35 Free Nipple Graft Technique
Summary
Free nipple grafts or nipple reconstruction reductions are rarely needed in clinical practice. They should only be used in patients with extremely long ptotic breasts into any of the standard pedicled techniques run too high a risk of skin and fat necrosis. Patients should be warned about partial graft take and depigmentation issues when nipple grafts are used. Nipple reconstruction techniques will require areola tattooing postoperatively.
Key Teaching Points
The nipple graft technique eliminates concerns about nipple viability and fat necrosis accompanying massive reductions in extremely large-breasted patients.
Nipple grafting can be accompanying by blistering of the graft resulting in patchy color loss.
Nipple grafts may have poor projection if thinned excessively.
The fishtail technique obviates any problems with graft take or depigmentation. It does, however, require subsequent tattooing of the areola.
35.1 Introduction
As a general guide, I am wary of performing inferior/central pedicle reductions in patients with nipple-to-notch measurements greater than 37 cm or inferior pedicle lengths greater than 25 cm, unless the pedicle base is extremely wide.
In my experience, the risk of fat necrosis and nipple blistering is higher in these patients. A simple lower and lateral breast resection (as described in the inverted-T pedicle technique) combined with a free nipple–areolar graft provides a significant reduction in volume without concern for nipple necrosis.
Technical Pearls
Volume reduction can be more dramatic than conventional pedicle techniques, because the volume of a pedicle is completely negated.
Volume is preserved entirely on the upper breast flaps, creating a better short- and long-term breast shape with less of a tendency to bottoming out.
Nipple–areolar survival approaches 100% when this technique is used with a well-applied bolster dressing.
Fat necrosis and nipple–areolar devascularization that may occur after complex resections or when large pedicles are developed for women with very large breasts with compromised microcirculation are minimized.
Liposuction reduces lateral breast and axillary fullness allowing additional volume reduction.
In patients of color, nipple–areolar depigmentation may occur even when grafts appear to have taken well.
Loss of nipple sensation may occur either partially or completely in these individuals. Patients must be warned of these possible complications preoperatively. In such cases, a nipple reconstruction with modified fishtail flaps can provide an excellent facsimile of a nipple when coupled with areolar tattooing.
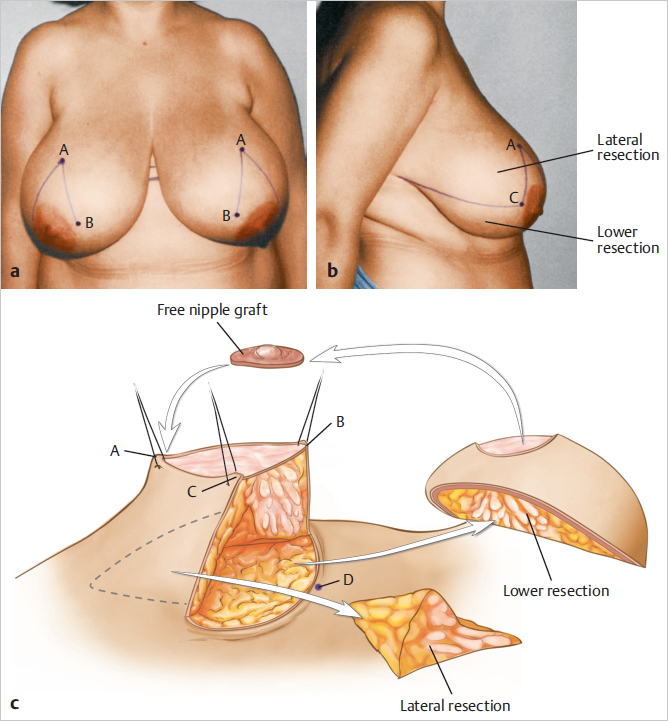
This woman, who wore a 40DDD bra, requested reduction to a more comfortable size to relieve the pain in her back, bra strap grooving, and constant moisture beneath her breasts. She had two teenagers and did not plan to have any more children. She had smoked two packs of cigarettes a day for 20 years and recently stopped. Because of the large breast reduction, history of heavy cigarette smoking, functional considerations, and distance required for pedicle transfer, a free nipple graft technique was selected (▶Fig. 35.1).

Surgical Plan
Preoperative markings to delineate the future site of the nipple as well as areas of central and inferior breast resection.
Liposuction laterally if necessary to reduce lateral fullness.
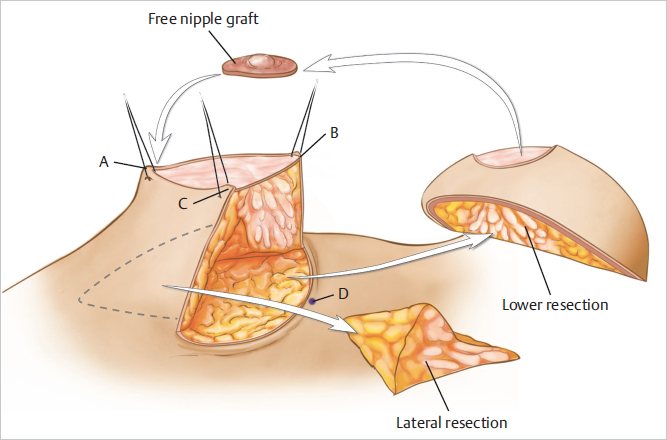
Harvesting of the nipple–areola as a full-thickness graft approximately 40 mm in diameter.
Resection of breast parenchyma inferiorly and laterally.
Closure of the breast as an “inverted-T” Wise pattern.
Deepithelialization of the areolar site at the appropriate position and suture of the areolar graft, which is secured with a tie-over dressing.
35.2 Technique
35.2.1 Markings
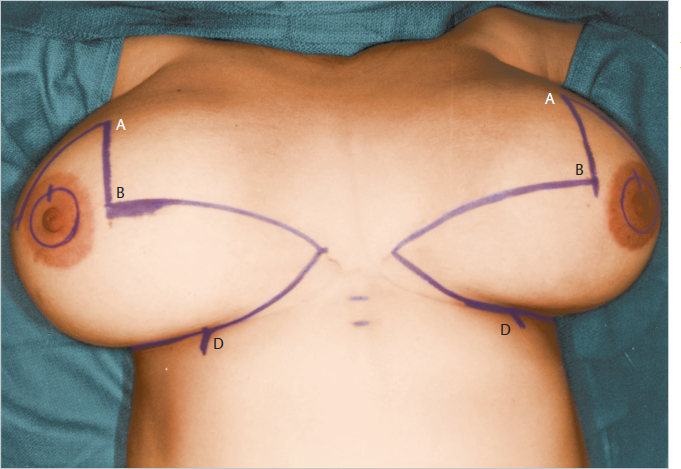
Preoperative markings identify the point of the areolar apex (point A) and the position of the future inframammary fold (IMF). This is determined with the weight of the breast supported to prevent point A from moving upward after the resection, thus displacing the nipple upward. The larger the breasts, the greater the likelihood the remaining breast will lift upward after the resection, leaving the nipple–areola too high (▶Fig. 35.2).
The final IMF incision is marked with the patient supine (▶Fig. 35.3).
35.2.2 Harvesting the Free Nipple Graft
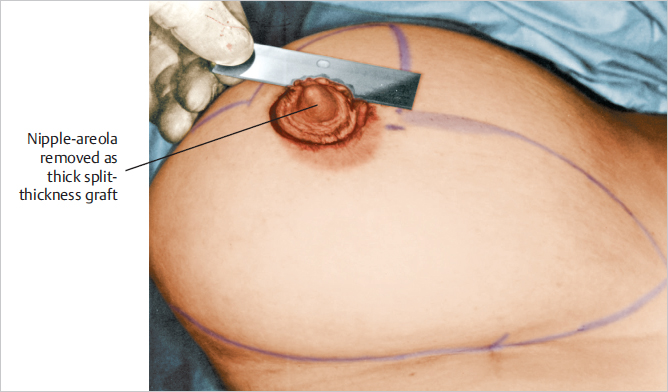
An incision is made around the areola, and the nipple–areola is removed as a thin full-thickness skin graft. The nipple is preserved in a sponge soaked in saline solution for grafting at the end of the procedure (▶Fig. 35.4).
35.2.3 Parenchymal Resection
The inframammary incision is made, and the breast is lifted off the pectoralis major fascia with electrocautery for a distance of only 5 cm.
Technical Pearl
The breast resection should be beveled from above downward to prevent undercutting of the upper breast flap and over-resection.
Many women with gigantomastia tend to be very ptotic, and a majority of their breast volume lies below the horizontal equator of the breast. If these precautions are not taken, lower pole over-resection will occur and the upper pole volume will be grossly inadequate (▶Fig. 35.5).
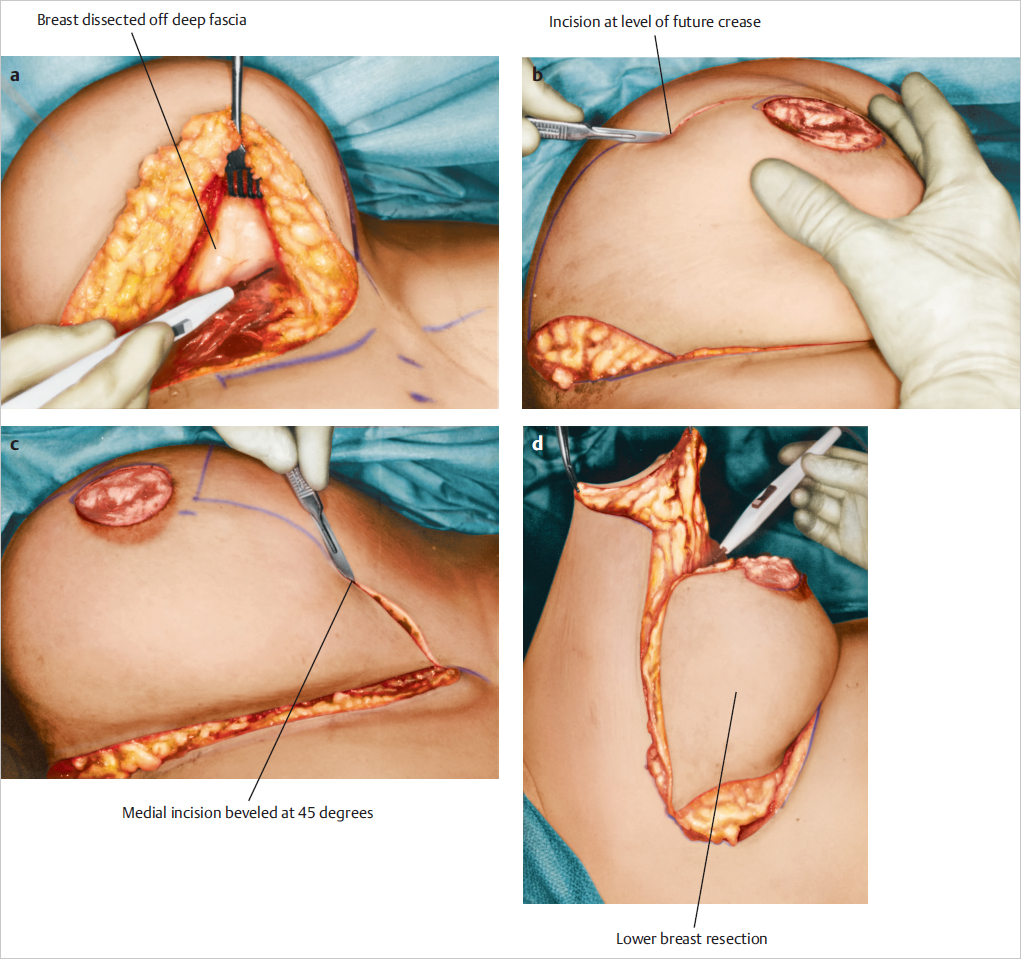
After the central inferior resection is performed, the breast is lifted from the chest wall and markings are made laterally to identify any lateral parenchyma for additional deep lateral excision to achieve debulking of the lateral breast fullness. This is an optional maneuver, because some women have relatively little tissue in this area, and it may need to be preserved for central fullness when the lateral and medial skin incisions are approximated. Liposuction can be used as an alternative to sculpt this area (▶Fig. 35.6).
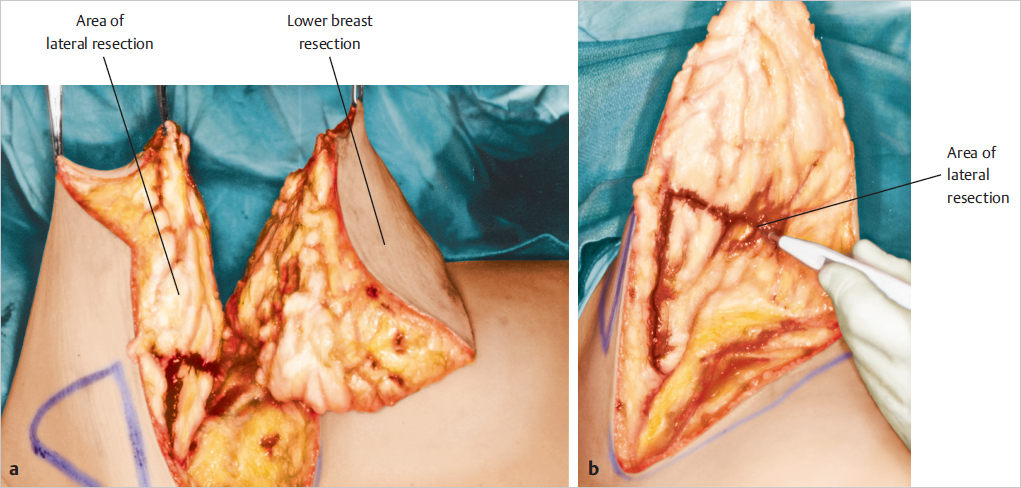
This resection permits some narrowing of the breast during closure. The inferior and lateral resected portions of the breast parenchyma are shown (▶Fig. 35.7).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








