88
Actinic Keratosis, Basal Cell Carcinoma, and Squamous Cell Carcinoma
Introduction
• NMSC typically refers to the keratinocyte carcinomas – i.e. basal cell carcinoma (BCC) and squamous cell carcinoma (SCC) – but can also include rare tumors such as Merkel cell carcinoma (see Chapter 95).
• ~75–80% of NMSCs are BCCs, and up to 25% are SCCs.
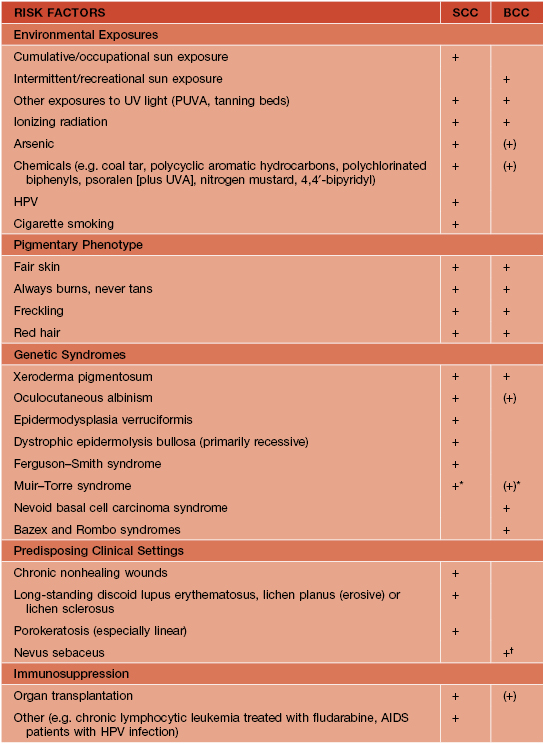
• The two most important risk factors for developing NMSC are skin phototype (see Appendix) and UV light exposure (Table 88.1).
Actinic Keratoses (AKs)
• The atypical keratinocytes are confined to the lower portion of the epidermis (Fig. 88.1).
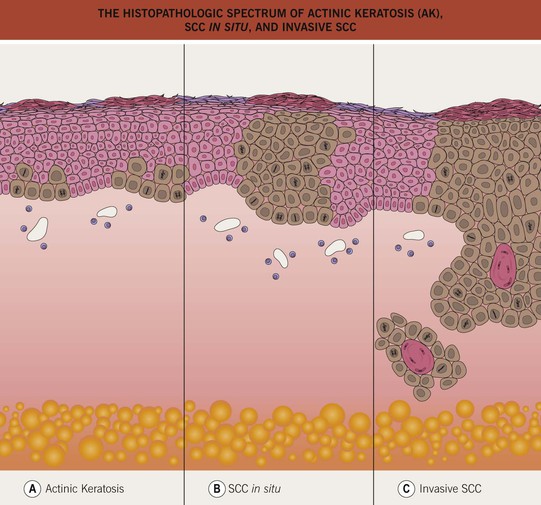
Fig. 88.1 The histopathologic spectrum of actinic keratosis (AK), SCC in situ, and invasive SCC. A An AK consists of a lower epidermal proliferation of cytologically abnormal keratinocytes; the adnexal epithelium is notably spared. B In SCC in situ, the atypical keratinocytes occupy the entire epidermis and intraepidermal portion of adnexal structures, without invasion into the dermis. C Invasive SCC is distinguished by the extension of the malignant keratinocytes into the dermis. If an invasive SCC is clinically suspected, the biopsy specimen should be deep enough to determine the extent of dermal invasion.
• AKs are one of the most frequently encountered lesions in clinical practice.
• Classic presentation is a gritty papule with an erythematous base; the associated scale is usually white to yellow in color and feels rough (Fig. 88.2).



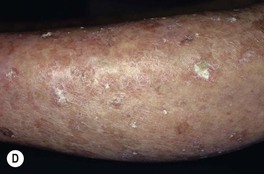
Fig. 88.2 Actinic keratoses (AKs). A Multiple AKs on the face of an elderly woman with fair complexion, blue eyes, and moderate to severe photodamage; the AKs vary in size from a few millimeters to more than 1 cm. On the left forehead, the red nodule with slight scale-crust represents a well-differentiated SCC. B Pink-colored atrophic AK with minimal scale on the forehead. C Multiple hypertrophic AKs on the bald scalp with hypopigmentation at sites of previous treatment. D Multiple, large hypertrophic AKs on the shin of an elderly woman; note the thick scale. A, C, Courtesy, H. Peter Sawyer, MD; B, Courtesy, Iris Zalaudek, MD; D, Courtesy, Jean L. Bolognia, MD.
• Common clinical variants: hypertrophic (referred to as HAK [Fig. 88.2C,D]), pigmented, lichenoid, and atrophic (Fig. 88.2B); in actinic cheilitis, there is scaling and roughness of the lower vermilion lip (see Fig. 13.5).
• DDx: SCC in situ, BCC, lichen planus-like keratosis (LPLK; see Chapter 89), irritated seborrheic keratosis (SK) or verruca vulgaris, and amelanotic melanoma; for thicker lesions (e.g. HAK), invasive SCC; for lesions on extensor extremities, actinic porokeratosis; occasionally, isolated lesions of psoriasis or seborrheic dermatitis may resemble an AK.
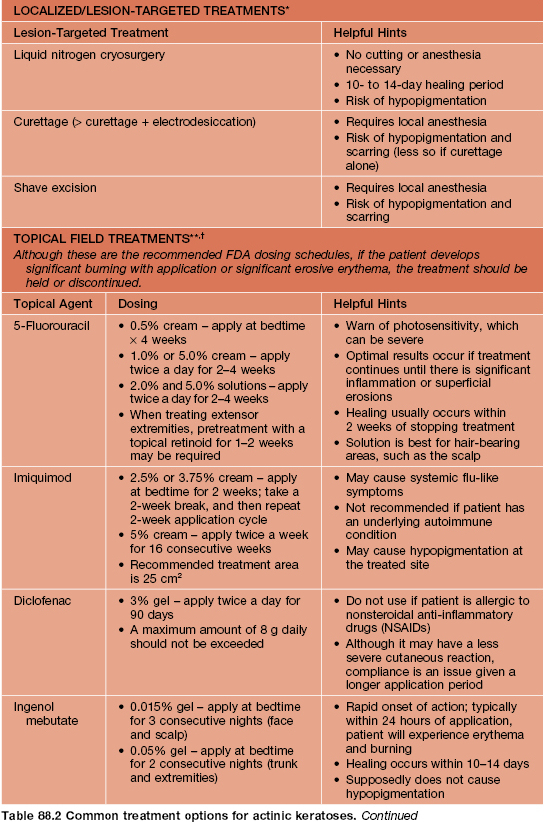
• Rx: localized or lesion-targeted treatments are best for an isolated or limited number of lesions; field treatments are best for more numerous or larger lesions (Table 88.2).
• Prevention is possible with broad-spectrum sunscreens and sun avoidance measures.
SCC In Situ (Bowen’s Disease)
• May arise de novo or from a pre-existing AK; sometimes caused by oncogenic strains of human papillomavirus (HPV, e.g. periungual [see Chapter 66]).
• Keratinocyte atypia is seen throughout the entire epidermis (full-thickness) (see Fig. 88.1) and has the potential to progress to invasive SCC, with an estimated risk of ~3–5% if untreated.
• With the exception of HPV- or arsenic-related SCC in situ, the risk factors for and the locations of SCC in situ are similar to those for AKs (see above and Table 88.1).
• Clinically presents as an erythematous patch or thin plaque with scale (Fig. 88.3); occasionally, the lesions are pigmented.




Fig. 88.3 Squamous cell carcinoma, in situ, Bowen’s type. A Scaly red plaque on the chest with skip areas. B Bright-red, well-demarcated plaque on the proximal nail fold with associated horizontal nail ridging; the possibility of HPV infection needs to be considered. C Dermoscopic examination of a pink scaly plaque of SCC in situ on the chest, with tiny dotted vessels in the upper half of the lesion combined with superficial scales. D Extensive involvement of the finger, which is often misdiagnosed clinically as psoriasis or chronic eczema and therefore treated for years with corticosteroid creams (as was this patient). C, Courtesy, Iris Zalaudek, MD; D, Courtesy, H. Peter Sawyer, MD.
• Less common sites (may be related to HPV infection): beard area, periungual (see Figs. 88.3B and 58.7) and subungual, anogenital (now referred to as intraepithelial neoplasia, further qualified by anatomic site [see Chapter 60 and Fig. 88.4]); SCC in situ in non-sun-exposed sites may also be related to arsenic exposure.