Ablative and Nonablative Resurfacing in Darker Skin
Henry H.L. Chan
Skin rejuvenation in dark-skinned patients differs in several important respects from that in Caucasians. In dark-skinned patients, photoaging is associated with more pigmentary problems but less wrinkling. As a result, laser resurfacing is less warranted.
Furthermore, dark-skinned patients have higher epidermal melanin content and are more likely to develop postinflammatory hyperpigmentation (PIH) following laser resurfacing. Nonablative skin rejuvenation is therefore more suitable for dark-skinned patients. More recently, fractional resurfacing—a new technique that is considered to be halfway between ablative and nonablative skin resurfacing—has been introduced. With the appropriate parameters, fractional resurfacing can be used effectively and safely in skin rejuvenation among darker-skinned patients.
Indication and Contraindication for Ablative and Nonablative Skin Resurfacing in Darker Skin
Darker-skinned patients have photodamage that presents with pigmentary problems but have less wrinkling than Caucasians. Chung et al. performed photographic assessment of 407 Koreans between the ages of 30 and 92 and assessed the manifestation of cutaneous damage.1 Their findings indicated that pigmentary changes are common features of photoaging in Asians, with seborrhoeic keratosis being the major pigmentary lesion in men and lentigine the prominent feature in women. Furthermore, laser resurfacing in dark-skinned patients is associated with more adverse effects, especially PIH.2 As a result, nonablative skin resurfacing is often the preferred option for most dark-skinned patients with photoaging. Ablative skin resurfacing is now used for those who fail to improve to their degree of satisfaction after nonablative procedure. Although acne scarring can also improve after nonablative skin resurfacing, the degree of improvement is often suboptimal, and ablative resurfacing remains the preferred treatment. More recently, fractional resurfacing has become a feasible alternative to ablative resurfacing for the treatment of acne scarring.
In terms of contraindications, patients who have been on systemic isotretinoin treatment should not receive laser resurfacing or fractional resurfacing for at least 6 months after the discontinuation of therapy. Topical retinoid should be stopped for 2 weeks before ablative and fractional resurfacing. In my experience, stopping systemic isotretinoin for a month is adequate for the nonablative procedure. A history of gold therapy and photodermatoses are other contraindications. Pregnancy should be considered as a relative contraindication. As PIH is the most common complication of laser surgery among darker-skinned patients, particular attention should be paid to factors that can increase it, such as sun exposure within 2 weeks of the surgery or the use of phototoxic agents, such as tetracycline.
The Use of Laser and Intense Pulsed Light Source for Treatment of Pigmentary Problems in Darker Skin
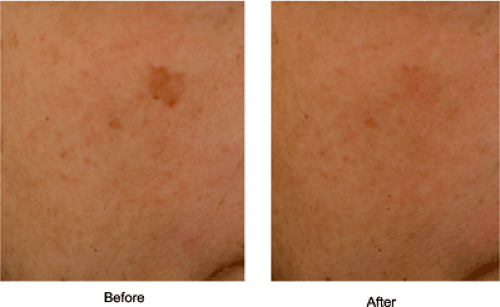
For many years, Q-switched (QS) lasers have been used to treat lentigines (Fig. 19-1), and although the approach is mostly effective, PIH occurs in 10% to 20% of darker-skinned patients. Several years ago, our group compared the efficacy and complication rates in Chinese patients treated with QS 532-nm neodymium:yttrium-aluminum-garnet (Nd:YAG) laser with those treated with long-pulsed 532-nm Nd:YAG laser and found that although the two groups had similar degrees of clearing, treatment with the QS device was associated with a greater risk of PIH.3 We created controversy when we proposed that QS lasers are not suitable for the removal of lentigines in Asians because of the photomechanical effect of these systems leading to a greater risk of PIH (the rapid change of
thermal gradient that is associated with the use of QS laser leads to the generation of localized shock waves within the target). Since then, others looking at the use of intense pulsed light source (IPL) and long-pulsed 532-nm Nd:YAG laser in the treatment of lentigines in dark-skinned patients have confirmed our hypothesis.4,5 By choosing a pulse width (minisecond domain) that matches the thermal relaxation time of the epidermis (10 miniseconds), the risk of thermal injury to the dermis is minimized (Fig. 19-2).
thermal gradient that is associated with the use of QS laser leads to the generation of localized shock waves within the target). Since then, others looking at the use of intense pulsed light source (IPL) and long-pulsed 532-nm Nd:YAG laser in the treatment of lentigines in dark-skinned patients have confirmed our hypothesis.4,5 By choosing a pulse width (minisecond domain) that matches the thermal relaxation time of the epidermis (10 miniseconds), the risk of thermal injury to the dermis is minimized (Fig. 19-2).
Most pigment laser/light source is also absorbed to a lesser degree by hemoglobin. Therefore, besides the use of long-pulsed rather than QS laser, another means to further reduce the risk of PIH is to compress and empty the dermal vessels and, in doing so, reduce the risk of dermal vascular damage.6 A recent study compared the efficacy and complication of QS ruby laser against long-pulsed 595-nm pulsed dye laser with a compression window attached for the removal of lentigines among Japanese patients. The group treated with the compression technique was associated with a lower risk of PIH than the group treated with QS laser, but the degree of efficacy was the same in both groups.7
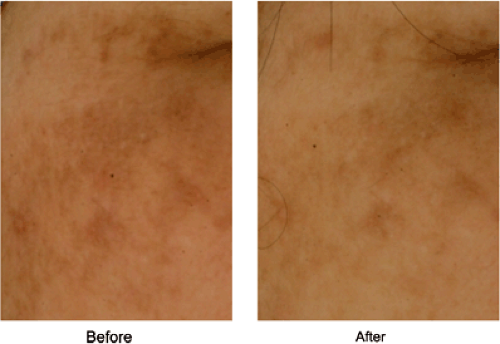 Figure 19-2 Lentigines after one treatment with long-pulse 532-nm Nd:YAG laser 2-mm spot size, 12 J/cm2 with contact cooling. |
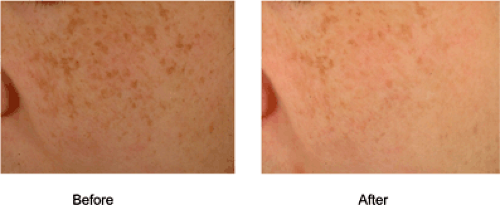 Figure 19-3 Lentigines after two treatments by intense pulsed light source (V-handpiece, Starlux, Palomar, 15 J/cm2, 40 milliseconds |
My current treatment approach is to use a long-pulsed laser (532 nm Nd:YAG) with an ashen-grey appearance as the clinical end point. A large spot-size second harmonic (532-nm) neodymium:yttrium-aluminum-garnet laser (Nd:YAG Gemini, Laserscope, San Jose, CA, USA) is one such device that can be used effectively to treat lentigines in darker-skinned patients (10-mm spot size, 20-millisecond pulse width, and 7 J/cm2 for one pass over the entire anatomic area, then 2-mm spot size, 2-millisecond pulse width, and 12 J/cm2 to individual lesions).8 Patients are warned that there will be mild postoperative crusting for 5 to 7 days. About three treatment sessions are necessary to obtain desirable clinical effects.
For clinicians with QS laser, the intention is to use the lowest possible fluence and the smallest spot size (and therefore spare the surrounding normal epidermis) to obtain immediate whitening. For QS laser, a test area is best performed to assess the risk of PIH. A test area also helps patients to understand the procedure and the degree of postoperative downtime. With patients for whom downtime is an issue, IPL can be used instead (Fig. 19-3). Depending on the type of IPL, four to six treatment sessions are usually necessary, and if the removal of lentigines is the main aim, IPL is less cost-effective. IPL has the advantage of improving other skin qualities, such as skin texture and telangiectasia. Although cooling is essential when dermal chromophobes, such as water or vessels, are targeted, for the removal of epidermal pigment, excessive cooling can reduce IPL-induced photothermal effects.
In all cases, a moderate-potency steroid mixed with antibiotic (mometasone furoate) is applied to the skin immediately after surgery to reduce the risk of PIH. Sun protection, sun avoidance, and the use of bleaching agents 2 weeks before and after any laser/IPL procedure also lower the risk of PIH.
Ablative, Nonablative Skin Rejuvenation and Fractional Resurfacing: Technique, Degree of Improvement, and Complication
Nonablative skin rejuvenation involves the use of a laser/light source together with a cooling device, and in doing so improves the features of photoaging, including lentigines, telangiectasia, pore size, skin texture, wrinkles, and skin laxity with minimal downtime. Patients typically experience a mild degree of erythema that usually lasts less than 24 hours and darkening of the lentigines immediately after surgery. Repeat monthly treatment, usually for 6 months, is necessary to obtain the desired effect. A wide range of lasers or light sources can be used for nonablative skin rejuvenation, including visible green-yellow (532-nm Nd:YAG, 585-nm or 595-nm pulsed dye laser), near infrared and infrared lasers (1,064-nm Nd:YAG, 1,320-nm Nd:YAG, 1,450-nm diode, 1,540-nm erbium glass), and IPL sources.
