Fig. 4.1
Adenosquamous carcinoma. An erythematous nodule with erosive surface on the upper arm
Pathology
ASC is a biphasic tumor with an epithelial malignant component of conventional SCC, merging with an epithelial malignant component of adenocarcinoma (Figs. 4.2 and 4.3). Histopathologically, the tumor consists of interlacing nests and cords of atypical squamous cells forming keratocysts and showing superficial epidermal connection, indicative of an epidermal origin. The adenocarcinomatous component ranges from focal to diffuse and consists of glandular and cystic spaces lined by cuboidal to low-columnar mucin-secreting epithelium containing mucicarmine and Alcian blue-positive material. A helpful histopathologic clue is the presence within glandular lumens of neutrophils and cellular necrotic debris. Perineural invasion is reported in 15 % of primary tumors and in 43 % of recurrences. Recurrent disease tends to occur in younger patients (mean age 65 years) and more frequently involves the face (43 %). There is a progressive transition and merging of the two cellular components, characterized by a keratin 7-/CEA + immunoprofile in the squamocellular counterpart and keratin 7+/CEA + immunoprofile in the adenocarcinomatous counterpart (Fig. 4.4). Both the squamous and glandular components stain positively with p63 (Fig. 4.5) and cytokeratin 5/6, suggesting a primary cutaneous origin.
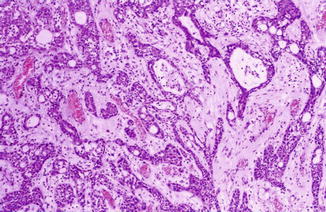
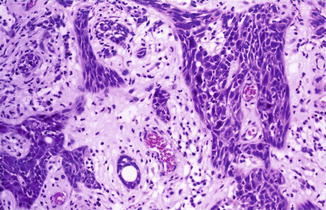
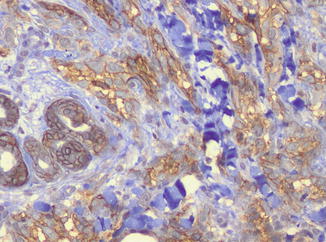
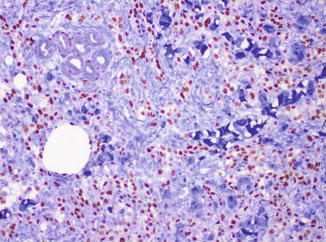
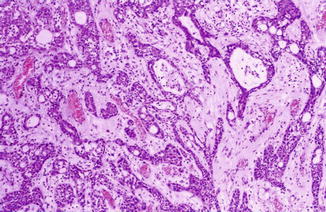
Fig. 4.2
The tumor consists of interlacing nests and cords of atypical squamous cells with glandular and cystic spaces
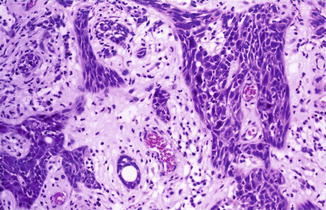
Fig. 4.3
The epithelial cords contain glandular lumens with clusters of mucin-secreting clear cells
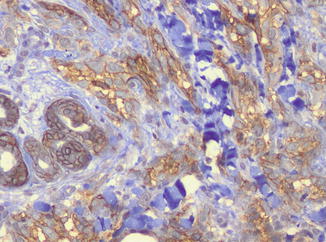
Fig. 4.4
The adenocarcinomatous component is stained by CEA
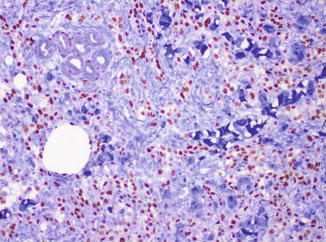
Fig. 4.5
Both the squamous and glandular components stain positively with p63
Differential Diagnosis
ASC should be histologically distinguished mainly from mucoepidermoid carcinoma. Although some authors consider ASC and mucoepidermoid carcinoma as the opposite extremities of a spectrum of the same entity, mucoepidermoid carcinoma shows slight different features consisting of low-grade appearing squamous cells intermingled with intermediate clear cells and mucin-secreting goblet cells. SCC with mucinous metaplasia is characterized by a component of conventional SCC with mucinous, PAS-positive, and Alcian blue-positive cells, not arranged in glandular spaces. Another differential diagnosis is with acantholytic squamous cell carcinoma that is characterized by pseudoglandular spaces due to acantholysis of dyskeratotic keratinocytes in the absence of true glandular formation and mucin-secreting cells. Invasive Bowen’s disease may show glandular differentiation, but ASC does not show typical changes of Bowen’s disease in the epidermis. Cutaneous metastases of visceral ASC may enter the differential diagnosis, but recently it has been reported that primary cutaneous neoplasms are diffusely p63 and cytokeratin 5/6 positive.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








