Abdominal Breast Reconstruction Using a SIEA Flap Approach
Adrian S. H. Ooi
Deana Shenaq
Julie E. Park
David H. Song
DEFINITION
Abdominal-based flaps for breast reconstruction can be divided into pedicled and free flaps based on their arterial supply.
Pedicled
Transverse rectus abdominis myocutaneous (TRAM) flap
Free
TRAM flap
Muscle-sparing TRAM (MS-TRAM) flap
Deep inferior epigastric perforator (DIEP) flap
Superficial inferior epigastric artery (SIEA) flap
The free TRAM, MS-TRAM, and the DIEP flaps are based on a deep inferior epigastric vascular pedicle arising directly from the external iliac vessels.
In the free TRAM flap, the entire width of rectus muscle is taken to capture all the perforators within that segment.
In the MS-TRAM flap, a cuff of rectus muscle is harvested to capture multiple perforators from the deep inferior epigastric pedicle.
In the DIEP flap, only the perforating vessels to the subcutaneous fat and skin are harvested and the rectus muscle is not sacrificed.
The SIEA flap is based on the subcutaneous superficial inferior epigastric vascular pedicle arising from the femoral vessels in the femoral triangle. Harvest of the flap does not involve any rectus muscle or fascia.
ANATOMY
The SIEA flap is a Mathes and Nahai fasciocutaneous type A flap, harvested from the lower abdomen.
The skin island for the SIEA flap extends laterally to the anterior superior iliac spine (ASIS), medially to the midline or just past it, and from the level of the umbilicus superiorly to the pubic tubercle inferiorly.
Vascular anatomy
Arterial
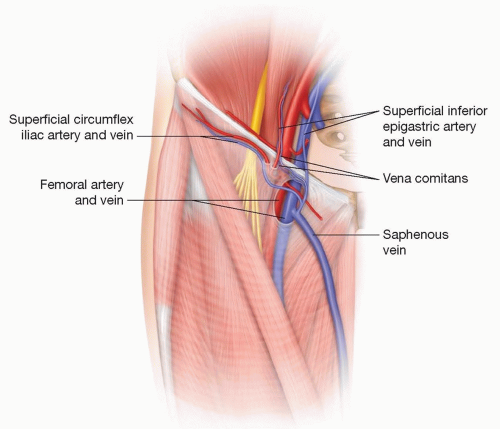
The SIEA is a branch of the femoral artery and arises from the femoral artery 2 to 3 cm below the inguinal ligament (FIG 1).
The average size of the SIEA is 1.2 to 1.6 mm and average length 4 to 6 cm.3
It is present in both groins in 58% of patients.4
In about 75% of cases, it arises from a common origin with the superior circumflex iliac artery (SCIA).5
The course of the artery is variable in relation to the superficial inferior epigastric vein (SIEV), usually arising up to 3 cm lateral to the SIEV and deep to the Scarpa fascia.
After piercing the cribriform fascia, the SIEA courses inferolaterally for a short distance immediately above the deep fascia.
It runs in a superolateral direction before crossing the inguinal ligament at roughly the midpoint between the pubic tubercle and the ASIS.
The SIEA then pierces the Scarpa fascia to run in the superficial fatty later of the abdomen before arborizing with the periumbilical perforators of the deep inferior epigastric artery.
Venous drainage
The venous drainage of the flap is through up to two venae comitantes of the epigastric artery and/or the SIEV (see FIG 1).
Diameter: 1.3 to 4 mm1
The surface marking of the SIEV is one-third of the way between the pubic symphysis and the ASIS.
The SIEV directly drains the subcutaneous plexus and is usually located superficial and medial to the SIEA in the superficial fatty layer of the abdomen.
The venae comitantes of the SIEA typically drain into SIEV.6
Occasionally, the superficial circumflex iliac vein (SCIV) and SIEV join into a common branch before draining into the femoral vein and if taken together can be used to enhance venous drainage of the flap (FIG 2).
Flap vascular territory
The literature consists of varying reports using different measurement parameters stating flap perfusion can range from the hemiabdomen to 100% of the entire abdominal flap.1,2,6
We have found harvesting of the tissue across the midline to be unreliable, and would not advocate going past the hemiabdomen without testing perfusion either clinically with clamping off all other vascular input on the contralateral side or utilizing intraoperative fluorescence imaging.
The flap receives sensory innervation via the segmental intercostal nerves T10-T12.
PATHOGENESIS
Breast defects requiring SIEA flap reconstruction can be partial or total mastectomy defects and can arise from a variety of pathologies including:
Postcancer resection
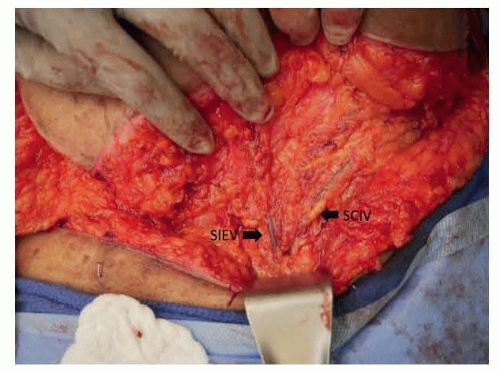
FIG 2 • The left superficial inferior epigastric (SIEV) and superficial circumflex iliac veins (SCIV) draining into a common branch.
Prophylactic resection
Failed implants
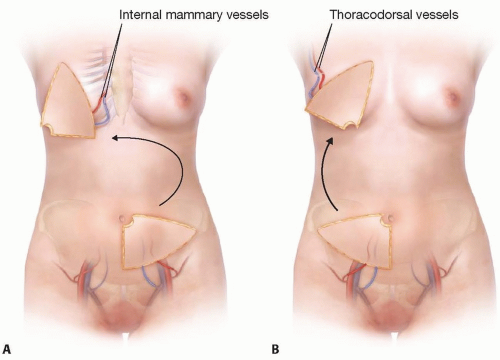
A single large mastectomy defect may require a complete abdominal flap for coverage. An SIEA flap can be used together with the contralateral SIEA, DIEP, or MS-TRAM flap.
The SIEA flap has been used for coverage of other defects including:
Head and neck
Upper extremity and hand
Lower extremity
NATURAL HISTORY
Holmström reported the first use of a free abdominoplasty flap based on the deep inferior epigastric vessels in 1979.7
Hartrampf pioneered the use of the pedicled TRAM flap for breast reconstruction in 1982.8
While sacrificing rectus muscle, the free TRAM gained increasing popularity for breast reconstruction due to the use of the dominant blood supply to the rectus muscle, the deep inferior epigastric pedicle, to perfuse the abdominal tissue. It also allowed for more freedom in insetting and shaping the breast.9
To minimize donor-site morbidity from harvest of the rectus muscle, the free MS-TRAM and DIEP flaps were developed following improvements in microsurgical knowledge and technique. Varying amounts of rectus muscle are left behind after harvest to maintain abdominal wall integrity and strength.
Further evolution of the abdominal tissue flaps led to the development of the SIEA flap. The flap, first used by Antia and Buch for facial reconstruction in 1971 and further elucidated by Taylor and Daniel in their cadaveric studies of 1975, is based on a subcutaneous pedicle and completely spares the rectus fascia and muscle. Grotting first reported on its use in breast reconstruction in 1991, and owing to its obvious donor-site benefits has rapidly gained popularity ever since.10,11,12
PATIENT HISTORY AND PHYSICAL FINDINGS
A focused history and examination relevant to any form of free flap reconstruction should be performed. In particular, the following should be elucidated and corrected if possible:
History of tobacco use
Obesity
Previous irradiation
Prothrombotic conditions
Anticoagulant use
Similar criteria are applied to the SIEA flap as when determining the suitability of a patient for a free DIEP, MS-TRAM, or TRAM.
Sufficient redundant lower abdominal skin and fat
Approximates final desired breast volume
Allows for primary donor-site closure analogous to an abdominoplasty
Abdominal scars
Transverse lower abdominal scars such as in a Pfannenstiel incision may preclude the use of the SIEA or even deep inferior epigastric pedicles.
Midline laparotomy scars limit the abdominal tissue use to a single hemiabdomen as the perfusion across the midline is no longer reliable.
IMAGING
Though not essential, several preoperative investigative techniques can be used to elucidate the vascular anatomy of the abdominal flap.
Doppler ultrasound
Can be used pre- and intraoperatively to locate perforators and pedicle position.
Used postoperatively for flap monitoring
CT-angiogram and MR-angiogram
Used preoperatively to elucidate location of abdominal perforators and the route of the source vessels
Can be used to select cases where the SIEA is suitable for use
Fluorescence imaging
Intraoperative administration of ICG via a peripheral vein after the hemiabdominal flap has been isolated on its pedicle and imaging with an infrared camera can help to assess the flap vascular territory.
DIFFERENTIAL DIAGNOSIS
Reconstructive options for breast defects include but are not limited to:
Implant-based reconstruction +/− acellular dermal matrix
Immediate implant
Primary expander with implant exchange
Expander-implant
Pedicled flaps
Latissimus dorsi (LD)
TRAM
Free flaps
LD
TRAM
MS-TRAM
DIEP
SIEA
Superior gluteal artery perforator (SGAP) flap
Inferior gluteal artery perforator (IGAP) flap
Gracilis muscle-based flaps
Anterolateral thigh
Pudendal artery perforator (PAP) flap
Lateral thigh perforator (LTP) flap
SURGICAL MANAGEMENT
Options of breast reconstruction should be tailored to each individual patient based on her disease process, adjuvant treatment, body habitus, and personal preference.
Although implant-based breast reconstruction provides an expeditious reconstructive option, it is associated with implant-related complications as well as aesthetic outcomes which can be below expectations, especially in the setting of postoperative radiotherapy.
We consider implant-based reconstruction in these scenarios:
The patient refuses autologous tissue use or has no autologous options.
Bilateral mastectomies
No postreconstructive radiation planned
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree