61. Medial Thigh Lift
Anatomy
The medial thigh has a relatively thin outer layer of epidermis and dermis.
Beneath the dermis are two layers of fat separated by a relatively weak superficial fascial system.
Deep to the subcutaneous fat lies the strong, thick Colles fascia. 1 – 4
Attaches to the ischiopubic rami of the bony pelvis, to Scarpa fascia of the abdominal wall, and to the posterior border of the urogenital diaphragm
Has an especially strong area at the junction of the perineum and the medial thigh
Provides the anatomic shelf that defines the perineal thigh crease
Best found intraoperatively by dissecting at the origin of the adductor muscles on the ischiopubic ramus and retracting the skin and superficial fat of the vulva medially
Lies just at the deepest and most lateral aspect of the vulvar soft tissue 5
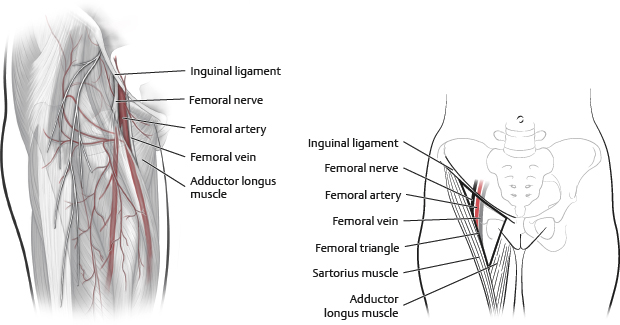
The femoral triangle lies lateral to the Colle fascia dissection (Fig. 61-1).
Midinguinal point between the pubic symphysis and anterior superior iliac spine
Borders
Superior: Inguinal ligament
Medial: Adductor longus
Lateral: Sartorius
Note:
Surgeons must be aware of the femoral triangle and avoid entering it to prevent major vascular or nerve injury and disruption of the lymphatic channels.
Indications and Contraindications
Indications
The indication for a medial thigh lift is the presence of skin laxity. Without skin laxity, thigh contouring may be achieved with liposuction alone.
Accurately classifying the deformity is critical for guiding treatment (see Tables 61-1 through 61-3).
Contraindications
Contraindications for performing a medial thigh lift are similar to those for any elective or aesthetic procedure and include the following:
The presence of modifiable risk factors, including residual obesity
Unresolved depression
Unrealistic expectations
Unwillingness to accept a lengthy scar or likelihood of common complications
Massive-weight-loss (MWL) patients with unstable chronic illnesses, cardiovascular disease, postphlebitic syndrome, or lymphedema
Preoperative Evaluation: History and Physical Examination
A complete history is obtained, with special attention to the following:
Smoking status
Nutrition status, with adequate protein and vitamin supplementation in bariatric patients
Weight history, especially weight stability
Surgical history, i.e., previous body contouring procedures
Psychiatric evaluation
Plans for other body contouring procedures and priority problem areas for the patient
A complete physical examination is performed, with special attention to the following:
Presence, location, and degree of skin ptosis–drape, bulges, tension, the pattern of sagging (i.e., proximal versus distal)
Skin tone and the relationship of skin to the underlying adipose
Context of the remaining thigh and lower body deformity
Presence or absence of extra subcutaneous fat in the medial and lateral thighs, lower body, which may be addressed with liposuction during surgery
Standardized photographs should be taken (see Chapter 3).
Classification Systems
Pittsburgh Rating Scale
6 (Table 61-3)
Tip:
Careful evaluation of each patient’s deformity is needed to determine the best treatment.
Senior Author Tip:
Careful evaluation of the lower leg preoperatively is essential. Many patients after weight loss will present with lipedema, which should be differentiated from preexisting lymphedema. The feet and ankles should be photographed preoperatively so that patient concerns of postoperative swelling can be assessed in comparison with the baseline examination.
The thigh can be addressed in thirds, regardless of whether patients have had massive weight loss. Skin laxity in the upper third can be treated by a medial thighplasty (crescent thighplasty) with the scar completely hidden in the groin crease. Laxity to the middle third can be treated with a short-scar vertical thighplasty. Laxity down to the knee and encompassing the entire thigh can be treated with a full-length vertical thighplasty. Global thigh adiposity is best treated with staged procedures: debulking liposuction first, followed by an excisional procedure. Patients with outer thigh skin laxity may be best treated with a circumferential lower body lift or Lockwood type 1 body lift first, which will allow some skin relaxation to occur postoperatively. Tissues will relax in a medioinferior direction; thus a staged medial thigh lift can help to correct any of the residual laxity after the initial body lift. If a patient had a prior abdominoplasty or panniculectomy, medial thighplasty can be combined with a lower body lift in a Lockwood type 2 procedure.
Informed Consent
The informed consent should include the likely possibility of wound complications and the possibility for extension of the incision/scar.
Senior Author Tip:
Thighplasty can have most of the complications seen in body contouring. Because the rate of minor wound-healing complications is very high with this procedure, they should be discussed in detail with patients before surgery to prevent postoperative dissatisfaction. Complications include seroma, hematoma, delayed wound healing, scar migration, prolonged pain, swelling or change in the shape of the genital region, tissue relaxation, leg swelling (which may be permanent and require chronic care [lymphedema]), unsatisfactory thigh contour and shape, incomplete correction of loose skin at the knee, and risk of deep vein thrombosis (DVT) or pulmonary embolism.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree