37 Gynecomastia: Evaluation and Treatment
Summary
Male gynecomastia typically occurs in puberty with the second peak in later life. While most cases are idiopathic and probably related to breast end-organ receptor sensitivity, drugs and medications can influence its occurrence. Insurance rarely covers surgery for this problem.
Some teenagers may outgrow the problem. Tamoxifen and anastrozole may be helpful in treating adolescent cases. Conservative measures are rarely successful in established postpubertal cases.
Surgical intervention is usually curative.
Key Teaching Points
Tamoxifen and anastrozole may benefit adolescents suffering from gynecomastia.
Surgery is a mainstay of treatment in established cases, particularly in the elderly patient.
Liposuction is an essential component of the treatment and maybe adequate in fatty breasts.
Additional surgical excision through a periareolar incision is usually necessary in dense glandular breasts.
Arthroscopic cartilage shavers can be helpful to debulk the gland through remote incisions.
Extreme care should be exercised to ensure that adequate subareolar tissue is left to provide for a smooth convex contour in order to prevent saucer-shaped deformities.
Skin reduction is offered necessary in extreme cases.
37.1 Introduction
Gynecomastia, a pathologic enlargement of the male breast, is a common problem. This condition can be caused by drugs, medications, hormonal imbalances (especially the estrogen/testosterone ratio), abnormal end-organ responsiveness, genetic conditions, and exogenous hormones.
Gynecomastia may occur during two age peaks:
Puberty.
Late adulthood.
During puberty, it is normal for some adolescent boys to develop a degree of breast parenchymal proliferation. Ordinarily, this condition is self-limiting and subsides within 6 to 18 months. When gynecomastia persists, usually in both breasts or occasionally in one breast, it is often embarrassing and psychologically debilitating. Early pubescent cases may be treated effectively with tamoxifen or anastrozole therapy. Removing the excess breast parenchyma is the most effective treatment in established cases.
In elderly men, medical causes such as drug therapy (e.g., testosterone) should be considered and eliminated, because this may have an impact on reversing the condition.
Of increasing importance in this era is the widespread use of recreational and medicinal marijuana, a potent cause of gynecomastia in the male population.
Causes of Gynecomastia
Physiologic:
Puberty.
Advanced age.
Familial.
Idiopathic.
Systemic conditions:
Obesity.
Renal failure (hemodialysis).
Hyperthyroidism.
Hypothyroidism.
Liver disease.
Adrenal tumors.
Hermaphroditism.
Increased estrogen: – Testicular tumors.
Estrogen.
Diethylstilbestrol.
Androgens.
Decreased testosterone:
Klinefelter’s syndrome.
Chronic illness.
Orchiectomy.
Drugs:
Alcohol.
Amphetamines.
Chemotherapeutic agents.
Cimetidine.
Digitalis.
Haldol.
Hydroxyzine.
Isoniazid.
Methyldopa.
Marijuana.
Opiates.
Phenothiazines.
Progestins.
Reserpine.
Spironolactone.
Tricyclic antidepressants.
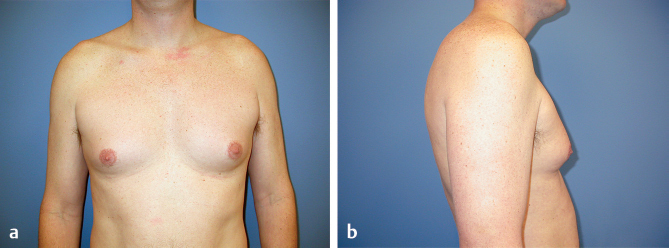
This 18-year-old man had pubertal-onset gynecomastia, which caused him severe embarrassment. His breasts were feminized, with a large central breast parenchymal bud and a modest volume of surrounding breast fat with a body mass index of 25. He was going into the military and requested reduction. A combined resection with liposuction was planned (▶Fig. 37.1).
Breast development may be severely asymmetrical in some of these patients. This patient had modest stage I gynecomastia on the right but a more extreme grade IV abnormality on the left, with grade 3 ptosis and at least a B cup size with dilation of the areola. Management of the left side would require breast reduction with nipple transposition. This degree of deformity is impossible to conceal even with loose-fitting clothing and may have profound psychological consequences (▶Fig. 37.2).

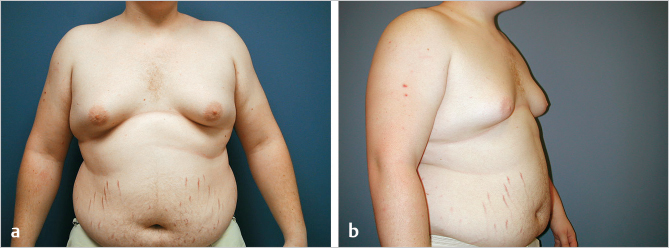
Obesity accentuates the problem, as was evident in this 16-year-old obese adolescent boy with pubertal gynecomastia. No underlying hormonal or chromosomal defects were apparent. As in women, breast tissue contains a significant amount of fat in these cases. Liposuction is invaluable when surgically reducing the breasts in such patients (▶Fig. 37.3). For overweight individuals, the additional anterior and lateral chest fullness must be treated with suction to obtain an acceptable contour.
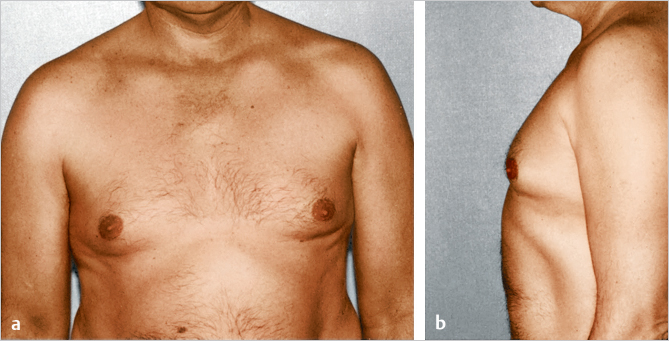
Marijuana usage is commonly linked to gynecomastia. This 55-year-old man developed gynecomastia after frequent cannabis usage (▶Fig. 37.4). Men taking estrogens or testosterone inhibitors for the management of prostate cancer and patients with liver disease who have a hormonal imbalance are also susceptible to this condition. Patients with gynecomastia usually exhibit a proliferation of fatty tissue and breast parenchyma in the chest wall area.
Men can develop gynecomastia as a result of taking anabolic steroids to enhance athletic performance or for bodybuilding. These patients usually have low body fat, but the exogenous testosterone suppresses the endogenous testosterone, permitting increased production of estrogens, which upsets normal hormonal ratios contributing to the development of gynecomastia. The resulting feminized breast appearance, often associated with genital atrophy, is especially distressing to these young men, who are attempting to achieve a more masculine physique.
37.2 Patient Evaluation
A detailed patient evaluation should be completed before the treatment of gynecomastia or a breast mass to determine whether the breast enlargement has a hormonal, oncologic, or idiopathic cause. In addition, in prepubertal gynecomastia patients, the duration of symptoms and psychological impact should be evaluated. Breast enlargement resolves with expectant management in most of these patients.
The physical examination includes the following:
A survey to determine the treatable causes of breast enlargement.
The breast is carefully palpated for the presence of discrete lesions and to assess the amount of fat and parenchyma and their relative proportions.
The axillary space is examined for adenopathy.
Further evaluation is essential when discrete masses indicate possible malignancy.
If the breast enlargement is primarily attributable to excess adipose tissue, liposuction may be the only therapy needed.
Male patients should be evaluated for the following:
Appropriate secondary sexual characteristics.
Gonadal development.
Appropriate diagnostic studies if necessary, particularly for patients taking anabolic steroids.
Liver and cardiac problems.
Gynecomastia can be graded on a scale of I through III, depending on the degree of breast ptosis present. A simple classification system is helpful in determining the appropriate treatment (▶Table 37.1).
Rohrich has added a more extensive classification based on breast tissue composition and size (▶Table 37.2).
37.3 Treatment Options
Available Treatment Options for Gynecomastia
Liposuction reduction (power-assisted or ultrasound-assisted).
Direct excision augmented by liposuction.
Breast reduction with nipple transposition or nipple grafting in severe cases.
Patients with gynecomastia typically have subareolar glandular tissue surrounded peripherally by fibrofatty tissue.
Technical Pearl
Young males tend to have a preponderance of dense breast parenchyma with relatively little surrounding fat, unless they are overweight, whereas elderly males often have a significant component of breast fat centrally and peripherally.
The breast consistency will help determine which of the previous treatment modalities will be most effective in improving a patient’s clinical outcome.
In my experience, standard liposuction effectively reduces the bulk of breast fullness only in overweight patients or men who have a high percentage of fat as a component of their breast enlargement. If breast enlargement is primarily attributable to excess fatty tissue, as in patients with pseudogynecomastia with large fatty deposits in the breast region but not a large volume of fibrous breast parenchyma, liposuction alone may provide adequate contour improvement, without the breast scars from direct excision of the breast. Liposuction can be performed through a distant site such as the axilla or inframammary region, obviating the need for scars on the breast. In addition, the resection can be tailored laterally to provide good contour while promoting skin contraction.
Unlike loose subcutaneous fat, dense, hypertrophied fibrous breast parenchyma tends to be resistant to removal with conventional liposuction techniques. In this situation, power-assisted liposuction (PAL) or ultrasound-assisted liposuction (UAL) may be a useful adjunct, often aided by sharp excision. PAL or UAL permits cavitation and emulsification of the fibrous breast parenchyma. Standard liposuction is then used to remove excess fat and evacuate the liquefied tissue remaining after cavitation. Endoscopic mastectomy may also be a useful technique in this setting.
When significant breast parenchyma is present, I prefer to perform direct excisional reduction coupled with liposuction of the breast periphery. In addition, I prefer to use PAL, although UAL is also helpful in these patients.
Suctioning before sharp excision appears to reduce the incidence of postoperative hematoma and promotes skin contraction and a smoother contour at the resection margins. This traditional approach may be used with endoscopic visualization through axillary incisions. The endoscopic technique makes it possible to excise this parenchymal tissue through limited, distant incisions, thereby avoiding a breast or areolar scar, which is a source of concern to most men. Excess fatty tissue is treated with liposuction.
37.4 Power- and Ultrasound-Assisted Liposuction
In patients who have dense breast parenchyma in addition to fatty tissue, I perform liposuction initially after infiltration of tumescent fluid using a superwet technique (1:1 ratio) or tumescent technique (3:1 ratio). The remaining dense subareolar glandular tissue is treated with ultrasound energy or PAL. Results tend to be improved with the use of UAL compared with conventional mechanical PAL, although seromas are more prevalent with UAL. The ultrasound probe is introduced through an axillary or inframammary fold incision. It is advanced slowly through the dense parenchymal tissue to allow the energy to slowly cavitate and then emulsify the breast parenchyma. The remaining fluid is evacuated using standard liposuction. A drain and compression dressing are used postoperatively. Open surgical excision, either through traditional periareolar incisions or with endoscopic assistance through the axilla, is used if PAL or UAL does not achieve sufficient correction.
Technical Pearl
In recent years, I have relied more heavily on surgical excision coupled with power-assisted liposuction than suction alone, as liposuction has difficulty coping with dense glandular tissue.
37.5 Technique Using Liposuction Alone
Surgical Plan
Preoperative marking.
Tumescent infiltration.
Liposuction of breast periphery and gland (PAL or UAL).
Closure.
37.5.1 Operative Technique
Positioning
The patient is marked in the erect position and is placed in the supine position with the arms abducted to 90 degrees. While this is the traditional positioning for most breast surgery, it can be argued that there is benefit in leaving the arms at the sides in order to gain a better sense of how much resection to perform without leaving residual deformity. It has been my experience that even when the chest wall looks very well contoured on the table with the arms abducted, patients notice small amounts of residual tissue when the arms are at their sides.
Tumescent Infiltration
A 3- to 4-mm incision is made in each axillary fold. The standard wetting solution is infiltrated into the chest wall and breast, using either a superwet or preferably tumescent technique.
Liposuction
A 3- or 4-mm blunt-tip, three-hole cannula is inserted and the anterior chest wall and breasts are suctioned. In patients with large amounts of adipose tissue I will often start with a 5-mm cannula reducing subsequently to smaller cannulas for feathering of the peripheral contours. Suctioning is performed in a radial fashion, using multiple, smooth strokes. The area of central fullness as well as the entire chest wall is treated. Considerable care shouldbe taken not to oversuction the region, which can create a saucer-shaped deformity.
After the initial suctioning is completed, focused suction is used to treat the firm mass in the subareolar region. If UAL is used, the amplitude is increased, and the tissue is elevated manually to facilitate passage of the cannula. When PAL is used, I tend to reduce the cannula size in order to allow easier passage through dense glandular tissue and I prefer multiple hole devices or spiral hole cutting cannulas in order to achieve adequate penetration and tissue removal. This tissue is difficult to remove adequately and care must be taken to achieve symmetry Approximately 10 mm of tissue, depending on the thickness of the chest wall fat, is left on the flaps and slightly more beneath the nipple–areola to avoid depression in this region.
Closure
Care should be taken to ensure that these incisions are well-closed as well as being as short as possible. Although they are peripherally placed in general, they can often be visible especially if placed lower down on the lateral chest wall, which gives easier access than incisions placed toward the anterior axillary fold.
37.5.2 Clinical Example
This 48-year-old man developed gynecomastia after undergoing treatment of metastatic prostate cancer. His breasts were uncomfortably full, and their large size limited his choice of clothing and physical activity. He requested correction of the gynecomastia, with minimal scars. Axillary and inframammary approaches were used. Wetting solution was infiltrated throughout the breast region. Liposuction was used to reduce the fatty tissue excess in the overall breast and upper and lateral chest regions. The remaining central breast parenchyma was treated with ultrasound energy. The ultrasonic probe was effective in cavitating and emulsifying the breast parenchyma so that the excess breast tissue could be removed. He is shown 2 months after surgery. Although there is some residual postoperative edema and the inframammary access site is visible, he is delighted with the result and is no longer embarrassed about the appearance of his breasts. The associated discomfort is also alleviated. Notice that the inframammary incisions are far more visible and intrusive than the laterally placed incisions. (▶Fig. 37.5).

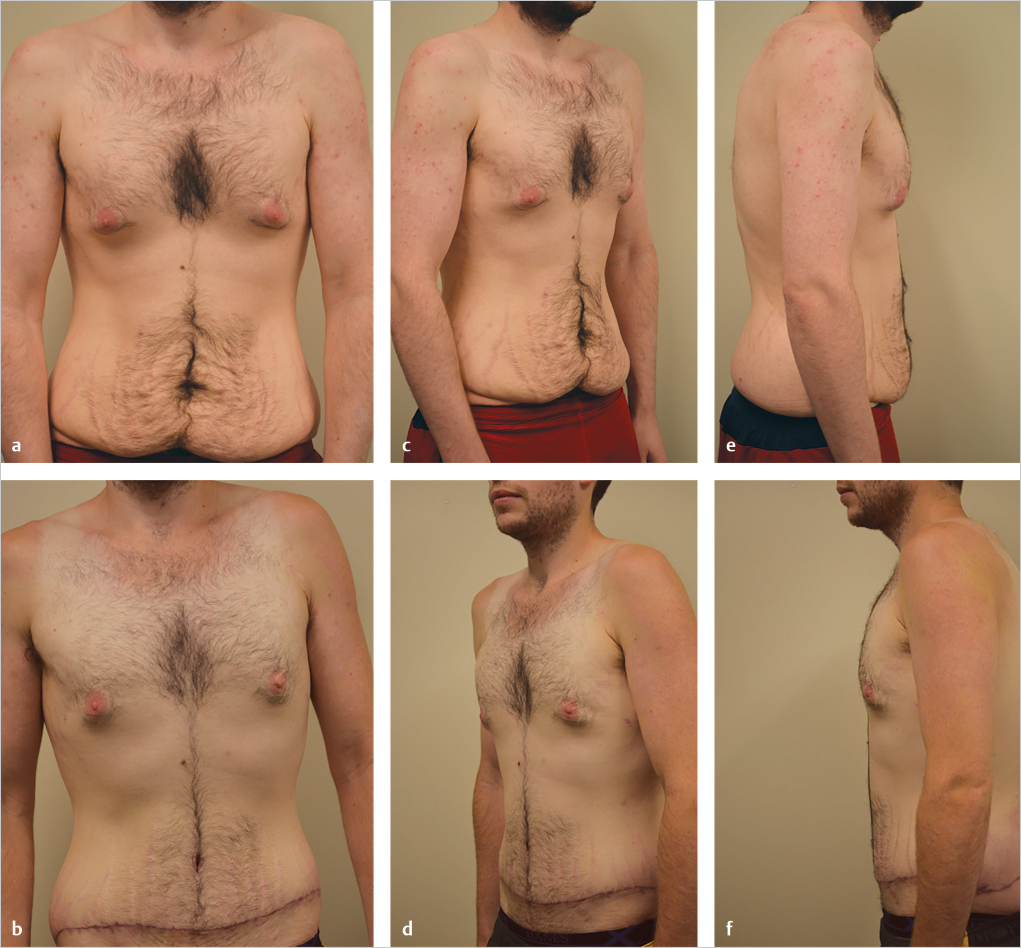
This 32-year-old Caucasian male with gynecomastia presented for body contouring after massive weight loss of 180 pounds with diet and exercise. He had residual glandular hypertrophy with minimal surrounding adipose tissue present. He was very reluctant to have breast scars. Reduction was achieved with PAL. Lateral access incisions were used. Note the slight residual bulge due to difficulty removing dense glandular tissue with liposuction alone (▶Fig. 37.6).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








