62
Acute Perilunate and Lunate Dislocations
Kevin D. Plancher
History and Clinical Presentation
A 30-year-old right hand dominant woman presents with swelling, pain, and deformity of the right wrist. The patient reports that while mountain biking, she fell on her outstretched hand. She reports no previous history of injury to her hand or wrist.
Physical Examination
Circulation of the hand and fingers was evaluated. A radial and ulnar pulse was verified as well as intact capillary refill of all fingers. A sensory and motor exam of the ulna and median nerve distribution was done. A dissociation between the distal radius and proximal carpal row was noted, and a palmar mass at the base of the hand was palpated.
Diagnostic Studies
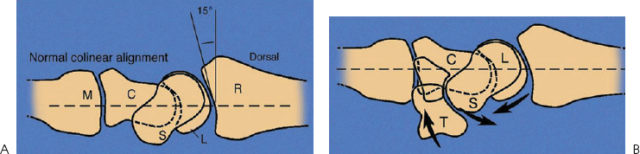
Lateral radiographs demonstrate dorsal displacement of the capitate (Fig. 62–1). The proximal pole of the scaphoid is rotated dorsally as the scaphoid palmar flexes (Fig. 62–2). Anteroposterior radiographs will verify the distal carpal row overlapping the proximal carpal row (Fig. 62–3). The scapholunate interval should be greater than 2 mm (Fig. 62–4).
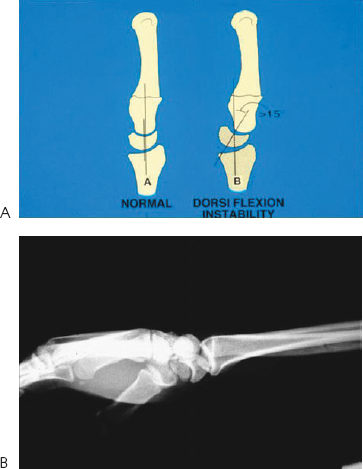
Figure 62–1. (A). Artwork of the typical appearance of the lateral radiograph in a scapholunate ligament tear. (B). Lateral radiograph that demonstrates a dorsal periluate dislocation (note the capitate and scaphoid are dorsal to the lunate with the lunate displaced volarly).
PEARLS
- An acute perilunate dislocation should be treated by operative intervention.
- Posttraumatic arthritis has been reported as high as 56% in surgically treated perilunate dislocations.
- Intraoperative radiographs facilitate avoiding poor reductions at surgery.
- Patient expectations must be discussed, including loss of use and permanent stiffness after a perilunate dislocation.
PITFALLS
- Delayed treatment may be due to missed diagnosis and will lead to adverse outcomes.
- Reduction of the joint surfaces is important to allow for normal wear of the cartilage.
- Scaphoid fractures associated with a perilunate dislocation must be treated to avoid a possible complication of nonunion.
Diagnosis
Acute Perilunate Dislocation
Perilunate and lunate dislocations often result from a fall on an outstretched hand (Fig. 62–5
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








