Chapter 12
Acne and Rosacea
OVERVIEW
- 80% of people living in developed countries suffer from acne at some stage in their lives.
- Acne lesions can be pustular and painful leading to scarring and psychological/emotional upset.
- Androgenic hormones increase sebum secretion and the numbers of Propionibacterium acnes.
- Exposure to oils/pomades, tar, agricultural chemicals and topical steroids can promote acne.
- Increased levels of oestrogen, testosterone, cortisol and growth hormone can trigger acne.
- Medications implicated in promoting acne include steroids, oral contraceptives, phenytoin, isoniazid, ciclosporin and lithium.
- Rosacea is characterised by facial flushing, persistent erythema, telangiectasia, inflammatory papules, pustules and oedema.
- Unlike acne, rosacea tends to start in adult life.
- Conjunctivitis, blepharitis and eyelid oedema may be associated with rosacea.
- Chronic oedema in rosacea can lead to gross thickening and hypertrophy of the nose called rhinophyma.
Introduction
Most adolescents in developed countries suffer from acne leading many to conclude that acne is a ‘normal’. However, the significant morbidity associated with it means it frequently has a negative impact on people’s lives. Acne, from the Greek word ‘acme’ meaning ‘prime of life’, suggests a disorder mainly during adolescence; however, this is somewhat misleading as acne can affect young infants through to individuals in their 40s and 50s. Indeed, over the past two decades the number of individuals who suffer from acne in later life has been increasing. Estimates show that 5% of the population over the age of 45 years still suffers from acne. Acne can have a significant psychological impact on patients regardless of its severity. Nonetheless, severe acne may, in addition, also be very painful, may cause irreversible scarring and may be associated with systemic symptoms including fever, joint pains and malaise.
What is acne?
Acne lesions develop from the sebaceous glands associated with hair follicles: face, back, chest and anogenital area (Figure 12.1). (Sebaceous glands are also found on the eyelids and mucosa, prepuce and cervix; however, they are not associated with hair follicles.) The sebaceous gland contains holocrine cells that secrete triglycerides, fatty acids, wax esters and sterols as ‘sebum’. The main changes in acne include
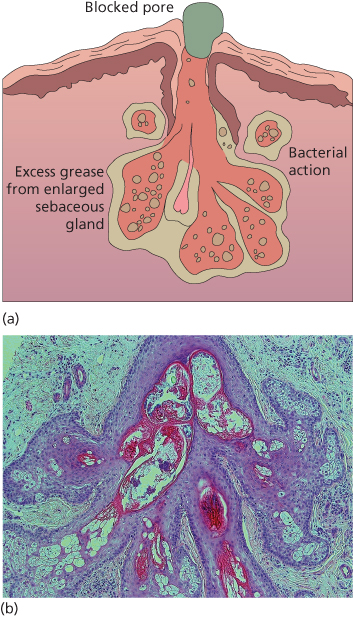
Figure 12.1 (a) Sebaceous gland: pathology in acne. (b) Histology of acne.
- thickening of the keratin lining and subsequent obstruction of the sebaceous duct resulting in closed comedones (‘whiteheads’) (Figure 12.2) or open comedones (‘blackheads’ whose colour is due to melanin, not dirt) (Figure 12.3). Acne cannot be diagnosed without the presence of comedones (there are no comedones seen in rosacea).
- an increase in sebum secretion.
- an increase in Propionibacterium acnes bacteria within the duct.
- inflammation around the sebaceous gland.

Figure 12.2 Acne with closed comedones.

Figure 12.3 Acne with open comedones, cysts and scars.
Underlying causes
There are various underlying causes of these changes (Box 12.1).
Hormones
Androgenic hormones increase the size of sebaceous glands and the amount of sebum in both male and female adolescents. Although
Box 12.1 Factors causing acne
Intrinsic factors
- Hormones
- Polycystic ovary syndrome.
- Virilising tumours.
- Congenital adrenal hyperplasia.
- Increased cortisol (Cushing’s syndrome).
- Increased growth hormone (acromegaly).
- Polycystic ovary syndrome.
- Medications
- Topical and systemic steroids.
- Oral contraceptive pill (higher androgen content).
- Phenytoin.
- Barbiturates.
- Isoniazid.
- Ciclosporin.
- Lithium.
- Topical and systemic steroids.
- Extrinsic factors
- Oils/pomades.
- Coal and tar.
- Chlorinated phenols.
- DDT and weed killers.
- Oils/pomades.
androgen levels may be normal there is thought to be an increased sensitivity of the glands to androgen hormones. In some women with acne, there is a lowered sex hormone-binding globulin concentration with a consequent increase in free testosterone levels. This change in the hormone balance is mimicked by many combined oral contraceptive pills (OCPs) resulting in increased acne. Oral contraceptives containing more than 50 µg ethinyloestradiol can also make acne worse. Oestrogens have the opposite effect in prepubertal boys and eunuchs. Infantile acne occurs in the first few months of life. It can rarely be caused by congenital adrenal hyperplasia or virilising tumours, but is most commonly due to transplacental stimulation of the adrenal gland by maternal hormones causing increased adrenal androgens.
Fluid retention
Premenstrual exacerbation of acne is thought to be due to fluid retention leading to increased hydration and swelling of the sebaceous duct. Sweating also makes acne worse, possibly by the same mechanism.
Stress
It has long been observed by patients that stress leads to a worsening of their acne. Now there is evidence to back up the clinical observation. Stress induces inflammation in the pilosebaceous unit leading to acne or acne exacerbation. There is evidence that within sebocytes is a complete corticotropin-releasing hormone system that leads to increased lipid and steroid synthesis and an interaction with testosterone and growth hormone.
Diet
Many patients believe their acne is exacerbated by eating certain foods. Most commonly implicated foods include dairy products, chocolate, nuts, coffee and fizzy drinks. Some epidemiological studies have suggested that a Westernised diet of high levels of refined sugars and starch may explain striking differences in the prevalence of acne amongst different populations that are not thought to be explained by genetic factors or weight differences. However, during studies when Westerners were fed a low glycaemic diet, there was no significant improvement in their acne.
Seasons
Acne often improves with natural sunlight. Phototherapy with artificial light sources using visible blue light alone or in combination with red light has been shown in several clinical trials to be an effective treatment for acne in a proportion of patients.
External factors
Oils, whether vegetable oils in the case of cooks in hot kitchens or mineral oils in engineering, can cause ‘oil folliculitis’, leading to acne-like lesions through contact with the skin. Other acnegenic substances include coal tar, dicophane (DDT), cutting oils and halogenated hydrocarbons. Cosmetic acne is seen in adult women who have used cosmetics containing comedogenic oils over many years. Individuals who use rich oils in the scalp can suffer from ‘pomade acne’, which occurs close to the hairline.
Iatrogenic factors
Corticosteroids, both topical and systemic, can cause increased keratinisation of the pilosebaceous duct resulting in acne. Androgens, gonadotrophins and corticotrophin can induce acne in adolescence. OCPs of the combined type and antiepileptic drugs may also cause acne. However, an OCP with a high oestrogen combined with low androgen can actually be used to treat acne in women. Some patients develop perioral dermatitis (Figure 12.4) after application of topical steroids to the face, which is characterised by papules and pustules around the mouth and eyes that may mimic acne but there are no comedones. The topical steroid should be stopped and the patient treated with oral tetracycline or erythromycin for 6 weeks.
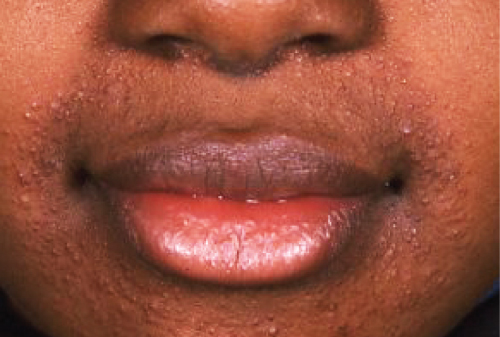
Figure 12.4 Perioral dermatitis.
Types of acne
Acne vulgaris
Acne vulgaris, the common type of acne, occurs during puberty and affects the comedogenic areas of the face, back and chest. There may be a familial tendency to acne. Acne vulgaris is more common in boys, 30–40% of whom develop acne between the ages of 18 and 19 (Figure 12.5). In girls, the peak incidence is between 16 and 18 years. Adult acne is a variant affecting 3% of men and 5% of women over the age of 40. Acne keloidalis is a type of scarring acne seen particularly on the neck in men (Figure 12.6; Box 12.2).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








