34 Central Mound Inferior Pedicle Technique
Summary
The central mound inferior pedicle technique incorporates multiple perforators from the thoracoacromial and internal mammary source vessels.
This technique preserves intercostal nerve supply to the nipple, improves the likelihood of breast-feeding postoperatively, and enhances upper and medial fullness due to tissue preservation in these areas.
Key Teaching Points
The new nipple level should be marked with the weight off the lower pole of the breast in order to prevent areola show above the edge of the patient’s bra.
The vertical incisions should be cut in a relatively narrow angle inverted V such that the vertical limbs just skirt the areola initially. More skin can always be removed later during closure but tension should be avoided at all costs.
Neurovascular supply can be optimized to the pedicle by leaving modest amounts of breast tissue as “mesenteries” surrounding the central cone of the pedicle. The pectoral muscle need never be seen during this dissection.
Skin flaps should be raised with adequate parenchymal support for vascular inflow and breast shaping, particularly in the upper and medial aspects of the breast.
There should be absolutely no tension at the confluence of the T scar at point D.
34.1 Introduction
The inferior central pedicle technique preserves a central breast mound to maintain the blood supply to the nipple–areola. This is a popular, versatile, and safe technique that relies on perforators from the thoracoacromial, internal mammary, lateral thoracic, and lateral intercostal blood supply and allows selective breast shaping in all quadrants. As an option, an inferior dermal pedicle may also be preserved on the lower portion of the central pedicle to enhance the nipple–areolar blood supply from the subdermal plexus. As such, the technique combines many of the safety features of the superior and superomedial pedicles with the familiarity of an inferior pedicle approach.
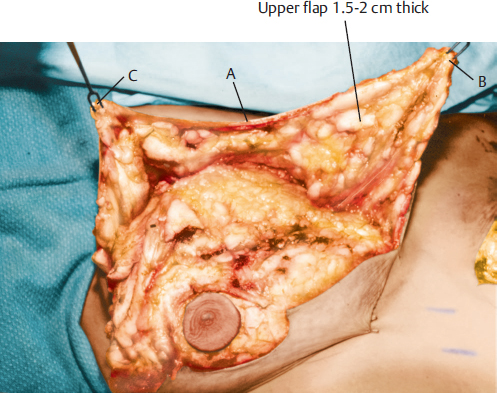
Although the inferior pedicle technique as first described used an inferior dermal pedicle, the primary blood supply is derived from the vascularity of the central mound of breast parenchyma, as described by Hester and colleagues. I personally preserve the inferior dermal strip in all cases to provide an element of dermal support, but there are no scientific data to indicate that nipple blood flow is improved by preserving this dermal element. The skin flaps (above the future inframammary crease line) are elevated as thick (at least 1.5–2 cm) flaps, and breast tissue is removed tangentially, medially, laterally, superiorly, and inferiorly from the superficial surfaces of the central breast mound tissue. More tissue is removed from the primary area of breast hypertrophy: the lateral and inferior portions of the central mound. The breast parenchyma attached to the resected skin in the lower portions of the breast constitutes a sizable portion of the tissue resection (▶Fig. 34.1).

Conservatism is the wisest course of action. Over-resection of breast parenchyma from the upper and medial breast area can create flattening and deformity in an area where most women prefer fullness. It is essential to preserve medial, lateral, and superior mesenteries of breast tissue overlying the pectoralis major muscle in an effort to improve nipple blood supply and sensation. The pectoralis major muscle should not be visualized at all in this procedure as a consequence.
The inferior pedicle technique has a better likelihood of preserving breast sensation and lactation potential and permits more versatility in moving the nipple–areola than is possible with the superior pedicle techniques. The procedure does not narrow broad-based breasts nearly as well as vertical breast reduction, but it provides considerable flexibility for controlling breast size, shape, and volume. Unfortunately, it is more prone to bottoming out with time than the superiorly based pedicle techniques. Resections in several areas of the breast make this procedure more complex and obtaining symmetry more challenging compared with those described previously.
Surgical Plan
Projected amount of reduction and the future shape of the breasts.
Preoperative markings to denote the future site of the nipple–areola and inframammary incisions.
Liposuction of the lateral breast region if excess fullness is present.
Preservation of the nipple–areola with a 38- to 42-mm diameter and deepithelialization of the upper V and, optionally, the inferior dermal strip.
Resection of breast parenchyma and skin from the lower and upper breast regions.
Preservation of thick skin in breast parenchymal flaps; reflection of flaps to identify the central pedicle.
Resection of the central pedicle from the inferior and lateral portions primarily to obtain a new breast base shape.
Closure of the skin and repositioning and inset of the nipple–areola.
Closure of the inverted-T incision.
34.2 Technique
34.2.1 Markings
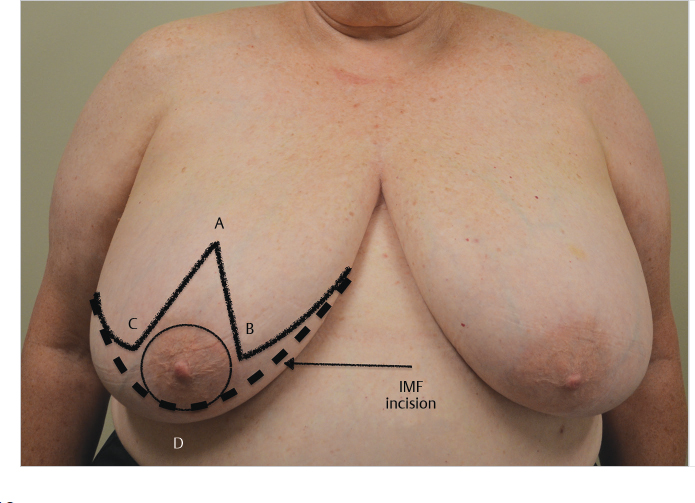
Markings for the inferior pedicle technique are similar to those described for the superior pedicle technique. The new nipple–areolar position is marked on the central breast meridian; marking the width of the V too wide should be avoided to ensure tension-free breast closure of points B and C to D at the inframammary fold.
To accommodate the central pedicle, the central V (B and C points) should diverge only enough to encompass the areola. Additional central breast skin along A to C and A and B within this V is removed at the conclusion of the procedure to avoid a tight-T closure.
Technical Pearl
Tension-free closure at the T is critical to avoid skin necrosis, wound dehiscence, and delayed healing.
During the initial steps of the operation, including the markings for the inferior pedicle and the actual breast resection, the patient is in the supine position with the breast positioned vertically and anatomically over the chest wall. In this position, there is no ptosis, and the perforators from the underlying musculofascial layer will enter directly into the breast. The nipple–areola is positioned centrally over the breast at the fourth intercostal space (▶Fig. 34.2).
34.2.2 Liposuction
I routinely perform dissection of the tail of the breast in an effort to debug the lateral chest wall and redefine the lateral mammary crease. The inverted-T skin pattern has a tendency to leave this area ill-defined due to the tension created laterally at closure, like the section gives the surgeon an opportunity to re-create this anatomical boundary more precisely.
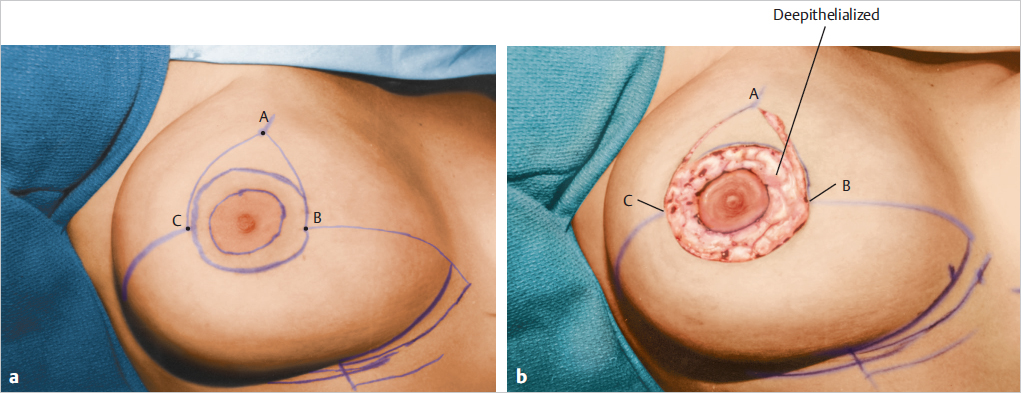
34.2.3 Areolar Incision and Periareolar Deepithelialization
The nipple–areolar diameter is marked at 42 mm with the areola relaxed. With the nipple–areola positioned centrally above the breasts and chest during the resection, an incision is made around the areola, and the circumareolar deepithelialization is performed using scissors or a scalpel. The main source of the blood supply to the nipple–areola will be the underlying breast parenchyma and perforating underlying vessels; however, some additional blood supply is provided by the subdermal plexus (▶Fig. 34.3).
34.2.4 Breast and Skin Flap Dissection
Periareolar dissection is carried down along the lines joining points AB and AC to a depth of 1.5 to 2 cm. The plane of dissection is then beveled obliquely down toward the chest wall. The upper breast flap is mobilized upward centrally, medially, and laterally with at least a 1.5- to 2.5-cm thickness of breast tissue attached. This thickness ensures maintenance of blood flow to the flaps, avoiding necrosis later, and contributes to postoperative breast contour over the central mound. I tend to leave the upper medial skin flap thicker to optimize cleavage fullness postoperatively (▶Fig. 34.4).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