Green and yellow lasers/light sources target the epidermal pigment and papillary dermal vessels. Injury to the papillary dermal vessels not only allows effective treatment of facial telangiectasia, but also leads to the subsequent healing process and new collagen formation. Affecting the microvascular supply of the sebaceous gland can reduce sebum production and improve pore size. Because of the higher epidermal melanin content of darker-skinned patients, epidermal melanin acts as a competing target chromophore for hemoglobin, which means that skin cooling is essential when vascular lasers are used for skin rejuvenation. In my experience, long-pulse pulsed dye laser with dynamic cooling can be used safely in skin rejuvenation among dark-skinned patients (V-beam, 595 nm, 10-mm spot size, 7.5 J/cm2, 10 millisecond, Candela Corp., Wayland, MA, USA). Alternatively, large spot–size 532-nm Nd:YAG laser can be used, but swelling is more likely to occur, leading to longer downtime.
Near infrared and infrared lasers/light sources, together with skin cooling, target water content in the dermis, and their photothermal effect, produced as a result of the laser-tissue interaction, causes a rise in the dermal temperature. The consequences are collagen tightening, increased fibroblastic activity, and increased collagen production.
Near infrared and infrared lasers (1,064–1,540 nm) are particularly suitable for nonablative skin rejuvenation in dark-skinned patients as the longer wavelength is associated with less epidermal melanin interference. QS 1,064-nm Nd:YAG was one of the first lasers in the near infrared spectrum to be used for nonablative skin rejuvenation. Goldberg and Silapunt used pinpoint bleeding as the clinical end point for nonablative skin rejuvenation in lighter-skinned patients (type I to III) and found clinical and histological data to support the use of QS 1,064-nm Nd:YAG for the treatment of rhytids.9 In my experience, QS 1,064-nm Nd:YAG laser can be effective in skin rejuvenation among dark-skinned patients. Mild erythema rather than pinpoint bleeding should be used as the clinical end point (QS 1,064-nm Nd:YAG laser, 6-mm spot size, 1.6 J/cm2). A 1,064-nm Nd:YAG laser in the minisecond domain together with long-pulsed 532-nm potassium titanyl phosphate (KTP) laser has been used successfully for nonablative skin rejuvenation in Asians. Lee treated 150 patients (skin type I to V) with the long-pulsed KTP 532-nm (Aura; Laserscope, San Jose, CA) and long-pulsed Nd:YAG 1,064-nm (Lyra; Laserscope) lasers, both separately and combined.10 The fluences that were used varied between 7 and 15 J/cm2 at 7- to 20-millisecond pulse duration with a 2-mm handpiece, and 6 to 15 J/cm2 and 30- to 50-millisecond pulse duration with a 4-mm handpiece for KTP. The Nd:YAG fluences were set at 24 to 30 J/cm2 for a 10-mm handpiece and 30 J/cm2 for a SmartScan Plus scanner (Laserscope, San Jose, CA). These energies were delivered at 30- to 65-millisecond pulse durations. All of the patients were treated monthly three to six times and observed for up to 18 months after the last treatment. All 150 patients were found to have a mild to moderate degree of improvement in wrinkling, a moderate degree of improvement in skin toning and texture, and significant degree of improvement in redness and pigmentation. The KTP and Nd:YAG laser combination was superior to either laser used alone.10 In my experience, this combination is most effective, and using the large spot–size (10-mm) Nd:YAG laser, nonablative skin rejuvenation can be successfully performed in darker-skinned patients (10-mm spot size, 532-nm Nd:YAG 20 milliseconds, 7 J/cm2 for one pass, then 2-mm spot size, 12 J/cm2 to individual lentigines and telangiectasia and 1,064-nm Nd:YAG 45 milliseconds, 40 J/cm2 for two passes) (Gemini, Laserscope, San Jose, CA, USA).
Among all of the long wavelength lasers that are used for nonablative skin rejuvenation, 1,320-nm Nd:YAG has been extensively investigated. Trelles et al. studied the use of a 1,320-nm Nd:YAG laser among Spanish patients and found histological improvement and fair to significant clinical improvement 4 to 6 months after twice-weekly treatment for 4 weeks in total (1,320-nm Nd-YAG, 30–35 J/cm2, 30-millisecond dynamic cooling, 40-millisecond delay, 5-mm spot size, CoolTouch, Laser Aesthetics, Auburn, CA).11 Another study was performed to look at the use of 1,320-nm Nd:YAG laser for the treatment of acne scarring and wrinkle improvement in Chinese women. Of the 27 patients, seven were treated for acne scarring and the others for wrinkle reduction. Besides treatment of the face, all patients also received treatment in the postauricular areas so that a postoperative skin biopsy could be obtained. A spot size of 10 mm was used, and three passes were performed (two precooling and one postcooling). The overall degree of patient satisfaction was 4.9 (range 0–9.8) for wrinkle reduction and 4 (range




Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree