Disorders of Hair Follicles and Related Disorders 
Glossary of Terms
Hair Follicle Cycle
The hair follicle undergoes life-long cyclic transformations into three primary phases: anagen, catagen, and telogen (Fig. 31-1).
Figure 31-1. Hair growth cycle Diagrammatic representation of the changes that occur to the follicle and hair shaft during the hair growth cycle. (A) Anagen (growth stage); (B) Catagen (degenerative stage); (C) Telogen (resting stage). (Courtesy of Lynn M. Klein, MD.)
Anagen. Growth phase; lasts variable periods of time depending on body site and age; determines the ultimate length of hair at a site. Anagen hair matrix has rapidly proliferating epithelial cells and is exquisitely sensitive to drugs, growth factors, hormones, stress, and immunologic and physical injury. Destruction of epithelial stem cells results in permanent hair loss. Anagen hairs have pigmented malleable proximal ends (Fig. 31-2A). About 85-99% of hairs will be in this phase, with some individual variation.
Figure 31-2. Hair mount (A) Anagen: note the malleable proximal ends and (B) Telogen: club hairs. [From Goldsmith LA et al. (eds.). Fitzpatrick’s Dermatology in General Medicine, 8th edition. New York: McGraw-Hill, 2012.]
Telogen. Period of relative quiescence, prior to shedding. Telogen hairs are club hairs with depigmented rounded proximal ends (Fig. 31-2B). About 1-15% of hairs are in this phase at any given time.
Catagen. Apoptosis-driven phase between telogen and anagen phase. Duration: few weeks. Only about 1% of hairs are seen in this phase.
Exogen. Active process of hair shaft shedding.
Types of Hair
Lanugo Hair. Soft fine pigmented hair that covers much of fetus; usually shed before birth.
Vellus Hair. Fine, nonpigmented hair; growth not affected by hormones. Genetically determined to produce very small (but functionally fully active cycling) hair follicles located in the dermis.
Terminal Hair. Thick, pigmented hair found on scalp, beard, axillae, pubic area; growth is influenced by hormones. Eyebrow/eyelash hairs are terminal hairs. Produced by large hair follicles located in the subcutis.
Laboratory Examinations
Hair Pull. Scalp is gently pulled. Normally, three to five hairs are dislodged; shedding more hair suggests pathology.
Trichogram. Determines the number of anagen and telogen hairs and is made by epilating (plucking) 50 hairs or more from the scalp with a needle holder and counting the number of anagen and telogen hairs.
Scalp Biopsy. Offers insight into pathogenesis of alopecia.
Nonscarring Alopecia (Table 31-1)
TABLE 31-1 ETIOLOGY OF HAIR LOSS
Etiology and Epidemiology
Etiology. Combined effects of androgen on genetically predisposed hair follicles. Genetics: (1) autosomal dominant and/or polygenic; (2) inherited from either or both parents.
Age of Onset
• Men: May begin any time after puberty, as early as the second decade; often fully expressed in 40s.
• Women: Later—in about 40% occurs in the sixth decade.
Sex. Men >> women.
Classification
Hamilton classified male-pattern hair loss into stages (Fig. 31-3 A):
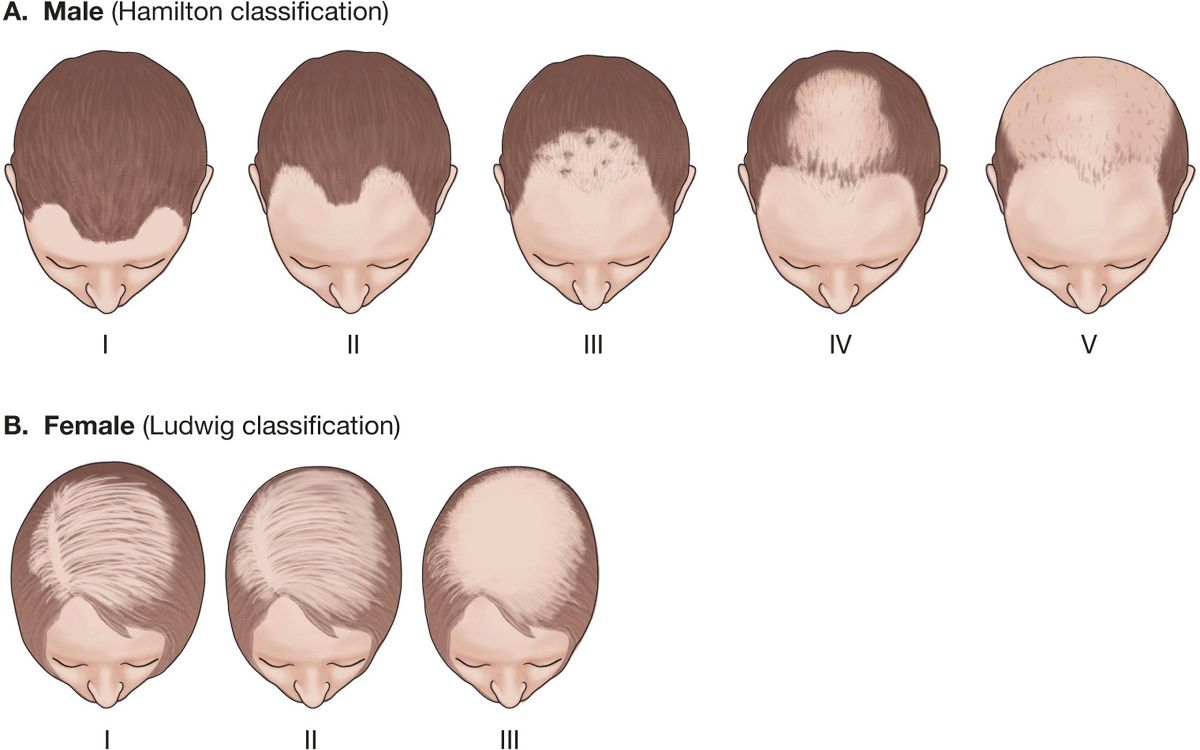
Figure 31-3. Androgenetic alopecia: patterns in men and women (A) Hamilton classified the severity and pattern of hair loss in men into types I to V. (B) Ludwig classified hair loss in women into types I to III.
Type I: Loss of hair along frontal margin.
Type II: Increasing frontal hair loss as well as onset of loss of occipital (vertex or crown).
Types III, IV, and V: Increasing hair loss in both regions with eventual confluent and complete balding of top of scalp with sparing of sides.
Ludwig classified hair loss in women (Fig. 31-3B).
Pathogenesis
• Dihydrotestosterone causes growth of the prostate, growth of terminal hair, AGA, and acne.
• Testosterone causes growth of axillary hair and lower pubic hair, as well as sex drive, growth of the phallus and scrotum, and spermatogenesis.
• Testosterone is converted to (DHT) by 5α-reductase (5α-R). Two isozymes of 5α-R occur: type I and type II.
• Type I 5α-R is localized to sebaceous glands (face, scalp), chest/back skin/liver, adrenal gland, kidney.
• Type II 5α-R is localized to scalp hair follicle, beard, chest skin, liver, seminal vesicle, prostate, epididymis, and foreskin/scrotum.
• Finasteride inhibits conversion of testosterone to DHT by type II 5α-R.
Clinical Manifestation
Skin Symptoms. Most patients present with complaints of gradually thinning hair or baldness.
Skin Findings. Scalp skin is normal.
• In young women, look for signs of virilization (acne, excess facial or body hair, male-pattern escutcheon).
• With advanced pattern hair loss, scalp is smooth and shiny; orifices of follicles are barely perceptible with the unaided eye.
Hair (Fig. 31-4 to 31-7). Hair in areas of pattern hair loss becomes finer in texture (shorter in length, reduced diameter). In time, hair becomes vellus and eventually atrophies completely.

Figure 31-4. Pattern hair loss: male, Hamilton type III A 46-year-old male with bitemporal recession of hairline and frontal thinning of hair.
Figure 31-5. Pattern hair loss: male, Hamilton types IV to V A 37-year-old male with loss of hair in the frontotemporal and vertex areas in a male corresponding to Hamilton types IV and V.

Figure 31-6. Pattern hair loss: female, Ludwig type II A 66-year-old female with diffuse thinning of hair on the crown.

Figure 31-7. Pattern hair loss: female, Lugwig type III with basal cell carcinoma (BCC) A 67-year-old Greek female with advanced alopecia of the crown with BCC arising within it.
• Men usually exhibit patterned loss in the frontotemporal and vertex areas (Figs. 31-4 and 31-5). The end result may be only a rim of residual hair on the lateral and posterior scalp. In these regions, hair never falls out in pattern hair loss. Paradoxically, men with extensive pattern hair loss may have excess growth of secondary sexual hair, i.e., axillae, pubic area, chest, and beard.
• Women, including those who are endocrinologically normal, also lose scalp hair according to the male pattern, but hair loss is far less pronounced. Often hair loss is more diffuse in women, following the pattern described by Ludwig (Fig. 31-3B).
Systemic Findings. In young women with AGA, look for signs of virilization (clitoral hypertrophy, acne, facial hirsutism) and, if present, rule out endocrine dysfunction. However, most women with pattern hair loss are endocrinologically normal.
Differential Diagnosis
Diffuse Nonscarring Scalp Alopecia. Diffuse pattern of hair loss with alopecia areata, telogen defluvium, secondary syphilis, systemic lupus erythematosus (SLE), iron deficiency, hypothyroidism, hyperthyroidism, trichotillomania (pulling of one’s own hair, compulsive), seborrheic dermatitis.
Laboratory Examinations
Trichogram. In pattern hair loss, the earliest changes are an increase in the percentage of telogen hairs.
Dermatopathology. Abundance of telogenstage follicles is noted, associated with hair follicles of decreasing size and eventually nearly complete atrophy.
Hormone Studies. In women with hair loss and evidence of increased androgens (menstrual irregularities, infertility, hirsutism, severe cystic acne, virilization), determine the following:
• Testosterone: total and free.
• Dehydroepiandrosterone sulfate (DHEAS).
• Prolactin.
Other Studies. Treatable causes of thinning hair should be excluded with measurement of thyroid-stimulating hormone (TSH), T4, serum iron, serum ferritin, and/or total iron-binding capacity, complete blood count, antinuclear antibodies (ANA).
Diagnosis
Clinical diagnosis is made on the history, pattern of alopecia, and family incidence of AGA. Skin biopsy may be necessary in some cases.
Course
The progression of alopecia is usually very gradual, over years to decades.
Management
Oral Finasteride. 1 mg po daily. Finasteride has no affinity for androgen receptors and therefore does not block other actions of testosterone (growth of the phallus and scrotum, spermatogenesis, libido). Most men who respond may begin to see benefit in slowing hair loss as early as 3 months. After 6 months, there is a regrowth of terminal hair on the vertex and anterior mid-scalp. If the drug is stopped, however, the hair that had grown will be lost within 12 months. Two percent of men taking finasteride report decrease in libido and erectile function; these effects were reversible when the drug was stopped and disappeared in two-thirds of those who continued taking finasteride.
Topical Minoxidil. Topically applied minoxidil, 2% and 5% solution, may be helpful in reducing the rate of hair loss or in partially restoring lost hair in both men and women.
Antiandrogens. In women with AGA who have elevated adrenal androgens, spironolactone, cyproterone acetate, flutamide, and cimetidine bind to androgen receptors and block the action of DHT. These must not be used in men.
Hairpiece. Wigs, toupees, prosthetics; hair weaves.
Surgical Treatment
Hair transplantation: Grafts of one or two follicles are taken from androgen-insensitive hair sites (peripheral occipital and parietal hairy areas) to bald androgen-sensitive scalp areas. Scalp reduction/rotation flaps.
Etiology and Epidemiology
Etiology. Unknown. Association with other autoimmune diseases and immunophenotyping of lymphocytic infiltrate around hair bulbs suggests an anti-hair bulb autoimmune process; 10-20% of persons with alopecia areata (AA) have a familial history of AA.
Age of Onset. Young adults (<25 years); children are affected more frequently. Can occur at any age.
Prevalence. Relatively common; 1.7% of the US population experiences at least one episode of AA in a lifetime. Varies with geography and ethnicity.
Pathogenesis
• Chronic organ-specific autoimmune disease, mediated by autoreactive T cells affecting hair follicles and nails.
• Follicular damage occurs in anagen followed by rapid transformation to catagen and to telogen; then to dystrophic anagen status. While the disease is active, follicles are unable to progress beyond early anagen and do not develop normal hair.
• Follicular stem cell is spared; hair follicles are not destroyed (there is no scarring).
Clinical Manifestations
Duration of Hair Loss. Gradual over weeks to months. Patches of AA can be stable and often show spontaneous regrowth over a period of several months; new patches may appear while others resolve.
Associated Findings. Autoimmune thyroiditis. Down syndrome. Autoimmune polyendo-crinopathy-candidiasis-ectodermal dysplasia syndrome.
Hair
• Round patches of hair loss. Single or multiple. May coalesce. Alopecia often sharply defined with normal-appearing skin with follicular openings present (Figs. 31-8 through 31-10).
• “Exclamation mark” hairs. Diagnostic broken-off stubby hairs (distal ends are broader than proximal ends) (Fig. 31-8); seen at margins of hair loss areas.

Figure 31-8. Alopecia areata (AA) of scalp: solitary lesion An area of alopecia without scaling, erythema, atrophy, or scarring on the occipital scalp. The short, broken-off hair shafts (so-called exclamation point hair) appear as very short stubs emerging from the bald scalp.
• Scattered, discrete areas of alopecia (Fig. 31-9) or confluent with total loss of scalp hair (Fig. 31-10), or generalized loss of body hair (including vellus hair).
Figure 31-9. Alopecia areata of scalp: multiple, extensive lesions A 46-year-old male with multiple, confluent patches of alopecia areata.
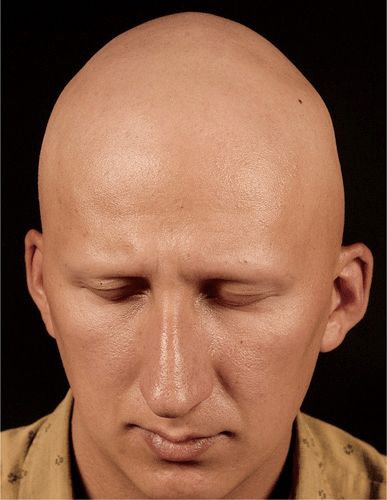
Figure 31-10. Alopecia areata universalis (AAU) This patient has lost all scalp hair (alopecia totalis), eyebrows, eyelashes, beard, and all body hair (alopecia universalis) and has dystrophic (“hammered brass”) nails.
• Diffuse AA of scalp (noncircumscribed) gives the appearance of thinned hair; can be difficult to differentiate from telogen effluvium (TE) or hair loss with thyroid disease.
• With regrowth of hair, new hairs are fine, often white or gray.
Sites of Predilection. Scalp most commonly. Any hair-bearing area. Beard, eyebrows, eyelashes, pubic hair.
• Alopecia arcata (AA): Solitary or multiple areas of hair loss (Figs. 31-8 and 31-9).
• AA totalis (AAT): Total loss of terminal scalp hair.
• AA universalis (AAU): Total loss of all terminal body and scalp hair (Fig. 31-10).
• Ophiasis: Bandlike pattern of hair loss over periphery of scalp.
Nails. Fine pitting (“hammered brass”) of dorsal nail plate. Also: mottled lunula, trachyonychia (rough nails), onychomadesis (separation of nail from matrix) (see also Section 32).
Differential Diagnosis
Nonscarring Alopecia. White-patch tinea capitis, trichotillomania, early scarring alopecia, pattern hair loss, secondary syphilis (alopecia areolaris) (“moth-eaten” appearance in beard or scalp).
Laboratory Examinations
Serology. ANA (to rule out SLE); rapid plasma reagin (RPR) test (to rule out secondary syphilis).
KOH Preparation. Rule out tinea capitis.
Dermatopathology. Acute lesions show peribulbar, perivascular, and outer root sheath mononuclear cell infiltrate of T cells and macrophages; follicular dystrophy with abnormal pigmentation and matrix degeneration. May show increased number of catagen/telogen follicles.
Course
• Spontaneous remission is common in patchy AA but is less so with AAT or AAU.
• Poor prognosis associated with onset in childhood, loss of body hair, nail involvement, atopy, family history of AA.
• If occurring after puberty, 80% regrow hair. With extensive involvement, <10% recover spontaneously.
• Recurrences of AA, however, are frequent.
• Systemic glucocorticoids or cyclosporine can induce remission of AA but do not alter the course.
Management
• Treatment directed at inflammatory infiltrate. No curative treatment is currently available.
• In many cases, the most important factor in management of the patient is psychological support from the dermatologist, family, and support groups (The National Alopecia Areata Foundation, http://-www.naaf. orgl).
• Persons with extensive scalp involvement such as AAT may prefer to wear a wig or hairpiece.
• Makeup applied to eyebrows is helpful. Eyebrows can be tattooed.
Glucocorticoids. Topical. Superpotent agents not usually effective.
Intralesional Injection. Few and small lesions of AA can be treated with intralesional triamcinolone acetonide, 3-7 mg/mL, which can be very effective temporarily.
Systemic Glucocorticoids. May induce regrowth, but AA recurs on discontinuation; risks of longterm therapy therefore preclude their use.
Systemic Cyclosporine. Induces regrowth, but AA recurs when drug is discontinued.
Induction of Allergic Contact Dermatitis. Dinitrochlorobenzene, squaric acid dibutylester, or diphencyprone reported to be successful, but local discomfort due to allergic contact dermatitis and swelling of regional lymph nodes poses a problem.
Oral PUVA (Photochemotherapy). Variably effective, as high as 30%, and worth a trial in patients who are highly distressed about the problem. Entire body must be exposed.
 Human hair has little vestigial function:
Human hair has little vestigial function: Contributes to a psychological perception of beauty and attractiveness.
Contributes to a psychological perception of beauty and attractiveness. Tactile sensation.
Tactile sensation. Protects the scalp, face, and neck from UV solar radiation.
Protects the scalp, face, and neck from UV solar radiation. Reduces heat loss through the scalp.
Reduces heat loss through the scalp. Psychology of hair: Alteration of the “normal” quantity of hair is often associated with profound psychological impact. Loss of scalp hair is considered abnormal in many societies, associating balding with old age (pattern hair loss) or impaired health (chemotherapy).
Psychology of hair: Alteration of the “normal” quantity of hair is often associated with profound psychological impact. Loss of scalp hair is considered abnormal in many societies, associating balding with old age (pattern hair loss) or impaired health (chemotherapy). Excess hair on the face (hirsutism, hypertrichosis) and extremities of women is often considered unattractive.
Excess hair on the face (hirsutism, hypertrichosis) and extremities of women is often considered unattractive. ICD-10: L63-L66
ICD-10: L63-L66 Shedding of hair is termed effluvium or defluvium, and the resulting condition is called alopecia (Greek alópekia, “baldness”).
Shedding of hair is termed effluvium or defluvium, and the resulting condition is called alopecia (Greek alópekia, “baldness”). Individuals are often aware of and very concerned about subtle thinning of the hair.
Individuals are often aware of and very concerned about subtle thinning of the hair. Alopecia classified into:
Alopecia classified into: Noncicatricial alopecia: No clinical sign of tissue inflammation, scarring, or atrophy of skin.
Noncicatricial alopecia: No clinical sign of tissue inflammation, scarring, or atrophy of skin. Cicatricial alopecia: Evidence of tissue destruction such as inflammation, atrophy, and scarring may be apparent.
Cicatricial alopecia: Evidence of tissue destruction such as inflammation, atrophy, and scarring may be apparent.
 Pattern hair loss is the most common type of progressive balding.
Pattern hair loss is the most common type of progressive balding. Occurs through the combined effect of:
Occurs through the combined effect of: Genetic predisposition
Genetic predisposition Action of androgen on scalp hair follicles
Action of androgen on scalp hair follicles In males, pattern/extent of hair loss varies from bitemporal recession, to frontal and/or vertex thinning, to loss of all hair except that along the occipital and temporal margins (“Hippocratic wreath”).
In males, pattern/extent of hair loss varies from bitemporal recession, to frontal and/or vertex thinning, to loss of all hair except that along the occipital and temporal margins (“Hippocratic wreath”). Synonyms: Males: Androgenetic alopecia (AGA), male-pattern baldness, common baldness. Females: Hereditary thinning, female-pattern baldness.
Synonyms: Males: Androgenetic alopecia (AGA), male-pattern baldness, common baldness. Females: Hereditary thinning, female-pattern baldness.
 A localized loss of hair in round or oval areas with no apparent inflammation of the skin.
A localized loss of hair in round or oval areas with no apparent inflammation of the skin. Nonscarring; hair follicle intact; hair can regrow.
Nonscarring; hair follicle intact; hair can regrow. Clinical findings: Hair loss ranging from solitary patch to complete loss of all terminal hair.
Clinical findings: Hair loss ranging from solitary patch to complete loss of all terminal hair. Prognosis: good for limited involvement. Poor for extensive hair loss.
Prognosis: good for limited involvement. Poor for extensive hair loss. Management: intralesional triamcinolone effective for limited number of lesions.
Management: intralesional triamcinolone effective for limited number of lesions.









