI (17 and older) or Child Dermatology Quality of Life Index (CDQLI , 16 or younger), and usability/satisfaction (0 to 10 scale)with the text message reminder program. All pre-intervention measurements increased post-intervention. Specifically, treatment adherence (mean days/week) increased from 3.8 (SD 2.4) pre-intervention to 6.0 (SD 1.7) post-intervention (P < 0.001). Mean number (days/week) of self-care actions reported as “always” increased from 3.6 (SD 2.3) pre-intervention to 6.1 (SD 3.1) post-intervention (P < 0.002). Mean SCORAD decreased from 33.4 (SD 8.9) pre-intervention to 28.2 (SD 7.7) post-intervention (P < 0.001). Finally, DQLI/CDQLI decreased from 7.8 (SD 5.2) pre-intervention to 5.0 (SD 3.8) post-intervention (P < 0.014). The usefulness/satisfaction of the text message tool was graded as 7.1 (SD 2.4, range 2–10). 88% reported it as useful; 84% wanted to continue in the program; 92% found the educational texts helpful; 84% would recommend such a system to friends; and 72% would pay a small fee for the service [14].
A randomized controlled trial compared adherence in psoriasis patients receiving text message reminders compared to control in 40 patients over the course of 12 weeks. Evaluation of patients during the 12-week study included Psoriasis Area Severity Index (PASI), Self-Administered Psoriasis Area Severity Index (SAPASI), DLQI , Physician Global Assessment (PGA), patient-physician relationship questionnaire, and treatment adherence. The last outcome was evaluated through a series of multiple-choice questions assessing failure to use medications (days/week) with confirmation via 7-day recall calendar. The text message reminder group showed significantly increased treatment adherence (3.86 days/week to 6.46 days/week) compared to the control group which showed no significant change (P < 0.001). After 12 weeks, the text message reminder group had significant reduction in PASI (P < 0.05), SAPASI (P < 0.05), and PGA (P < 0.05) despite both groups having similar baseline values of each index score. Similarly, DLQI was significantly increased in the text message reminder group compared to the control group (P < 0.05). Likely as a result of the positive disease severity and quality of life scores, patients receiving text message reminders demonstrated improved patient-physician relationship scores compared to the control group, which had similar scores at the beginning and end of the 12-week treatment period (P < 0.01). Overall, 85% found text message reminders useful; 75% would recommend such a service to friends; 75% would continue with the text messages; and 15% would even pay a small fee for such a system to integrate with their psoriasis medications [15].
A randomized controlled trial compared adherence for sunscreen use in patients receiving text message reminders to control in 70 adult patients over the course of 6 weeks. Patients in the text message reminder group received daily reminders entailing a “hook” (regarding daily local weather) and “prompt” (reminder to use sunscreen). The primary outcome measured was adherence to sunscreen by the number of days used over the course of 6 weeks, which was measured by electronic monitoring device. Over the course of the 6 weeks, the text message reminder group maintained similar adherence at the start and end of the study, whereas the control group showed precipitous decline. Specifically, at the end of the 6-week period, the text message reminder group had mean adherence of 23.6 days (95% confidence interval [CI] 20.2–26.9 days) with daily adherence of 56.1% (95% CI: 48.1% to 64.1%) whereas the control group had mean adherence of 12.6 days (95% CI: 9.7–15.5 days) with daily adherence of 30.0% (95% CI: 23.1% to 36.9%). Statistical analysis of both mean adherence days and daily adherence percentages yielded P < 0.001. Although weekly adherence was similar after week one (50% in control group verses 58% in text message reminder group, P = 0.21), thereafter weekly comparisons of adherence were significantly different (P = 0.01 for week 2 and P < 0.001 for weeks 3–6). Sub-analysis of adherence on 8 rainy days (38% text message reminder group versus 9% control group) and 31 cloudy days (55% text message reminder group versus 30% control group) were also significantly increased in the interventional group (both P < 0.001). These results remained after controlling for demographic, educational, age, and other patient characteristics. A mean score of 8.31 (standard deviation [SD] of 1.99) out of 10 was reported for the utility of the reminder system (0 = not useful at all; 10 = most useful). 69% of participants would continue with reminders while 89% would recommend it to friends [16].
Another randomized controlled trial compared adherence to sunscreen use in three groups of patients (including one group receiving text message reminders) in 149 adults over the course of 12 weeks. All three groups received sun protection advice. Group 1 received 4000 HUF in compensation at the conclusion of 12 weeks. Group 2 received free sun protection factor (SPF) 50+ sunscreen. Group 3 (experimental) group received the SPF 50+ sunscreen and were sent personalized educational e-mails and text messages weekly. Adherence was measured by sun exposure diaries and interview results. Group 3 members used sunscreen more often (3.21 days/week ±2.37) than participants of Group 1 (1.47 ± 1.91) and Group 2 (2.09 ± 1.85) (P < 0.005 for both) [17].
Overall, it appears that the frequency of text messaging is not as important as the use of a reminder system itself. For instance, one of the prior mentioned studies showed twice daily text messages did not improve adherence [12]. Meanwhile, another study demonstrated merely weekly text message reminders were sufficient to improve adherence [17]. Too many notifications can lead to alarm fatigue. What may be most important is the context of the messages. A “hook” that provides value to the patient in a manner relative to behavior (e.g. weather or ultraviolet index) in addition to the reminder may be most effective [16].
Telecommunications/Mobile Phone Calls
A seemingly simple modality, phone calling is as accessible of a measure studied to improve adherence in our age of mobile phones.
An open-label, randomized study compared clinical improvement in 12 patients with atopic dermatitis who had previously failed topical corticosteroids under conditions designed to promote good adherence over the course of 7 days. Patients were given desoximethasone spray 0.25% as treatment. They were then randomized to control (n = 6) and experimental group (n = 6), which received twice-daily phone calls to discuss treatment adherence. Outcomes measured were the Pruritus Visual Analog Scale (PVAS), Total Lesion Severity Scale (TLSS), EASI, and Investigator Global Assessment (IGA). Overall, 100% (12/12) showed improvement in PVAS; 83.3% (10/12) showed improvement in EASI score; 75.0% (9/12) showed improvement in TLSS score; and 58.3% (7/12) showed improvement in IGA score. The interventional group receiving twice-daily phone calls showed greater improvement in all parameters compared to control group except for pruritus: PVAS (76.9% in interventional versus 87.0% in control); EASI (46.9% in interventional versus 21.1% in control); TLSS (38.3% in interventional versus 9.7% in control); IGA (45.8% versus 4.2% in control). These dramatic differences were attributed to increased adherence to treatment regimen as a result of phone call reminders [18].
A randomized controlled trial compared adherence in psoriasis patients receiving motivational phone calls compared to control in 177 adults over the course of 6 months. The motivational phone calls were administered at three points during the study (weeks 2, 8, and 16). Outcomes measured were PASI, adherence, and proper application of medication. Baseline characteristics between the two groups were similar. Improvement in PASI was seen in both motivational phone call group (6.8 to 4.8, P < 0.001) and control group (7.0 to 5.5, P < 0.001). However, there was no statistically difference in reduction between the groups upon completion of the study (P = 0.136). No statistically significant difference was seen between the groups to either topical (P = 0.278), scalp (P = 0.250), or systemic therapy adherence (P = 0.975). However, sub-analysis demonstrated patients’ proper administration/application of treatment was significantly improved in the motivation phone call group (82.4%) compared to the control group (67.4%) (P = 0.021) [19].
An open-label randomized controlled trial comparing adherence in acne patients undergoing different modalities of reminders to control in 46 teenagers was conducted over the course of 12 weeks. All 46 patients were treated with once-daily adapalene gel 0.1%. Four interventional groups were created: Group 1 (standard of care); Group 2 (frequent office visits: weeks 1, 2, 4, 6, 8, and 12); Group 3 (patients received daily phone call reminders); and Group 4 (parents received daily phone call reminders). Adherence was monitored by electronic monitoring caps. Adherence decreased over the study period for all groups. However, the overall difference in adherence was different between the four groups (P < 0.05). Group 2 has the highest median adherence (82), followed by Group 1 (59%), Group 3 (48%), and Group 4 (36%) [20].
Smartphone Applications
A randomized controlled trial compared adherence in 134 psoriasis patients using a smartphone application to control was conducted over the course of 28 days. The results of this trial are pending publication. Highlighted are principles of the investigation. In this trial, all patients were treated with topical calcipotriol and betamethasone dipropionate. The application under investigation is a combination of an electronic monitoring unit linked to a smartphone application. The three functions it is meant to serve are: a) provide patients with data on medication consumption; b) measure severity of psoriasis by completing a symptom and photo diary via the application; and c) support patients via reminders to refill medications and optional educational and motivational text messages. Primary outcome measures were rates of adherence measured by patient self-reporting, weight of medication, and electronic monitoring unit data. Secondary outcomes were DQLI and Lattice System Physician’s Global Assessment (LS-PGA) scores [21].
Investigation in other fields have showed mixed results. For instance, a randomized controlled trial compared adherence to antidepressant medications in 40 college students who were reminded via a smartphone reminder app (n = 20) or control (n = 20) over the course of 8 weeks. The primary outcome measure was adherence to the medication as measured by dividing the actual number of pills taken by the expected number of pills taken during the study period and multiplying the total by 100. Secondary outcomes included depression scores as measured by Beck Depression Inventory (BDI). Results showed the reminder app group patients were nearly 3.5 times more likely to adhere to their regimen than control group patients; however, these results were not statistically significant (P = 0.057). Similarly, the reduction in BDI scores were not significantly different between interventional (5.50 ± 8.34) and control (3.30 ± 5.40) groups (P = -0.374) [22].
Weekly treatments may be more difficult for patients than daily medications. Smartphones are capable of setting reminders based on standard features already available without additional application downloads. For instance, alarm reminders may be set at a specified time or a reminder notification may be delivered through text form via the reminder icon built-in application on smartphones [23].
It appears reminder apps seems to lose efficacy over time when reminders become ignored. In order to optimize long-term use, such apps may need to use a “hook” to capture patients’ attention with a follow-up “reminder” or link reminders to daily behaviors. Additionally, in-productive and recently released are applications created by pharmaceutical companies to serve as reminder systems. It may be prudent for clinicians and researchers to formally assess their utility and design moving forward.
Electronic Health (eHealth)
While eHealth caries similarities to mHealth and overlap may exist (especially with the use of mobile phone technologies to access Internet-based programs), eHealth is much more concerned with the use of computers and networks in healthcare. Use of such components of technology have been used in dermatology to promote adherence.
Web-Based Patient Education
A randomized controlled study comparing knowledge of condition and self-reported adherence in psoriasis patients receiving a web-based psoriasis education application to control in 22 patients was conducted during single office visits. A new training module was developed on DermPatientEd.com, a dermatology patient education webpage, to have an educational video regarding psoriasis, text-based content, and graphics on side effects. During the first clinic visit, patients were randomized to receive a link to the webpage followed by administration of an online quiz or solely access to the online quiz. Outcomes measured were quiz score and self-reported adherence. The web-based education group had a mean score of 11/14 on the psoriasis knowledge quiz compared to the control group mean score of 9/14 (P = 0.007). However, no improvements in self-reported medication adherence were observed [24].
A randomized controlled study compared adherence to sunscreen protection in 93 adult patients receiving online video education to control over the course of 12 weeks. Outcomes measured were assessment of sun protective behavior (using the National Health and Nutrition Examination Survey, NHANES), assessment of sunscreen knowledge (using questionnaire), and satisfaction survey (10-point scale). The experimental cohort received access to the online video, which discussed the mechanism of sunscreens, types of sunscreens, their importance, and proper application. The control group received the same information but as a pamphlet. Over the 12-week study, the online video group showed significant increase in adherence (days/week) to sunscreen use (1.7 ± 2.5 to 3.4 ± 2.6) (P < 0.005), unlike the pamphlet group (2.0 ± 3.0 to 2.4 ± 3.0) (P = 0.552). There was also a significant difference in the knowledge score increases between the online video group (2.0 ± 1.5) compared to the pamphlet group (1.2 ± 1.0) (P = 0.003). Finally, the online video group was significantly more satisfied with their education material (9 ± 0.9) compared to the pamphlet group (7.9 ± 1.3) (P < 0.001) [25].
A randomized controlled trial compared the utility of appearance-based video or a health-based video promoting sunscreen use in 50 high school students aged 13 and older. The appearance-based video focused on the negative effects of ultraviolet radiation (e.g. photoaging, wrinkles, sagging skin, uneven tone) whereas the health-based video focused on skin cancer risk and similar concepts. The production quality of both the appearance-based video (7.8 ± 1.3) and the health-based video (8.1 ± 1.3) were similar (P = 0.676). The satisfaction survey was administered 6 weeks after viewing the video. Mean satisfaction score for the appearance-based video (8.1 ± 1.2) was significantly higher than the health-based video (6.4 ± 1.4) (P < 0.001). Additionally, the mean appeal score for the appearance-based video (8.3 ± 1.0) was significantly higher than the health-based vide (6.6 ± 1.6) (P < 0.001) [26]. These authors also conducted a randomized controlled trial in the same patient population compared adherence to sunscreen based on appearance-based or health-based video education. While the health-based group showed a non-statistically significant increase (measured as days/week) in sunscreen use (0.9 ± 1.9, P = 0.096), the appearance-based group had a statistically significant increase (2.8 ± 2.2, P < 0.001). Inter-group comparison showed that the appearance-based group has significantly higher frequency of sunscreen use compared to the health-based group (2.2 ± 1.4 vs 0.2 ± 0.6, P < 0.001) [27].
A randomized controlled trial compared symptom improvement, quality of life, and adherence in 95 high school acne patients receiving automated online counseling to control standard website over the course of 12 weeks. The automated online counseling was an online module system that provides pre-recorded answers to an abundant number of specific questions patients may have. Outcomes measured were assessments of acne severity, quality of life (CDLQI), and skin care behavior. The automated online counseling webpage had the same information as that found in the standard website. There was not a significant difference in the reduction of acne lesions (mean) between the standard website group (21.33 ± 10.81 to 21.13 ± 14.42) and the automated-counseling website group (25.33 ± 12.45 to 21.43 ± 10.69) (between groups P = 0.10). Similarly, there was not a significant difference in the reduction in CDLQI scores between the standard website group (2.72 ± 3.19 to 2.54 ± 2.78) and the automated-counseling website group (2.69 ± 3.28 to 2.31 ± 2.99) (between groups P = 0.71). However, there was a significant difference in the percentage of patients in the automated-counseling website group (43%, 21/49) who maintained or recently adopted an anti-acne skin care program compared to the standard website group (22%, 10/46) (P = 0.03) [28].
Internet-Based Surveys
A randomized controlled trial compared treatment outcomes in 15 acne patients receiving Internet-based surveys compared to control over the course of 12 weeks. All patients were treated with daily topical benzoyl peroxide, 5% gel. The survey group received weekly surveys via e-mail with questions gauging adherence, ease of treatment regimen, efficacy, and side effects experienced. Adherence was also monitored objectively with electronic monitoring caps. Acne Global Assessment scores were used to score improvement at baseline, week 6, and week 12. Overall, the median adherence in the survey group was 74% compared to 32% in the control group (P = 0.01). Additionally, mean adherence dropped quickly (P = 0.02) while the survey group had no significant change in adherence over the study period (P = 0.10). The survey group also demonstrated greater decrease in acne severity as measured by non-inflammatory (44% versus 11%) and total lesion (36% versus 13%) counts, although these results were not statistically significant [29].
This concept has been translated into clinical practice by Causa Research, a company focused on targeting adherence issues facing physicians. Causa Research offers online survey platforms to improve patient adherence [30].
Teledermatology
A randomized controlled study comparing efficacy and adherence to actinic keratosis treatment in 157 patients undertaking care via teledermatology to face-to-face (i.e. in-person) visits was conducted over 4 weeks. Teledermatology visits began with the very first encounter for patients in the interventional group and then repeated at 4 weeks. All patients were prescribed 5% imiquimod applied three times per week. Eight weeks after beginning treatment, a blinded dermatologist assessed clinical response noted as partial, complete, or no response. Outcome measures were percentage of global response (complete response plus partial response) and reasons for treatment failure. Analysis was conducted under per-protocol and intention-to-treat parameters. Under per-protocol analysis, complete response was observed in 65.6% of teledermatology patients compared to 66.7% of face-to-face patients (P > 0.05). Under intention-to-treat analysis, complete response was seen in 51.2% of teledermatology patients and 64.0% of face-to-face patients (P = 0.073), Global response was improved in the face-to-face group (84.0%) compared to the teledermatology group (70.7%) (P = 0.036). However, multivariate analysis showed that the modality of care (face-to-face visits versus teledermatology) was not associated with global response but facial lesions and adverse events did. To assess adherence, reasons for failed therapy were assessed. Face-to-face patients completed the therapy 90.7% of the time compared to 72.0% in teledermatology patients. The major driven of treatment failure in teledermatology patients was not starting the therapy (47.8%) [31]. It is also worth noting, the 4-week study period is not the usual time span of treatment for actinic keratoses in daily practice. Typically, follow-up visits would occur much later.
However, it is plausible that a hybrid approach may exist in the future in which the initial visit is face-to-face (which may also avoid issues such as treatment initiation as noted in the prior mentioned study) with early follow-up via teledermatology to assess response and adherence.
Physical Technologies/Devices
Technology may come in the form of devices which may increase adherence. Typically, these devices serve as a mechanical means to assist, remind, or make it easier for patients to administer their treatments.
A randomized controlled study compared sunscreen adherence in an interventional group given combined sunscreen and toothpaste storage unit to control group (sunscreen only) in 62 Caucasian adult women over the course of 6 weeks. At the initial visit, all patients were advised of the benefits of sunscreen. Thereafter, patients were randomized into Group A (sunscreen only) or Group B (sunscreen + toothpaste storage unit). The outcome measure was difference in weight of sunscreen given at the initial visit (pre- minus post-study weight). The mean pre-weight of sunscreens was 112.2 g for all 62 patients. Group A sunscreen usage was 37.0 g (SD 17.2) while it was 44.1 g (SD 18.0) (P = 0.06). While the difference was not significantly different, it does represent a nearly 20% difference in use over the brief 6-week study [32].
A prospective study compared application success of compression stocking donning in 40 patients over 65 years old with chronic venous insufficiency randomized to order of compression stocking and donning device pairings. Compression stockings studied were one 40 mmHg or two superimposed 20 mmHg models. Donning devices were also studied. The endpoint of the study was successful donning of the compression stocking. Without donning devices, success rate for the one 40 mmHg stockings was 60% (24/40) and 70% (28/40) for patients donning the two superimposed 20 mmHg stockings (P = 0.220). With donning devices, the success rate for 40 mmHg stockings increased to between 88% (35/40; P = 0.001) to 90% (36/40; P = 0.002) depending on the donning device. Similarly, success rate increased to 88% (35/40; P = 0.016) for the two superimposed 20 mmHg stockings. These results were maintained even after controlling for patient characteristics associated with increased success (grip strength, P < 0.05; ability to access forefoot with hand, P = 0.001) [33]. The authors posit adherence is related to ability to don the garment and such devices would increase adherence.
