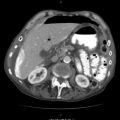
Fig. 8.1
Ways to reestablish patency or protect the airway
Treatment of A with no equipment, chin lift and jaw thrust, can be practiced “in the street,” requires 10 s works, and resolves almost all cases of airway obstruction due to the tongue simply dropping back. Remember to protect the spine.
Airway intubation with temporary measures is easier and faster than with permanent ones. It can be applied “in the street,” but requires equipment. If you have to bypass an obstructed airway surgically with no means, remember you can bail out with a needle cricothyrotomy (Figs. 8.2 and 8.3). This takes 60 s and buys 30 min for your patient. If you are enthusiastic, confident, and courageous and have common sense, have handy the pocket airway “Life-Stat®” – a metallic trocar with a large needle to penetrate the cricothyroid membrane, a connecting cannula, and a universal adapter matching the tubing diameter of any ventilator. The device is packed in one tube within the other, and you can carry it with your key holder. The only issue here is to convince airport authorities that you want this sharp instrument with you on board for a novel purpose.
Fig. 8.2
Technique for needle cricothyrotomy (lateral view)
Fig. 8.3
Technique for needle cricothyrotomy (craniocaudal view)
Temporary airway tubing can become dislodged at any moment. Replacement with a permanent one is mandatory a.s.a.p. This requires an organized environment, equipment, more skill, and a lot of time. A knife, a really helpful tracheal hook, a curved clamp, a tube, and your steady hand are all you need to perform an emergency cricothyrotomy (Fig. 8.4).
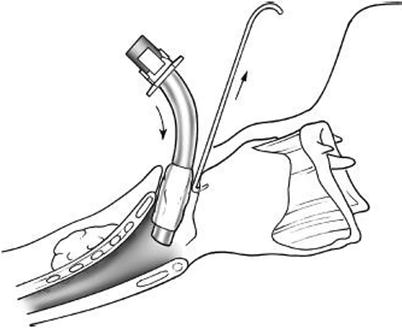
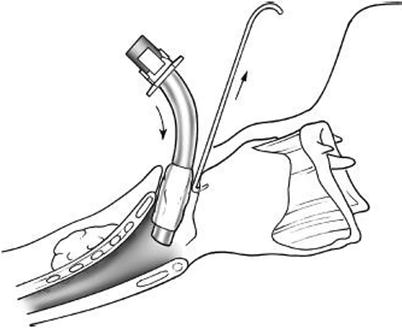
Fig. 8.4
Surgical cricothyrotomy (notice the hook)
So by now you have devoted something like 10 s, let’s say, to evaluating your patient’s airway, and if it is really indicated, another 3 min (a lot of time) to securing it, and now you are ready to proceed to B.
8.2 Breathing
8.2.1 Evaluation
Fifteen more seconds is needed to identify a life-threatening injury from B and localize it R or L. Clinical presentation in a conscious patient is so impressive and typical that it strikes you from a distance. The patient is in extreme agony, combative, with swallowing, high-frequency breaths, speaking with short, sharp phrase, “Doc, help; I am dying,” with every breath repeating exactly the same sentence, cutting the last word, because his breath volume is not enough to allow him to complete it. In such a “loud” case, are you allowed to bypass A and decompress the tPTX first? By all means. It’s “ABC” vs common sense. A 15-s delay in A evaluation, to reestablish breathing and circulation, is a bargain. If you are not “lucky” enough to see such a patient, a report of penetrating injury to the thoracic surface should alert you before you even see him. Observation of the respiratory movement of the two hemithoraxes and bilateral auscultation at the second intercostal space, midclavicular line, and sixth intercostal mid-axillary location is diagnostic. At the initial evaluation, a single breath or even less, one inspiration or expiration is enough to decide. If clear, proceed to C. If it sounds like there is a problem, do not waste a second, just treat. If you are inconclusive, given your clinician’s common sense, it seems that your patient has enough respiratory reserve to undergo an on-table X-ray. Any second delay from radiology should be invested in the next step, C.
8.2.2 Treatment
Two life-threatening injuries in B need immediate action. In most cases, this action will solve the problem, and only 15 % will need an operation.
Tension PTX: Decompression with a needle is done at the second intercostal space at midclavicular line. The task should be completed within 15 s, 14 of which are needed to find a large-caliber long venous catheter (a.k.a. needle) if you are not prepared. This will give time extension to a dying patient. During that time you now reevaluate A. If this is already done, you can put in a chest tube (Fig. 8.5), which takes a couple minutes if you are reasonably fast. If you anticipate more time for this task (skill confidence, find the tube, collection system not ready), it is wise to complete a rapid evaluation of C (30 s and three answers away), to have an idea what waits you there and start preparing, and then come back and complete the job with B, adjusting your pace.
Fig. 8.5
Insert chest tube without its trocar on the upper boarder of the lower rib. After insertion rotate tube by 360o at its longitudinal axis to avoid its entrapment in lung fissure
Massive hemothorax (HTX): more than 1,500 cc is drained as you put in a chest tube, or 200 mL/h over 3–4 h. Usually HTX is not massive, because vessels within the chest cavity are low-pressure/easily clotting, and the issue is simply to drain the blood completely. The thoracic cavity/mediastinum contains high-pressure vessels, which, when bleeding, can result in death even before arrival at the hospital. This could be one of the 15 % of cases that will require immediate operative management, where you actually treat a problem from C located in the B area. While you transport the patient to the OR, evaluate C and prepare for additional surprises.
Two more injuries from B require immediate action, although these are less demanding regarding time.
Flail Chest
Infrequent in penetrating injury. Patient will have lung contusion that will worsen over time; with aggressive fluid resuscitation, he will hypoventilate to diminish the pain in the injured area and may have HTX or PTX. Manage them with oxygen, analgesia, and physiotherapy. If the FiO2/PaO2 ratio drops below 200, prolonged intubation is required until contusion resolves.
Simple HTX or PTX
The issue here is to be sure that HTX is simple and not massive, and the easy way is an X-ray, most effective being a chest tube, both at least 2 min away. In simple open PTX a >3-cm defect at the wall affects respiration significantly and will press for immediate action (chest tube, dressing). In this case an Asherman chest seal (http://www.ashermanchestseal.com) is a very effective alternative for the physicians that have organized an emergency handbag for the field. In both cases, consider the vital signs, the time requirement for an X-ray/chest tube, and the stability of the patient, and you may choose to prioritize the chest tube over an X-ray or even a rapid initial assessment to rule out lethal injuries from C.
The bare necessities you need for substantial management of B injuries are large-caliber needle, chest tube, draining system with a Heimlich valve (sophisticated or simple), and the luxury of X-ray and stethoscope. You will find them in every medical facility. In the extreme scenario where your services are needed in an isolated environment, develop them by being a bit innovative. A real life example of chest tube placement during an airplane trip: whisky as antiseptic, a straightened wire from a dress hanger as a stylus, and a straw as a chest tube.
8.3 Circulation
Common sense bypasses all principles/traditions. If you are facing the red-hot juice pouring out of the body, compress to stop it, before B and before A. Devote 1 s and buy a lot of time. Applies to all compressible areas, from carotid to … digital artery. For uncompressible cavities (chest, abdomen) the patient needs an operation to contain the bleeding, so you follow time effectively the ABC rules.
C is a little more complex than A and B. It has three components: the pump, the tubing, and the circulating fluid. This vignette raises more questions that need to be answered, but again rapidly fatal injuries are very rare.
Start vice versa, treating before evaluating. Two 18-gauge IV catheters give you access to the intravascular space, a bare necessity. Postponing this task narrows the chances of success because of volume depletion. You can accomplish this within 60 s, although much longer times have been reported. For difficulties in venipuncture, familiarize yourself with the intraosseous catheterization technique and its limitations and utilize power intraosseous “EZ-IO®,” which promises 30-s access to the intraosseous/intravascular space in adults, has been tested, and works.
8.3.1 Evaluation
Check first what kills most rapidly:
- 1.
Get Clinical Tree app for offline access
Pump
- (a)
Heart penetration: Suspect it if there is penetrating injury to the left chest. Blood pressure rapidly drops despite resuscitative efforts. It is an ideal indication for ER thoracotomy, especially if the patient loses the pulse while retaining electrical heart function. You will need only six instruments, knowledge of the simple technique (see relevant Chap. 11), boldness, and common sense. Within 4 min you have the descending aorta clamped, so you force the few circulating erythrocytes to perfuse the brain, repair the cardiac hole with traumatic and not elective techniques (see relevant Chap 11 again), and give IV blood at a rhythm of 1 L/min if you have a rapid infuser. This injury is unmanageable outside of a well-organized hospital.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree



- (a)