Acute Management: Tangential Excision and Skin Grafting
Yvonne L. Karanas
DEFINITION
Tangential excision of a wound is defined as the sequential removal of eschar in thin layers until healthy tissue is reached. Punctate bleeding of the underlying wound bed signals the presence of viable tissue and the end point of excision.
Tangential excision can be applied to any eschar of the skin in order to minimize the amount of tissue removed and preserve underlying viable tissue. It is most commonly used in burn surgery.
This procedure was first described by Janecovic in the 1970s and has been adopted worldwide by burn and plastic surgeons.1
A split-thickness skin graft is a piece of skin removed from the body for the purpose of covering a wound in another location. The outer portion of the skin composed of the epidermis and some portion of the dermis is “split” from the remaining underlying dermis. Enough dermis is left in the “donor site” for re-epithelialization.
A full-thickness skin graft is a piece of skin containing the “full thickness” of the epidermis and the dermis. Like a split-thickness graft, this piece of skin is removed from the patient and then transplanted to another site for wound closure or to add additional skin after contracture release. Unlike a split-thickness skin graft, no dermis is left behind so the wound must be closed primarily.
Allograft is broadly defined as a tissue graft from another human being. In burn care and surgery, it refers to human cadaver skin used to provide temporary wound coverage.
TBSA is Total Body Surface Area and refers to the amount of skin on the body that is burned.
ANATOMY
Burns and traumatic injuries can result in partial-thickness and full-thickness injuries. These terms refer to the depth of the injury into the skin.
Partial-thickness injuries involve the epidermis and some portion of the dermis.
Full-thickness injuries involve the epidermis and the entire dermis and can even include the subcutaneous fat.
PATHOGENESIS
Full- or partial-thickness skin necrosis may occur with trauma, burn injury, and severe soft tissue infections.
There are approximately 486 000 burn injuries per year in the United States with 40 000 requiring hospitalization.2
Worldwide, the magnitude of the problem is even greater.
NATURAL HISTORY
Burns or traumatic injuries may initially appear as superficial injuries, but with time (72-96 hours), they may progress to full-thickness injuries.
Judicious early debridement and serial wound care preserve all viable tissue while preventing wound infection.
When the wound evolution is complete, areas of full-thickness and partial-thickness burns should be clearly delineated. Definitive surgical treatment may then be performed as needed.
PATIENT HISTORY AND PHYSICAL FINDINGS
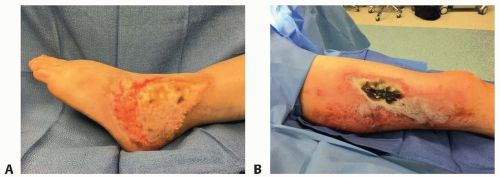
Full-thickness injuries may present as white, yellow, or brown leathery, insensate areas that lack capillary refill. With time, they will progress to a black eschar (FIG 1).
Partial-thickness injuries may be superficial with pink, moist, sensate tissue that has capillary refill.
Deep partial-thickness burns may be cherry red in color, lack capillary refill, have decreased sensation, and may be dry. These burns are often described as “indeterminate thickness” as it is often unclear initially whether they will require surgical treatment or not.
Burns and traumatic injuries may result in wounds that are a combination of different depths of injury (FIG 2).
NONOPERATIVE MANAGEMENT
Partial-thickness burns may be managed with wound care alone.
In general full-thickness skin, necrosis requires surgical treatment. It may be managed conservatively in select situations, for example, small wounds that are less than 1% TBSA on the torso. A large burn is commonly defined as a burn greater than 20% TBSA.
Wound care may be performed once or twice daily with silver sulfadiazine to soften and debride the eschar and prevent infection. Eventually the eschar will separate from the underlying wound bed; however, this process may take weeks or even months and lead to poor scarring and contractures.
For large wounds, an expectant management strategy carries a high risk of wound infection.
Surgical treatment remains the standard of care for large full-thickness wounds.
SURGICAL MANAGEMENT
Preoperative Planning
Equipment for Tangential Excision
Equipment for Skin Grafting
Dermatome electric or air powered
Guards of different widths (FIG 3C)
Mineral Oil
Tumescent solution: I L crystalloid, 1 cc (1:1000) epinephrine, 0.25% Marcaine (30 cc)
Klein Infiltration Pump—allows for high-volume infusion of tumescent solution in a rapid fashion
Tangential excision is performed using a variety of knives designed for this purpose, or a dermatome may be used.
The choice of instrument is based on the location of the wound and the size and thickness of the eschar. Small burns or burns in delicate areas such as the hands, face, or feet are excised with a Weck knife. Larger, thicker burns on the extremities or trunk are excised with a Watson knife. The depth of the excision can be set by adjusting the guard on the Weck knife or on the Watson knife itself.
The Weck knife has three guards that can be placed over the blade to control for the depth of excision: 0.012, 0.010, and 0.008 in. The selection of the thickness of the excision is based on the surgeon’s perception of the depth of the wound and the thickness of the skin in that region. The narrower guards of the Weck knife are used for less deep burns and areas of thin skin such as the dorsum of the hand, foot, or nose (FIG 3D).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree