65. Aesthetics of Gender Affirmation Surgery
The World Professional Association for Transgender Health (WPATH) promotes a multidisciplinary approach for the care of transgender patients.
According to the WPATH, transgender patients should be under the care of primary care physicians, mental health services, and endocrinologist and surgical specialists.
Although hormone and nonsurgical interventions may help in the transition of transgender patients, surgical interventions play a significant role in achieving psychological well-being and self-fulfillment.
Surgeons who have received specialized training in transgender surgery may address the unique aesthetic and functional concerns of transgender patients.
Facial Feminization
Facial feminization surgery (FFS) is primarily based on the modification of bone structures to soften masculine facial features.
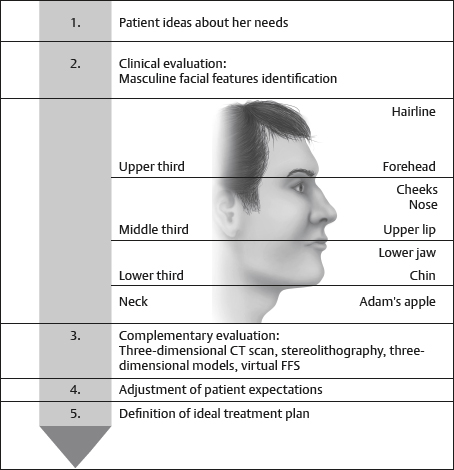
A comprehensive history and physical examination are necessary to appropriately diagnose a patient and to adapt specific surgical options rather than proceeding with a standardized approach.
Goal is to use hidden approaches and protocolized surgical techniques to achieve a natural and aesthetic result, alleviating gender dysphoria and facilitating transition.
Aesthetic Evaluation
Craniofacial Skeleton
Upper third: Hairline and frontonasal-orbital complex
Frontonasal-orbital complex: Greatest determinant of facial gender
Includes forehead, supraorbital ridge, orbit, frontal bossing, frontomalar region, temporal ridges, and frontonasal transition
Determines the position of the eyebrows and periorbital soft tissues, including the eyelids
Typically, more pronounced with greater bone volume in males versus females
Middle third: Nose, cheeks, and upper lip
The male nose is generally larger than the female nose because of increased volume of bone and cartilage, most notable at nasal dorsum and tip.
Males have greater malar bone volume, resulting in well-defined cheeks. Females have a greater concentration of fat in middle third of the face, giving them prominent round cheeks, which are compatible with femininity.
In males, the distance between the upper lip and nose is longer than in females.
Lower third: Jaw and chin
In males
The mandibular angle area is usually squared with well-defined corners.
The mandibular body has greater bone volume, which produces a wider lower facial third and gives greater vertical height.
The chin tends to be squared, providing a more pronounced and defined transition between the chin and mandibular body.
Neck: Thyroid Cartilage (Adam’s Apple)
The thyroid cartilage is among the most prominent hallmarks of male gender.
In males, the trachea has a greater volume and diameter.
Caution:
Although the most prominent portion of the thyroid cartilage can be modified during FFS, the tracheal structure itself should never be surgically approached for facial feminization, because it carries unacceptable and unnecessary risk for vocal cord damage and respiratory compromise.
Secondary Traits
Include the hair and hairline shape, facial hair, skin texture, and the distribution and volume of facial fat
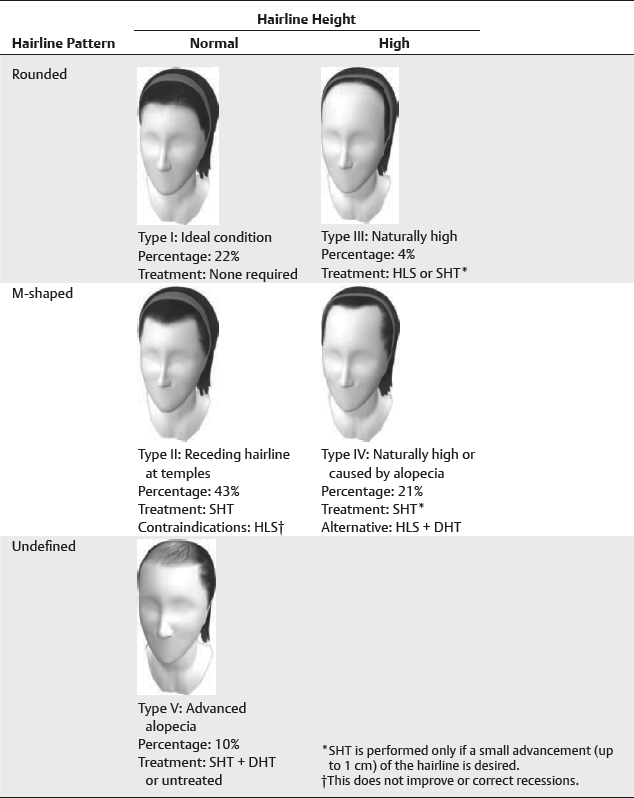
Males have M-shaped hairline with recession at temples, which may be affected by androgenic alopecia 1 ; females usually have rounded hairline that extends slightly higher in the center than in men 2 (Fig. 65-2).
Virtually all males have facial hair, which conditions skin to become thicker and rougher.
Largely influenced by hormones, females have a greater concentration and volume of facial fat within the middle third of the face (cheek). 3
Secondary features respond well to hormone therapy and should be addressed before FFS. 4
Surgical Consideration for Facial Feminization Surgery
Facial CT with three-dimensional reconstructions should be obtained to assess anatomic features that can be addressed.
In cases of financial limitations, a Panorex and lateral cephalogram will often provide adequate information.
Preoperative, intraoperative, and postoperative photographs (7 days, 6 months, and 1 year) should be maintained to provide an objective view of changes.
Upper Third
Forehead reconstruction
Forehead reconstruction completely modifies the frontonasal-orbital region and softens and feminizes the patient’s expression.
Goal: To reposition and remodel the forehead complex to soften frontal bossing, supraorbital rims, frontomalar buttresses, and temporal ridges
Approach: Osteotomy and repositioning of the anterior wall of the frontal sinus 5 or burring, depending on the anterior table thickness, to soften this region
Can be combined with hair transplantation to achieve upper-third feminization in one stage 6
Hairline versus modified coronal incision should be determined by hairline position and patient desires.
If hairline is low, then coronal incision is used.
Senior Author Tip:
If the anterior table of the frontal sinus is ≤3 mm, then a frontal bone setback will often be required to achieve a good result.
Hairline
Hairline lowering surgery is recommended only in patients with a high hairline, and non-hair-bearing scalp is excised during the lowering procedure.
Senior Author Tip:
Suturing of the posterior scalp flap to a cortical tunnel in the frontal bone or to titanium mesh or plates helps to maintain a lasting effect of hairline lowering.
Hair transplantation
Should be performed after androgenic alopecia stabilizes
Recommended for patients with an M-shaped hairline and with sufficient hair density without active androgenic alopecia
Goal: To address the recessed corners of the hairline
Central section of the hairline can also be addressed if hair density here is an issue.
May be performed during forehead reconstruction or in a delayed fashion 6
Follicular unit strip (FUS): Follicles are obtained from a strip of scalp removed in a small surgical procedure.
Follicular unit extraction (FUE): Individual follicles are obtained, without the need for a surgical procedure.
Middle Third
Cheeks
Fixed porous polyethylene implants for augmentation, zygoma not commonly reduced in FFS
Placed using an intraoral approach
Results stable over time
Autologous fat
Deposited in supraperiosteal plane
Natural results but dependent on surgeon’s experience
May require multiple sessions given graft resorption
Nose
Standard rhinoplasty techniques are used to make nose smaller and compatible with surrounding facial features.
Reduction rhinoplasty is commonly performed immediately after forehead reduction when done as a combined procedure.
The final result is largely dependent on skin quality.
Reinforcement of nasal tip and dorsum with cartilage grafts to prevent collapse is recommended.
Upper liplift
Goal: To reduce the vertical dimension between the upper lip and nose
Approach: Modified bullhorn technique to remove strip of skin and subcutaneous tissue without violating orbicularis oris 7
Performing the procedure in conjunction with an open rhinoplasty procedure is not recommended.
Lower Third
Lower jaw and chin
Goals: To modify width and height of the jaw, soften the jawline (including the transition between the mandibular angle and symphysis), and modify the size, shape, and position of the chin
Intraoral approach is strongly advised.
Approaches
Panorex or CT scan to evaluate both the course of inferior alveolar nerve and the third molar tooth roots and their relation to the mandibular angles
Burring: Used to reduce bone volume in parasymphysis, symphysis, mandibular body and angles
Standard osteotomies: Used to address chin position
Osteotomies with piezosurgery: Technique of choice for basal mandibular and chin bone resectioning and for redesigning mandibular angles
Neck
Thyroid cartilage
Recommended in the region of the cervicomental fold to conceal scar and prevent adhesions between thyroid cartilage and overlying soft tissues
Incision should not exceed 2 cm.
Approach: Burring, rongeuring, or sharp resection with scalpel
Must avoid sculpting near vocal cords
Senior Author Tip:
Marking should be performed with the patient facing the surgeon; the surgeon should place the incision as cephalad as possible for maximal concealment.
Top Surgery
For transgender females, this refers to breast augmentation with implants and/or autologous tissue.
Top surgery in transgender females may require a mastopexy because of the commonly low position of biologic male nipple on chest wall.
For transgender males, this refers to breast reduction/mastectomy.
A double-incision mastectomy (free-nipple grafts) is the most common top surgery procedure for transgender males, with the most predictable results.
Top surgery remains one of the most commonly performed surgeries in gender reassignment and one letter from a qualified mental health therapist recommending the patient for surgery should be obtained before performing the procedure in both transgender males and transgender females.
Top surgery may significantly facilitate a patient’s ability to live in a gender role congruent with their gender identity and is commonly performed before bottom surgery (vaginoplasty or metoidioplasty/phalloplasty).
For some transgender people, top surgery will be the only surgical step during transition.
Indications
Per WPATH 8 :
A persistent, well-documented history of gender dysphoria
The ability to make a fully informed decision and to give consent
Age of majority in a given country
A significant medical or mental health concern in a prospective patient for top surgery must be well controlled.
One letter from the patient’s mental health therapist recommending the patient undergo the procedure is required.
Additional Recommendations
Transgender females should undergo feminizing hormone therapy for a minimum of 1 year before breast augmentation surgery to maximize breast growth and obtain superior aesthetic result.
Usually, only a half to a full cup size is obtained in breast growth in transgender females on hormone therapy, and size will decrease if hormones are stopped.
Male-to -Female Top Surgery Aesthetic Considerations
Hormone therapy promotes mammogenesis, which follows a pattern similar to female pubertal mammogenesis, resulting in a softly pointed breast, as seen in young girls, or the small conical form found in young adolescents (Tanner stage 2 or 3). 9
Hormone effect is not dose dependent.
Males tend to have a wider chest, stronger pectoral fascia, more developed pectoralis muscles, and smaller nipple-areola complexes (NACs).
Surgical Considerations
Even with large volume and a wide implant, preventing wide cleavage between breasts is often not possible.
The NAC should always overlie the implant centrally.
Overly medial implant position can result in divergent nipple position and an unacceptable aesthetic result. 10
Implant selection
Silicone gel-filled implants versus saline-filled implants
Use of textured implants may reduce the potential for capsular contracture.
Anatomic cohesive gel-filled implants provide additional lower pole projection.
Incisions
Axillary
Inframammary: Should be placed lower than preoperative inframammary fold because the inferior areolar margin and inframammary fold will expand after augmentation
Periareolar: Less popular because of smaller areola in transgender females
Pocket
Subglandar: Easier to perform; less pain with good aesthetic results in patients with more subcutaneous and glandular tissue (Tanner stage 4 or 5)
Subpectoral: More soft tissue coverage of implant, which is necessary in thin patients; lower risk for capsular contracture
Fat Grafting
Good alternative to implants in patients with some breast volume from hormone treatment
Can provide a small to moderate augmentation of the breast
Patients need to be informed that variable amounts of the injected fat will be resorbed.
May require multiple grafting sessions to achieve desired volume
May also be used as an adjunct to implants
Injected into subcutaneous plane
Decreased implant visibility
Helps to narrow wide cleavage between the breasts
Female-to-Male Top Surgery
Aesthetic Considerations
Hormone therapy has minimal influence on breast size in transgender males.
Subcutaneous mastectomy (SCM) to create a male chest is the first surgery in transgender males. 13
SCM helps patient live in gender role that is congruent with their gender identity, which is required before bottom surgery.
Relative to males, the female chest has excess skin and glandular tissue, as well as abundant subcutaneous fat.
In females the inframammary fold is well defined; in males the inferior margin of the pectoralis marks the inferior margin of the chest.
During SCM, the inframammary fold is often obliterated to achieve aesthetic contouring.
Goals of SCM
Removal of breast tissue and excess skin
Reduction and proper positioning of the NAC
Obliteration of the inframammary fold
Minimization of chest wall scars to achieve aesthetically pleasing male chest
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree