33 Superomedial Pedicle Technique with Inverted-T Closure (Wise Pattern)
Summary
The superomedial pedicle technique with inverted-T (Wise pattern) breast reduction is extremely versatile and is applicable to a wide range of breast sizes and shapes. The technique is reliable and safe with robust blood supply. The pedicle transposes easily even with firm parenchyma, making it easier to use than a superior pedicle technique. It removes ptotic breast mass to minimize late “bottoming out”/loss of projection or pseudoptosis. It does have a horizontal scar, but this allows removal of larger amounts of lax skin in very large breasts or skin with poor elasticity. Liposuction laterally can help shorten the horizontal scar and narrows breast width. Careful planning gives reproducible results and excellent symptomatic relief. Appropriate patient selection and good technique minimize complications.
Key Teaching Points
The procedure is easily tailored to any breast shape or size.
Superomedial pedicle allows removal of ptotic tissue, preserves/restores projection and upper pole fullness.
Inverted-T scar/Wise pattern closure allows reduction of excess skin vertically and horizontally.
Lateral liposuction narrows wider breast and lateral chest fat/fullness without extending incision/lengthening scars.
Reproducible and safe technique.
33.1 Introduction
The superomedial pedicle technique with inverted-T (Wise pattern) breast reduction is extremely versatile and is applicable to a wide range of breast sizes and shapes. The technique can easily be scaled up or down. The technique is reliable, as it incorporates both the internal mammary perforator blood supply together with the thoracoacromial supply. The pedicle transposes easily even with firm parenchyma, making it easier to use than a superior pedicle technique. It removes ptotic breast mass to minimize late “bottoming out”/loss of projection or pseudoptosis. It does have a horizontal scar, but this allows removal of larger amounts of lax skin in very large breasts or skin with poor elasticity. The horizontal scar length can be shortened with lateral breast/chest liposuction. This allows removal of large amounts of breast and chest fat to remove weight and narrow the breast while minimizing scar length.
Technical Pearl
A relative contraindication would be prior surgery or trauma to the superomedial breast.
Patients with smaller breasts or those with excellent skin elasticity can have incisions closed with just the vertical scar. For very large breasts (notch–nipple > 40 cm, > 1,000 g resection) or in women with impaired microcirculation (smokers), it can be used with a free nipple graft modification while retaining the benefits of the technique: removal of large volume of parenchyma, reduction of skin vertically/horizontally, narrowing of the breast, and ease of pedicle transition.
Surgical Plan
Preoperative marking: nipple position projected anteriorly from inframammary fold (IMF).
Note asymmetry if present.
Lateral breast/chest liposuction (lateral to anterior axillary fold or along IMF for vertical style closure).
Resection of the inferior breast tissue, extending medial and lateral based on breast size and planned resection volume.
Transposition of nipple–areola to new position.
Reassembly of breast with staples temporarily to assess symmetry.
Placement of drains if used.
Closure of incisions.
33.2 Technique
33.2.1 Markings
The patient is marked in the upright position in the holding area so that final questions can be answered and the patient can participate in the process. The proposed location of the upper border of the areola, which will correspond to approximately 2 cm above the level of the inframammary fold (IMF) projected onto the anterior breast skin (Pitanguy’s point), is marked on the breast as point A (▶Fig. 33.1).
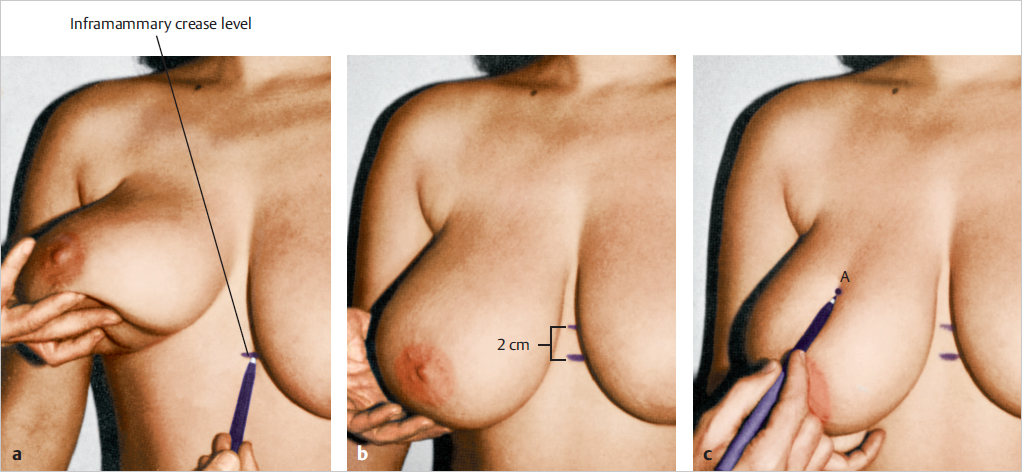
If the weight of the breast is held by the surgeon’s hand, the height will not change as much as if it is marked without supporting the breast.
Technical Pearl
It should be remembered that marking the nipple position with the breast fully dependent results in this point rising upward after breast resection as the nipple is no longer pulled down by the weight of the pendulous breast tissue. This may result in the final nipple position being too high.
The anterior axillary line is noted; the tissue lateral to this will be reduced primarily with liposuction, not resection. This allows gradual feathering of the resected areas. A small mark is made at the current IMF—at the planned location of the new breast meridian, point D. I prefer to complete marking with the patient supine to minimize the effects of gravity.
Gently sloping diagonal lines are drawn from point A medially and laterally to points B and C, respectively, creating an inverted-V shape. These lines are drawn close to the medial and lateral borders of the areola and can be adjusted at the time of skin and parenchymal resection to create a tension-free vertical closure. Their length should correspond to about 9 to 11 cm at most, depending on breast size. This will allow for a final areola diameter of 3.8 to 4.2 cm and vertical limb lengths of 5 to 6 cm.
When supine, I lower the point of the nipple 2 cm from what was marked upright. It is much easier to raise this point at the end of the procedure when insetting the pedicle than to lower it if it is too high. This adjustment of 2 cm is to compensate for skin elasticity, the effect of gravity, and the ease of raising or lowering this point, to tailor the final result to the nipple being at the most projectile point of the breast mound. The IMF is then marked (▶Fig. 33.2).
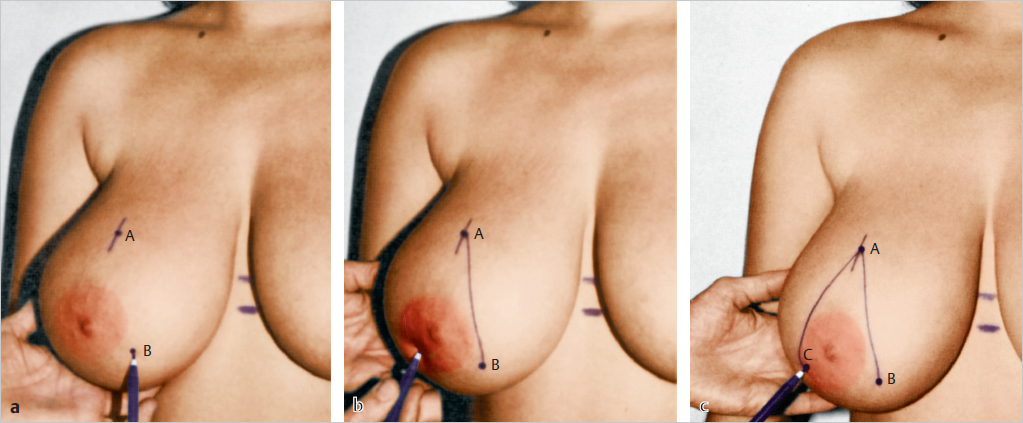
The IMF incision is marked 6 cm either side of the breast median (point D) at the IMF, totaling 12 cm in width (▶Fig. 33.3).
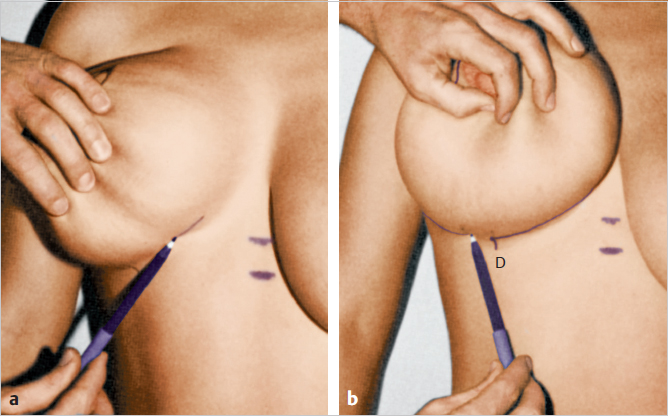
The breast meridian may be obvious while upright in a smaller breast. In a very wide or pendulous breast, it will be set at 11 to 13 cm from the midline—based on chest width. Once the proposed nipple–areolar location and IMF are marked, the width of the resection is marked; this will be the distance from a vertical line imagined up from the breast meridian with the breast first moved medially and then laterally. I use the same tension that gravity imparts on the breast laterally to move the breast medially. The ends of the limbs of the inverted V are connected to the 12-cm mark at the IMF (▶Fig. 33.4).
33.2.2 Tumescent Infiltration
After marking is complete, the operation begins with the patient supine. Tumescent solution is infiltrated into the tissue lateral to the anterior axillary line. Tumescent solution can also be used along the IMF for hemostasis. Typically, 500 mL is used per side. Doing this early allows for the best effect from the epinephrine and also absorption of some of the crystalloid. This allows for a truer estimation of the degree of fat removed. Some tumescent solution may also be infiltrated inferiorly if a vertical style closure is selected. Liposuction inferiorly in this method minimizes “dog-ears” and facilitates tissue contraction. Liposuction is used at the ends of the horizontal incision in the “inverted-T Wise pattern” closure, to minimize “dog-ears” in this location.
33.2.3 Pedicle Deepithelialization
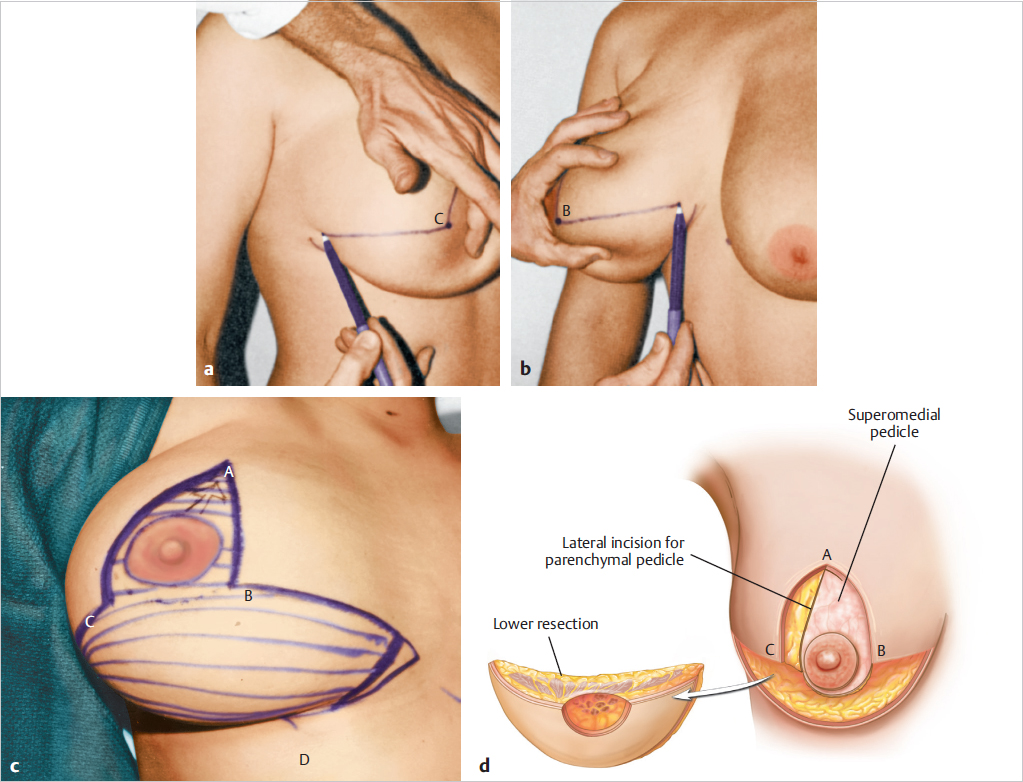
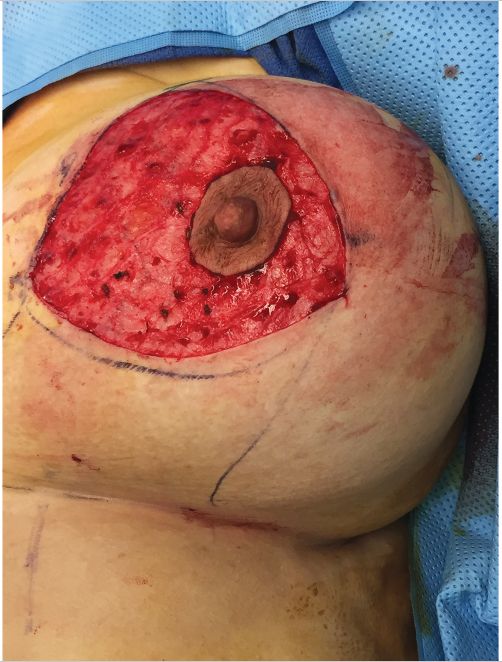
The nipple–areola is reduced to a diameter of approximately 4 cm. The area in the inverted V and outside of the proposed smaller areola is now deepithelialized. The breast tissue/parenchyma remaining with the inverted T of deepithelialized tissue will become the superomedial pedicle (▶Fig. 33.5).
33.2.4 Parenchymal Resection
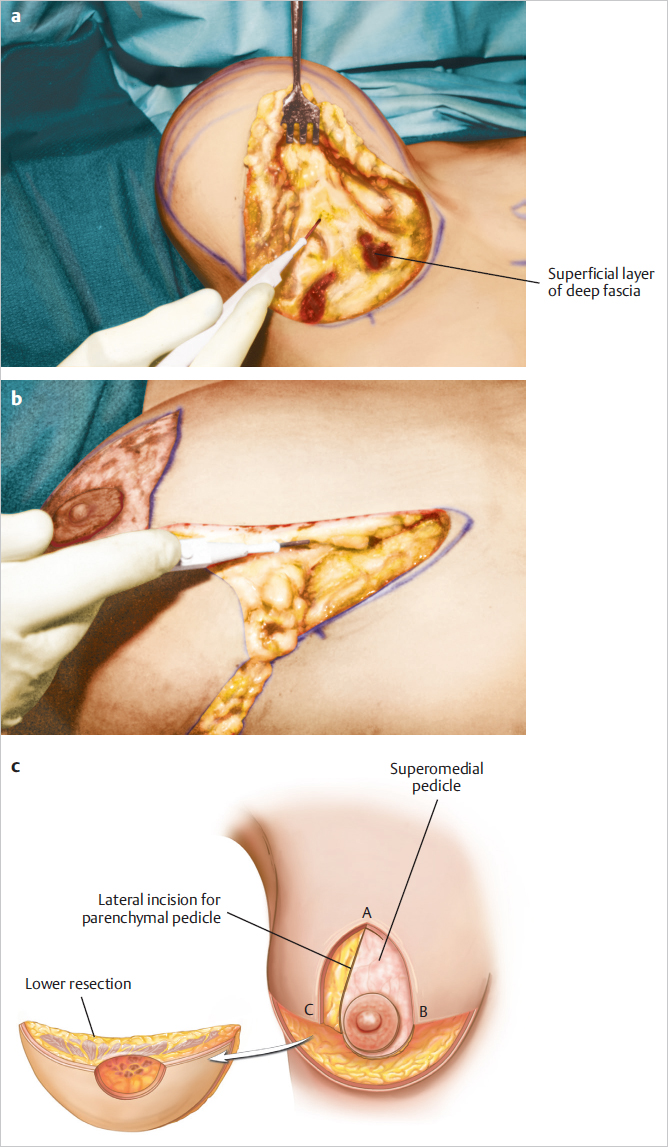
The IMF incision is made and the breast is lifted off the deep surface of the superficial fashion over the lower pectoralis major, serratus anterior, rectus abdominis, external oblique muscles, and up to the level where the areola will be repositioned. Proceeding medial to lateral—allowing gravity to retract the tissues, the breast tissue and skin in the area inferior to the pedicle area is excised. The tissue under the pedicle (in the inverted V) is now tapered at a 45-degree angle until the chest wall muscle fascia is reached (▶Fig. 33.6).
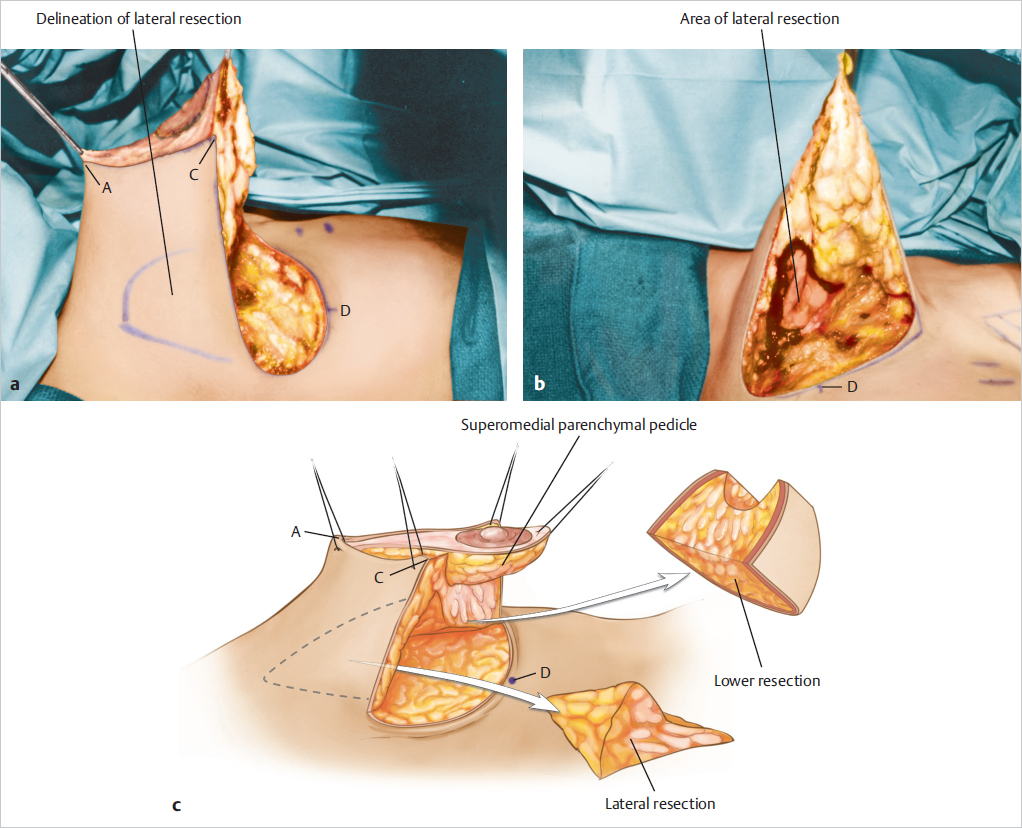
The area for lateral tissue resection is marked. This lateral parenchymal resection will narrow the breast and reduce superior lateral fullness when the breast is closed. This resection allows further reduction in the region of breast fullness and hypertrophy while preserving the functional components of the breast (▶Fig. 33.7).
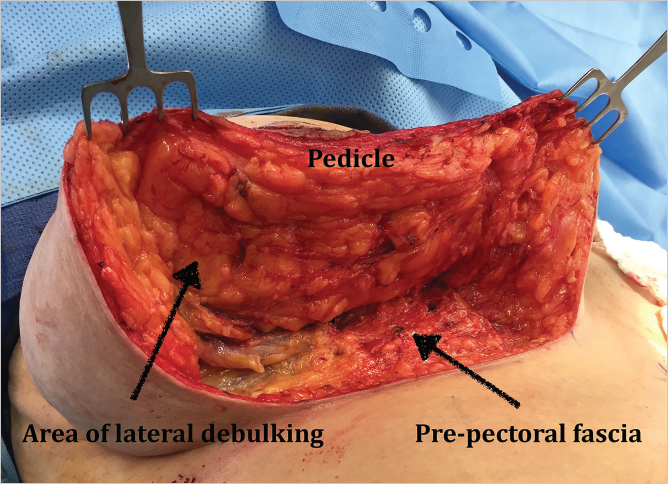
If liposuction is performed, it is convenient to complete it before the lateral resection at the level of the anterior axillary line is complete. This also allows for a smoother transition laterally—tapered with the liposuction, rather than excision (▶Fig. 33.8).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