A randomized, double-blinded, placebo-controlled, parallel-group trial compared adherence to secukinumab biologic treatment based on different administration modalities in 220 patients with moderate-to-severe psoriasis over the course of 48 weeks. Patients were assigned to secukinumab 300 mg, secukinumab 150 mg, or placebo at baseline (patients achieving PASI 75 at week 12 were continued on placebo or otherwise started on one of the other two regimens). All patients self-administered the medication or placebo via autoinjector. While the primary outcome of interest to the investigators was clinical efficacy (as measured by PASI and IGA), a secondary measure pertinent to this chapter was patient satisfaction and usability of the autoinjector device (measured by Self-Injection Assessment Questionnaire, SIAQ). This survey assessed feelings about self-injection, self-confidence, and satisfaction with self-injection. After completion of the 48-week study, SIAQ scores for the entire cohort were 8.92, 9.02 and 9.23 for feeling about injections, self-confidence and satisfaction with self-injection, respectively. These represented increases of 1.11 for feeling about injection, 1.70 for self-confidence and 2.52 for satisfaction with self-injection from baseline. 99.4% of patients reported that they were comfortable self-injecting at home (without staff supervision) using the auto-injector device even after the first administration [34].
Another apparent technology present in everyday life are smartwatches, which are increasingly being investigated for utility as medical care adjuncts. These devices are able to provide timely notifications to individuals. However, they lack formal scientific investigation to assess their impact on adherence behaviors.
Multimodal Approaches
A randomized controlled trial compared adherence in 1790 adult psoriasis patients undergoing a multimodal adherence program to control (standard of care) over the course of 64 weeks. All patients were treated with calcipotriol/betamethasone gel. The multimodal adherence program, named Topical Treatment Optimization Programme (TTOP), was comprised of five-elements: guidance for the conversation between dermatologists and patients, guidance for the conversation between nurses and patients, patient information material, telephone/e-mail helpdesks and treatment reminders. Outcomes measured were response to treatment (PGA score of 0 or 1 after 8 weeks of treatment) and patient-reported outcomes (DLQI and Topical Therapy Adherence Questionnaire [TTAQ]). From baseline to week 8, patients in the TTOP arm showed no significant difference in number of days of treatment use compared to the non-TTOP arm (53.5 ± 9.9 versus 53.5 ± 10.2 days). Patients in the non-TTOP group has higher mean use of study medication (adjusted for body surface area) compared to TTOP patients. Both groups showed large variations in usage highlighted by large SD. After 8 weeks, the percentage of patients attaining target response (PGA 0 or 1) was significantly higher for the TTOP group (36.3%) than the non-TTOP group (31.3%, P = 0.0267). After 8 weeks, the mean decrease in DLQI was similar between the TTOP group (2.6 ± 3.7) and non-TTOP group (2.2 ± 3.4). TTAQ responses were significantly higher in TTOP group patients who reported higher rates of feeling well-informed about their disease, treatment, and adherence-related factors (all P < 0.05). Despite the technologic aspects of the program (e.g. automated text message reminders), patients found structured one-to-one conversations with their providers as the most important in TTOP [35].
A multicenter, prospective, open-label interventional study compared efficacy and treatment adherence of a novel ultraviolet B home phototherapy system to control in six patients with stable plaque psoriasis over the course of 10 weeks. The primary outcome measures were Psoriasis Severity Index (PSI) and adherence. The compact technology allowed for home phototherapy and was synchronized to a smartphone application providing treatment plan information (schedule and dosing) and adherence data to the provider. Control lesions (n = 9) had mean change in PSI of 0.67 (95% CI: −0.27 to 1.61) compared to study lesions (n = 9), which had mean change in PSI of 4.44 (95% CI: 2.95 to 5.94) (P < 0.0002). Patient adherence was 96% and treatment satisfaction was 5/5 as rated by 100% of participants [36].
Emerging Concepts
Many of the previously discussed applications of technology to promote adherence pivot existing technological concepts towards tackling adherence issues in medicine and dermatology specifically. In this next section, we will highlight some of the emerging concepts in adherence research and technology that provide new avenues to apply these countermeasures. While many of these technologies are interesting takes on this age-old dilemma, it is important to bear in mind integration of such modalities is of utmost important. Otherwise, alarm fatigue, asynchrony between systems, and complexity of managing the technologies may lead to worse adherence.
Furthermore, integration of these technologies and concepts into the electronic medical record may proovc to be a boom for healthcare providers and their patients. By doing so, physicians can assess real-time adherence data and make calculated adjustments or changes to medication regimens. Furthermore, it may downstream aid insurance companies in stratifying risk and insurance premiums/costs for patients. And, most importantly, for patients it would allow for their physician to provide them with personalized and thorough management recommendations.
Gamification
Gamification refers to the concept of applying game playing features (e.g. points, competition) to other realms to promote engagement. This concept has been studied as a psychosocial principle that may be incorporated into technology to promote patient adherence. Literature on this topic is limited. Our literature review revealed 37 papers in PubMed; however, 7 were review papers (18.9%) and 26 (70.3%) were theoretical frameworks/description of app designs without intervention. Herein, we highlight one of the remaining studies, a randomized control study, within the scope of this chapter.
A randomized controlled trial compared intrinsic motivation and physical activity adherence in 36 patients with type 2 diabetes mellitus to control over the course of 24 weeks. Thirty-six inactive, overweight type 2 diabetes patients (45–70 years of age) were randomly assigned to the intentional group, which were instructed to play the smartphone app created by an interdisciplinary team, or control group. Primary outcome was intrinsic physical activity motivation measured by the Intrinsic Motivation Inventory (IMI). From baseline, intrinsic physical activity motivation (IMI score) increased significantly in the study group (+6.4, SD 4.2, P < 0.001) compared to the control group in which IMI score decreased (−1.9, SD 16.5, P = 0.625) (difference between groups, P = 0.029). This increase in IMI score in the interventional group was associated with increased usage of the app (P = 0.01; R2 = 0.34). Additionally, IMI score was associated with physical activity level, which was significantly higher in the interventional group compared to control group (P < 0.05) [37].
Gamification is an interesting principle that may be applied to adherence. It is a relatively novel concept, but has been highly utilized in the smartphone app space. A systematic review analyzing health and fitness apps related to physical activity and diet in the Apple App Store revealed 132 apps using concepts of gamification. Overall, 121/132 of the apps (91.7%) lacked citations or links to reputable sources to verify the health benefits and information claimed. Further evidence-based literature is needed to assess the utility of gamification [38]. Utilizing patients are resources in creation of these apps may be beneficial.
Automated Medication Dispensers
Traditionally, patients have utilized pill boxes or similar storage devices to medications to aid in daily adherence. While these serve as a memory device, they have shortcomings, such as lack of automation to facilitate memory.
A long-term, prospective feasibility study compared adherence in 21 elderly patients with chronic medical conditions with an automated medication dispenser to baseline adherence over the course of 6 months. All patients were referred by their primary care physician due to poor adherence and for inclusion in the study. Pill counts at baseline determined previous adherence, which was 49.0% for the cohort. Medication adherence was then assessed using an automated home medication dispenser. The dispenser is a bulk-loaded, single-patient medication tool designed to dispense scheduled and as-needed medications in residence. Audio and visual reminders are integrated into the device. Upon completion of the six-month study, adherence was measured at 96.8%, which was significantly higher than baseline (P < 0.001) [39].
The results of the prior study have inspired entrepreneurial ventures using this model. For instance, Pillo, Inc. is a company that has engineered a novel automated pill dispenser that combines concepts from machine learning, face recognition, video conferencing, and automation to serve as an overall in-home health assistant that also happens to dispense vitamins and medications [40]. Similarly, MySafeRx™ is a mobile technology integrating concepts such as motivational coaching, adherence monitoring, and electronic pill dispensing to manage office-based opioid treatment using buprenorphine/naloxone. It has demonstrated efficacy early on in a clinical trial before the adherence benefit was lost after conclusion of the study [41].
Some of these companies have technology integrating into medication packs monitoring adherence and provides alerts when doses are missed. Additionally, trusted family members may be notified to encourage adherence. These features may serve as cutting-edge countermeasures, although further research is needed.
Blister Pack Daily Medications
An innovative spin on the age-old distribution of medications, personalized daily medication blister packs are produced by some pharmacies to assist adherence. In this system, the patient’s pharmacy places daily medications into small packages labelled with the time and date for when the medications are to be taken. In doing so, it relieves patients of hassles such as personally obtaining medications (which are shipped), identifying them, sorting them, and remembering when in the day to take them (times are labelled on the package). However, this concept does have it shortcomings. It does not necessarily remove the rate-limiting step of patients (and particularly the elderly) remembering to take their medications.
Artificial Intelligence
Artificial intelligence (AI) is one of the hottest technology concepts in our modern world and its permeation into medicine has been inevitable. AI has the potential to assist physicians with diagnostics, procedures, and more. However, it also has a role in adherence.
Google LLC, for instance, has an artificial intelligence/natural language automated calling tool that is live in most of the United States. It is currently used to automate calls to book appointments and similar functions so that the user does not need to. It is not unreasonable to imagine such AI technologies could be educated to provide management recommendations for chronic diseases, call patients to confirm adherence to medications, and follow-up on questions patients may have about their regimens.
Conclusion
Adherence is among the most complicated issues physicians tackle in medicine. Technology has become a focal point in the battle against non-adherence. Many of these technologies utilize existing technologies that patients are generally familiar with (e.g. internet, smartphone apps, pre-existing smartphone reminder capabilities), allowing for ease in integrating these technologies. Other advancements may use new devices/technologies (e.g. at-home phototherapy) or pre-existing technology in a new context (e.g. gamification).
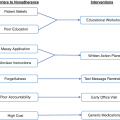
The evolving breadth of advancements in technologies promoting adherence is exciting for medicine and dermatology. However, it is important to realize, fundamentally, adherence is complex and concepts regarding behavior, psychosocial factors, and understanding are crucial regardless of intervention. This may, in part, explain why some of the newer technologies utilize behavior change/behavioral economics and psychological frameworks (e.g. gamification). Additionally, some of the largest barriers to adherence involve access to medication. Indeed, prohibitive costs, difficulties in navigating insurance, and inability to fill prescriptions at pharmacies are some of the largest barriers. Some initiatives have aimed to target such fundamental “gate-keeper” barriers that prelude medication adherence concerns in patients who have their medications [42]. Technological advancements seem to promote adherence despite some mixed results, but it is unquestionable that for any technology to function as expected a strong physician-patient relationship is needed as well as a thorough understanding of the factors contributing to individual non-adherence. Furthermore, patient preferences and characteristics that may limit participation in technologies (e.g. elderly) should be considered.
In other for these technologies to reach their full potential, integration between them and into the electronic medical record may be vital.
Conflicts of Interest
Mr. Vignesh Ramachandran, Dr. Abigail Cline, and Dr. Hawkins have no conflicts of interest to disclose.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree