52. Breast Augmentation
Background
Breast augmentation is the second most common cosmetic surgery (after liposuction). 1
Silicone implants were introduced in 1964.
Saline implants were introduced in 1970s as an alternative to silicone.
The U.S. FDA placed a moratorium on silicone implants in 1992 for primary augmentation because of concerns about autoimmune and connective tissue disease.
In 1999 the NIH Institute of Medicine and the National Academy of Sciences reviewed 17 epidemiologic studies and were unable to detect any link between silicone and systemic, autoimmune, or prenatal disease.
Studies found silicone in local macrophages, lymph nodes, and breast tissue.
Studies did not demonstrate elevated systemic levels (normal liver, lung, and spleen). 2
Saline implants increased in popularity during the 1990s because of silicone scare.
Silicone implants have evolved through different generations (Table 52-1).
Restriction on use of silicone gel implants for primary breast augmentation was lifted in November 2006.
Before this change, silicone implants were approved only for breast reconstruction, silicone implant exchange, and replacement of saline implants with complications. 3 , 4
Cohesive gel implants are considered to offer significant advantages.
In Europe since 1995
In Canada since 2000
Advantages: More natural shape, less rippling, limited gel migration in event of rupture
Disadvantages: Larger incision, more expensive, stiffer
Indications and Contraindications
Indications
Increase breast size
Restore prelactation breast appearance
Correct breast asymmetry
Enhance breast shape and volume
Improve body image, symmetry, and balance
Improves fit of clothing
Provide the appearance of a breast lift and increased cleavage
Rejuvenation after postpartum deflation
Contraindications
Significant breast disease (e.g., severe fibrocystic disease, ductal hyperplasia, breast cancer)
Collagen vascular disease
Body dysmorphic disorder
Psychological instability
Social instability (e.g., divorce or separation, searching for a relationship)
Patient responding to pressure from friends, family, or partner
Patient <18 years of age
Silicone implants are not FDA approved for women <22 years of age (see Chapter 1).
The following situations require mindfulness 6 :
After obtaining the history, the surgeon does not like the patient.
Patient desires an outcome the surgeon cannot deliver.
Patient desires an outcome outside the surgeon’s aesthetic sense of normal.
Patient is critical of previous surgeons or praises the current surgeon excessively.
Patient lies, provides a false history or information.
Patient refuses to be examined or photographed.
Patient is a perfectionist and wants a guarantee of results.
Patient is paranoid, delusional, or depressed.
Patient fails to communicate or is unable to understand what informed consent entails. PREOPERATIVE EVALUATION
Preoperative Evaluation
History/Interview
Begins with open-ended questions
The patient talks and the surgeon listens.
Assessment:
Motivation for surgery
Psychological state of mind and stability
Level of understanding
Expectations
Self-esteem
Medical history
Full medical history
Personal or family history of breast disease or cancer
Pregnancy history and plans for future pregnancies
Breast size before, during, and after pregnancy
Mammography history (recommended for patients >35 years of age and those with significant breast cancer risk)
Patients without significant history should have a mammogram every 2 years starting at 40 years of age, and every year beginning at 50 years of age. 7
Previous surgeries or procedures on breasts
Previous cosmetic procedures
Tobacco or nicotine replacement use, drug use
Anticoagulation use
Current breast size
Desired breast size (many patients will bring pictures to clinic)
Physical Examination
Breast examination
Masses, dimpling, discharge, lymph nodes
Cancer screening
Skin quality
Stretch marks, tone, elasticity
Asymmetries: Chest wall, scoliosis, breast
Difference in breast volume
Difference in inframammary fold (IMF) height
Difference in nipple-areolar complex (NAC) height
Soft tissue pinch test
Ã2 cm, may obtain a better result with a submuscular implant placement
Ptosis (see Chapter 53)
Mild ptosis is improved by augmentation.
Moderate to severe ptosis may require mastopexy.
Measurements (patient sitting up straight)
Breast width at its widest point
Breast height
Intermammary distance
Mark true midline of the chest
Mark IMF
Height, weight, body frame (small to large)
Sternal notch to nipple (SN-N)
Nipple to inframammary fold (N-IMF) during stretch
Base width (width of breast base)
Parenchymal coverage (pinch test)
Superior pole
Lower pole
Anterior-pull skin stretch (centimeters of anterior stretch with pull at edge of areola)
Parenchymal fill (percentage of skin envelope filled by parenchyma)
Photographs (all jewelry and identifying markers removed) (see Chapter 3)
Chin to below navel
Front, lateral, oblique, with arms at rest and elevated
Point out and document
Chest wall deformities
Spinal curvature
Asymmetries (nipple shape and size, nipple position, IMF position, breast size, breast ptosis)
Informed Consent
Not just signing a paper
Photographic review
Note asymmetries, ptosis, cleavage.
Note that asymmetries, ptosis, and cleavage are often unchanged or even accentuated by breast augmentation alone.
Implant selection
Review and discuss risks and benefits of implant type, texture, volume, positioning, and access incisions.
Review and discuss previous restrictions on silicone implants.
The patient must be thoroughly informed about:
Risks and complications
Bleeding
Infection
Capsular contracture
Change in nipple and skin sensation
Scarring
Breast calcifications
Breast implant-associated anaplastic large cell lymphoma (BIA-ALCL)
Seroma
Hematoma
Breast venous thrombosis
Implant failure
Implant extrusion
Changes in mammography detection
Implant visibility and palpability
Implant wrinkling or rippling
Implant malposition or displacement
Leakage of filling substance
Rare difficulties with breast-feeding
Chest wall deformation
Animation deformities (if submuscular)
Limitations of high-impact activity
Unsatisfactory result
The need for additional surgeries
Many insurance carriers do not cover cosmetic operations, correction of complications that may arise from surgery, and changes that necessitate revision surgery.
Implant weight, aging, weight loss or gain, and pregnancy will result in expected changes in breast appearance.
Benefits
Enhances natural body contour
Corrects loss of volume after pregnancy and lactation
Balances asymmetries
Replaces ruptured or displaced implants
Alternatives
Silicone versus saline
Fat grafting
Autologous tissue transfer
No surgery
Can use official ASPS informed consents
Document desired implant type, size, and shape discussed with patient.
Equipment
Instrumentation
Double hooks
Lighted breast retractor versus headlight
Army-Navy retractors
Extended Bovie tip
Endoscopic retractor (transaxillary approach, transumbilical augmentation)
Closed-loop saline-filled setup (saline-filled implants)
Implant sizers (if applicable)
Triple antibiotic solution
50,000 units bacitracin, 1g cefazolin, 80mg gentamicin per 500 ml saline solution (may reduce infection rate and capsular contracture) 8
Keller funnel (Allergan)
Allows no-touch insertion of silicone implant through minimal-sized incision
Implants
Filler Material
Saline
Advantages
Historically lower contracture rates
Adjusts quickly to body core temperature
Leaks easily detected and safely absorbed by body
Size more customizable—easier to adjust for size and correct breast asymmetry
Disadvantages
Wrinkling
Less natural look and feel
Complete deflation with leak
Construction
Silicone shell filled with physiologic saline solution
Silicone
Advantages
More natural feel and appearance than saline implants
Disadvantages
Historically higher contracture rate
Must be ≥22 years of age to receive silicone implant per FDA
Adjusts slowly to temperature change (e.g., implants remain cold after swimming)
Ruptures more difficult to detect and can cause local inflammation and granulomas
MRI recommended 3 years after surgery, then every 2 years to monitor for rupture, as per FDA
More expensive
Construction
Silicone shell with silicone filler
Silicone: Polymer of dimethylsiloxane. Longer chains with greater interchain cross-linking lead to increased viscosity.
Double-Lumen (Becker Implant, Mentor)
Advantages
Natural feel of silicone
Allows postoperative adjustments to inner-lumen saline volume
Useful for asymmetry and for patients uncertain of desired size
Disadvantages
Fill port temporarily implanted, requiring second procedure to remove
Possible fill valve failure
Construction
Outer and inner silicone shell: Outer lumen filled with silicone, and adjustable inner lumen filled with saline
Volume
Patient preference
Sizers put in bra to establish desired volume (not recommended)
Photos of other women
Digital imaging
Surgeon’s experience
125-150 cc to increase by one cup size
Larger body frames require larger implant volumes to increase cup size
Breast analysis
High Five system 9
Objective measures to determine optimal implant and volume
Volume based on breast base width
Add or subtract volume based on skin stretch, breast envelope fill, and N-IMF
Intraoperative breast sizers
Pitfalls of large implant volume
Stretching and stressing of tissues
Atrophy and thinning of parenchyma and skin
Increased palpability
Traction rippling
Caution:
Large implant can have detrimental effects on overlying soft tissues.
Texture
Smooth
Advantages
Thinner capsule formed
Less palpable: Preferable for patients with thin coverage
Disadvantages
Higher contracture rates
Requires larger pocket dissection
Requires displacement exercises to prevent contracture
Textured
All shaped implants are textured to prevent malposition.
Advantages
Lower contracture rate (surface disorients collagen deposition)
Less migration and implant rotation
Disadvantages
Require precise pocket dissection
More palpable
Traction rippling more common
Greater association with BIA-ALCL based on current data
Technique
Intraoperative positioning of implant is critical, because textured surface resists migration or movement in pocket.
Base must be properly oriented along IMF.
Polyu rethane -Covered
Advantage
Dramatically low contracture rates (<1% over 10 years)
Disadvantage
Pulled from U.S. market, because polyurethane breaks down as a carcinogenic compound, although levels likely insignificant
Construction
Polyurethane coating separates over weeks to months and becomes incorporated into the capsule, helping to disperse contractile forces.
Textured implants were developed to mimic the effect of polyurethane on the capsule.
Shape/Dimension
Round (Circular Implant)
Advantages
Offered in many different projections and sizes
Disadvantages
Less natural appearance
Low-profile
Moderate-profile
Moderate-plus-profile
High-profile
Increased projection for given base width
Increased projection with less volume
Advantage with a constricted lower pole or a narrow breast base width
Shaped/Anatomic
Implant height different than width
Increased implant height and projection for a given base width
Upper pole tapered; fuller lower pole, reducing upper pole collapse and filling out lower pole of breast
Most textured to maintain position
Advantages
Designed to give more natural appearance
Less upper pole fullness
More natural upper pole contour
Disadvantage
Must be oriented properly and symmetrically
More prone to malposition
Fewer available implant sizes in the United States
Size
Based on:
Patient’s desired size and projection
Breast base width
Implant should be slightly narrower than the patient’s breast width
Dimensions and compliance of the patient’s breast
High-volume implants (>400 cc) are more prone to complications.
Many surgeons have special consent forms for such implants.
Rule of thumb: 125-150 cc per cup size increase
Senior Author Tip:
While the anatomically shaped implants may help with the creation of natural breast contours, the real advantage of these devices is that they are wrinkle resistant. As a result of the anatomic shape of the shell combined with the more cohesive gel, these devices resist collapse and wrinkle formation which greatly reduces stress on the shell resulting from fold flaw failure. As a result, the rupture rates at 10 years for these devices are impressively low which can make these implants an attractive option for patients and surgeons alike.
Technique
Markings
IMF
True midline
Incisions
Pocket Position
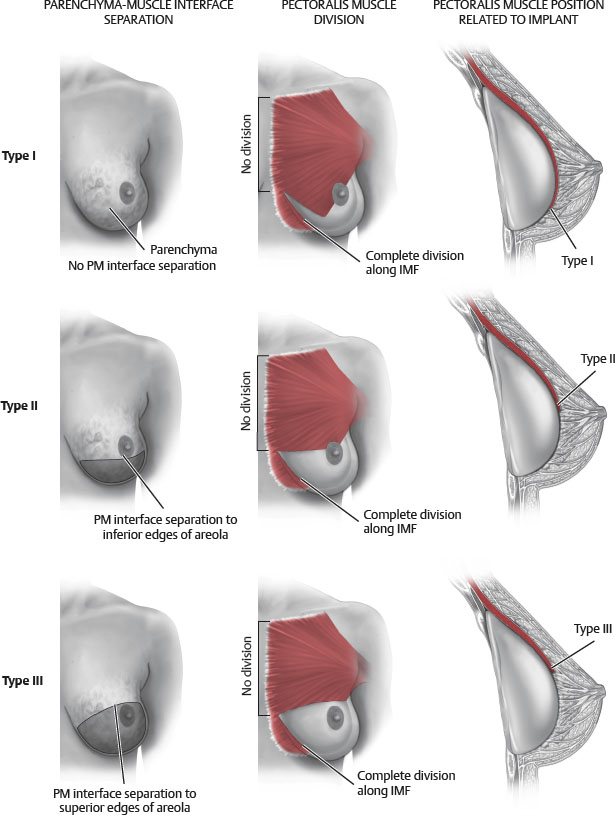
Pocket dissection is based on type of implant (Fig. 52-1).
Smooth gel implants can use larger pockets and displacement exercises to prevent capsular contracture formation.
Textured implants are placed in and are only slightly larger than the footprint of the implant to minimize malposition.
Subglandular/Subfascial
Subglandular: The implant rests under the breast gland.
Subfascial: The implant is placed under the anterior pectoralis major fascia and the pectoralis major muscle.
Advantages
Avoids implant distortion with pectoralis activity and in muscular patients
More anatomic
Better implant projection
Disadvantages
Higher capsular contracture rate
Visible implant wrinkling or rippling, especially if paucity of native breast tissue
Implant edges may be palpable
Interference with mammography
Technique
Dissection on top of pectoralis major, below gland
If pinch test is greater than 2 cm, the implant can safely be placed in the subglandular/subfascial plane.
Thin parenchymal coverage if upper pole pinch test is <2 cm
Total Subpectoral
Rarely performed in cosmetic surgery
Advantages
Lowest capsular contracture rates (<10%)
Thick soft tissue coverage
Good preservation of nipple sensation
Disadvantages
Implant shifts with pectoralis activity
“Dancing breasts” during pectoralis contraction
Implant malposition over time (superiorly and laterally)
Difficult to control upper pole fill
Relative contraindication
Muscular or active patient
Technique
Dissection below pectoralis major but above pectoralis minor
The implant is placed completely under the pectoralis major muscle
Does not disrupt inferior attachments of pectoralis if “total subpectoral”
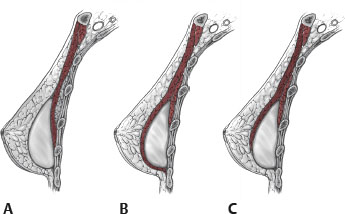
Dual Plane
The origin of the pectoralis major is completely divided from its origin at the level of the IMF, stopping at the medial aspect of the IMF.
The upper pole of the implant is placed under the pectoralis, and the lower pole is placed subglandularly.
The attachments of the pectoralis to the breast parenchyma are selectively divided. (The amount of dissection differentiates dual plane type I, II, and III.)
Advantages
Decreases implant displacement caused by pectoralis contraction
Provides thick upper pole soft tissue coverage with subpectoral placement
Lower capsular contracture rates than with subglandular placement
Increased control of IMF position compared to submuscular
The breast parenchyma and the pectoralis can be dissected apart to adjust for differing types of breasts.
Low contracture rate
Increases implant-parenchymal interface, which expands lower pole and prevents double-bubble deformity
Disadvantage
Usually restricted to IMF incision when performing dual plane II and III
Contraindication
IMF pinch test <0.4 cm
Rationale
Complete muscle coverage restricts expansion of inferior pole, forcing implant superiorly and laterally.
Especially with ptotic and loose breast parenchyma, breast tissue may slide inferior to the axis of the implant while implant remains fixed higher on the chest wall, causing a type A double-bubble deformity.
Dual plane techniques release inferior pectoralis attachments, allowing some pectoralis retraction superiorly.
This maximizes implant contact with lower pole breast parenchyma, with the advantage of upper pole coverage by the pectoralis.
Dual plane type I 10 (Fig. 52-2)
Complete division of the pectoralis from its origin at level of IMF, stopping at the medial aspect of the IMF, in addition to subpectoral dissection
No dissection in the retromammary plane to free the breast parenchyma-muscle interface
Indications: Most “routine breasts”
All breast parenchyma located above the IMF
Tight attachments at the parenchyma-pectoralis interface
Minimally stretched lower pole (NAC-IMF distance 4-6 cm)
Dual plane type II
Complete division of the pectoralis from its origin at level of IMF, stopping at the medial aspect of the IMF
Pectoralis separated from breast parenchyma in the retromammary plane to level of inferior NAC
Indications: “Highly mobile parenchyma”
Most of the parenchyma located above IMF
Looser parenchyma-pectoral attachments (breast tissue much more mobile relative to pectoralis major)
Moderate lower pole stretch (NAC-IMF distance 5.5-6.5 cm)
Dual plane type III
Complete division of the pectoralis from its origin at level of IMF, stopping at the medial aspect of the IMF
Separation of pectoralis from parenchyma in the retromammary plane is continued to level of superior NAC.
Indications: “Glandular ptotic” and “constricted lower pole breasts,” including tuberous breasts
Breasts with glandular ptosis or true ptosis when a third or more of parenchyma is below the projected IMF
Very loose parenchyma-pectoral attachments (parenchyma readily slides off pectoralis surface)
Markedly stretched lower pole (NAC-IMF distance 7-8 cm)
Tight, constricted lower breast with short, tight IMF
Parenchymal maldistribution, tightly concentrated centrally leading to narrow base width
Short NAC-IMF distance (tuberous breasts) (2-5 cm)
Use radial and concentric scoring through breast parenchyma
Senior Author Tip:
It is possible to consider an even more aggressive release of the muscle, essentially separating the breast from the muscle along its leading edge all the way up into the axilla. This allows the muscle to further “window shade” to a location above the NAC. This could be thought of as a dual plane type IV, or as the senior author calls it, a “combination pocket” and results in a great reduction in postoperative breast animation and yet still provides contour softening in the upper inner quadrant of the breast.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree