55. Breast Reduction
Pathophysiology
Breast hypertrophy is thought to be an abnormal end-organ response to circulating estrogens. 1 , 2
Normal number of estrogen receptors and normal levels of circulating estrogens have been found in women with hypermastia; thus an increased sensitivity to the hormone is suspected. 3
Hypermastia typically begins within the hormonal milieu of puberty or pregnancy.
With the increasing obesity epidemic, breast hypertrophy is often from excess adipose tissue rather than glandular hyperplasia.
Studies suggest that fat accounts for 46%-61% of modern breast reduction specimens. 4 , 5
Indications for Surgery
Breast reduction has an extremely high patient satisfaction rate and has been shown to improve self-image. 6 , 7
Medical Indications
Neck pain
Back pain
Shoulder pain
Bra strap grooving
Persistent or recurrent intertriginous infections, rashes, maceration, and irritation
Chronic headaches
In extreme cases, degenerative arthritis of the cervical and thoracic spine
Evidence
Netscher et al 8
Symptomatic hypermastia is better defined by symptom complex than by volume of tissue removed.
Symptomatic hypermastia affects quality of life on par with other significant chronic medical conditions (e.g., kidney transplant, living with moderate angina pectoris).
Symptoms are more important than volume in determining health burden and surgical benefit.
Weight loss, special bras, and medical treatments are not successful.
Aesthetic Indications
Women with hypermastia frequently report aesthetic dissatisfaction with breast size and shape.
Complaints include pendulous appearance and wide nipple-aerola complex.
Excessive size may limit clothing selection and athletic participation.
Tip:
Determining the aesthetic or medical necessity of reduction mammaplasty is ambiguous and nonstandardized by health insurance carriers in the United States.
Preoperative Evaluation
Patient History
Age (>50 years of age with higher complication rate, according to Shermak et al 11 )
Medical history of comorbid disease(s), clotting disorders
Surgical history pertaining to breast
Social history of smoking or nicotine use
Familial history of breast disease, anesthesia problems, deep vein thrombosis (DVT)
Breast history of lactation, changes with pregnancy and weight fluctuations, tumors
Previous medical or therapeutic treatment for hypermastia
Physical Examination
Sternal notch-to-nipple distance: Allows detection of asymmetry in nipple position
Nipple-to-inframammary fold distance: Serves as a measurement of the redundancy of the lower pole skin envelope
Base width: Allows detection of asymmetrical breast footprint
Areolar diameter: Widening of the areola is very common in patients with hypermastia (normal areolar diameter is 38-45 mm).
Classification of ptosis severity (see Chapter 52)
Breast examination for mass or lymphadenopathy
Additional Considerations
Skin quality: Presence of striae indicates the inelastic quality of affected skin.
Parenchymal quality: Fatty, fibrous, or glandular parenchyma
Mammogram
When indicated
Photography
(see chapter 3)
Anteroposterior (AP), lateral, and oblique photographs should be obtained.
Photographs of shoulder grooving and rashes, when present.
Patient Expectations
Breast shape
Reduction mammaplasty will not result in a virginal breast.
Most techniques will naturally result in a pendulous, mature-looking breast, but with a size more proportionate to the body habitus of the patient.
Breast size
The desired postoperative breast size can vary widely between patients and should be dicussed at length at the initial consultation.
Inform patients that complications with breast reduction are more common in larger reductions (>700 g) and in patients with a higher BMI. 12
Tip:
Although surgeons and patients frequently discuss bra-cup size, surgeons can better determine patients’ wishes by asking them to find representative photographs of the desired postoperative size in magazines or professional portfolios.
Informed Consent
Recommend items to be included in the informed consent:
A general description of the procedure and location of incisions
A sufficient description of potential risks
Bleeding and hematoma
Infection
Delayed healing and wound separation
Nipple necrosis, complete or partial
Change in nipple and skin sensation
Potential changes in breast-feeding
DVT and pulmonary embolism (significant risk with BMI >30 13 )
Asymmetry and poor cosmetic result
Poor lactation (70% of patients can lactate after surgery, but many require supplementary feeding.) 14 , 15 , 16
Poor scar quality
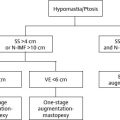
Surgical Options
Most techniques described in Chapter 53 were initially developed for breast reduction. Most patients with hypermastia also have breast ptosis. For detailed information on short-scar techniques, please see Chapter 53.
Liposuction has been described as an additional or sole treatment for reduction mammaplasty.
Reduction mammaplasty by excision can be thought to include the following four elements:
Selecting a pedicle to provide vascularity and innervation to the nipple-areola complex (NAC)
Determining the quadrants of the breast from which to resect tissue
Excising excess skin after removal of breast parenchyma
Creating an overall aesthetic breast shape. 17
Suction Lipectomy
Liposuction is often used in combination with excisional techniques to limit scar burden but can be used alone to reduce breast size. 18
Patient Selection/Indications
Ideal candidates:
Have a normally positioned NAC
Good skin quality
Predominantly fatty breasts.
A useful technique in elderly patients with significant symptoms of hypermastia and insignificant cosmetic concerns 19
Advantages
Smaller scars
Preserves lactation and vascular supply to the NAC
Preserves existing sensation
Can be easily performed with local and intravenous sedation
Disadvantages
Most surgeons agree that breast ptosis cannot be adequately treated with suction lipectomy alone and may be worsened in patients with poor skin quality.
Postoperative edema and induration often take months to resolve.
The evacuated breast tissue cannot effectively be sent for pathological evaluation.
Technique
Lateral and medial inframammary fold (IMF) stab incisions are used.
Wetting solution is infiltrated.
3-5 mm cannulas are used to treat both superficially and deep.
Postoperative compressive bras are worn for 6 weeks.
Note:
Ultrasound-assisted liposuction has been used in the breast, but surgeons are advised to obtain exhaustive informed consents from their patients, discussing the unknown effects of ultrasonic energy on breast tissue.
Excisional Techniques
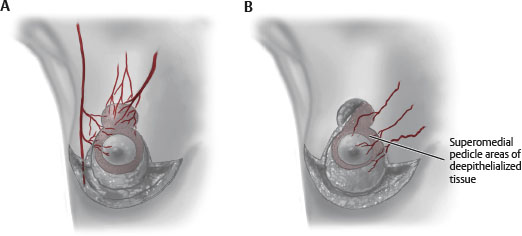
Pedicle Selection
Options include inferior pedicle, superior/superomedial pedicle, and central mound technique.
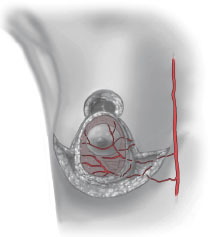
Inferior Pedicle
Has been the preferred method (in the United States) and is easily teachable 25
NAC maintained on an inferior dermal-parenchymal pedicle
Lateral, medial, and superior breast tissue can be removed.
Usually paired with an inverted-T skin excision
May use short-scar periareolar inferior pedicle (SPAIR) introduced by Hammond 26
Advantages
Large parenchymal resections can be done safely.
Reliable neurovascular supply
Lactation preserved in most patients 14 , 15
Low complication profile (11.4%) 27
Disadvantages
When nipple to fold is >18 cm, the pedicle becomes bulky, limiting extent of reduction.
Passive creation of breast shape from tailoring skin around parenchyma
Often creates a boxy breast
High rate of bottoming out
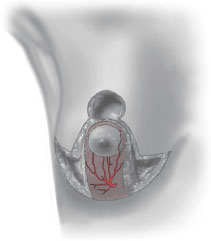
Superior/Superomedial Pedicle
Lassus 28 , 29 is credited with introduction of the superior pedicle technique.
Lejour 22 , 30 is credited with refinements and popularization of the technique.
Hall-Findlay 31 popularized the superomedial pedicle.
Nahabedian and Mofid 32 and Lista and Ahmad 33 made contributions.
Modifications include Strombeck horizontal bipedicle technique. 34
NAC is maintained on a superior or superomedial dermal-parenchymal pedicle.
Lateral, medial, and inferior breast tissue can be removed.
Advantages
Large parenchymal resections can be done safely, and involve resection of the ptotic tissue.
Pedicle is created from main blood supply of NAC. 35
Pedicle is superior, where fullness is commonly desired.
Allows creation of inferior pillar support to limit bottoming out
Ease of use with short-scar techniques
Nipple-areolar sensation reliably maintained
Disadvantages
Learning curve for technique
Creates dead space at dependent part of breast, where fluid may accumulate
Central Mound Technique
NAC is maintained on a central parenchymal pedicle (without dermis).
Breast tissue can be excised laterally, medially, superiorly, and inferiorly, leaving a central glandular component.
Advantages
Less reliable nipple-areolar neurovascular supply
Ideal to preserve lactation
Allows variable resection of parenchyma in multiple quadrants
Disadvantages
Underresection is common.
Safety issues with undermining pedicle as blood supply comes from chest wall.
Breast shape/support largely dependent on dermal support
Possible bottoming out.
Tip:
With all pedicle patterns, nipple viability should be checked before thinning the breast flaps. If the NAC is ischemic, the operation can be converted to a free nipple graft and the pedicle debrided to the appropriate level without compromising breast volume.
Skin Resection Patterns
Mastopexy procedures (or very small reductions) allow periareolar incisions and skin resection alone, but this is inappropriate for use in patients with true hypermastia.
Vertical Pattern
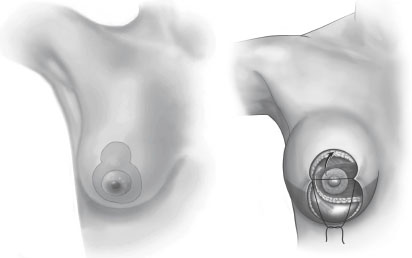
Allows excision of lax skin in horizontal dimension
With lateral (lazy-J) extension lax skin in the vertical dimension 36 , 37
Some authors advocate tailor-tacking to facilitate incision placement.
Once desired shape and skin contour are obtained, the “tailored” resection pattern is marked and excised.
Other techniques avoid a transverse scar by gathering the skin in the vertical closure, leaving a dog-ear in the inframammary fold (IMF). 31 This skin redundancy requires delayed excision in approximately 5% of patients.
More recent evidence, however, cautions against the use of gathering sutures 38
Significantly reduce the incision length in the operating room but do not change the areola-to-IMF distance or pucker revision rate.
Gathering negatively influences skin vascularity and wound healing.
Senior Author Tip:
If the remaining dog-ear appears exceptionally large in the IMF, do not hesitate to excise it with a small horizontal excision. A small horizontal incisional scar is usually preferable to a revision procedure, even if done in the office.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree