24. Treatment of Prominent Veins
Prominent Veins
Can occur in the presence or absence of either symptoms or an underlying functional venous disorder 2
Present in up to 50% of individuals
Risk factors include:
Advancing age
Family history
Ligamentous laxity
Prolonged standing
Increased BMI
Smoking
Sedentary lifestyle
History of trauma
History of venous thrombosis
Arteriovenous shunting
High estrogen states, including pregnancy in women
Telangiectasias, often referred to as spider veins, are most common.
Varicose veins are dilated, elongated, tortuous, subcutaneous veins ≥3 mm. 3
Goals of treatment
Improvement of symptoms (including pain or aching, heaviness, swelling, dry and/or irritated skin, and tightness)
Improvement of appearance
Treatment Options
Conservative Management
Extremity elevation
Exercise
Compression therapy
Sclerotherapy
Indications
Treatment of choice for most superficial leg veins
Appropriate for the treatment of telangiectasias, reticular veins, and small varicose veins 4
Contraindications
Acute venous thrombosis or phlebitis
Pregnancy
Diabetes mellitus (relative)
Moderate to severe peripheral artery disease (relative)
Patent foramen ovale (relative) 5
Preoperative Evaluation
For patients who are asymptomatic but find the cosmetic appearance of their veins distressing, sclerotherapy can be performed after physical examination without further diagnostic studies, because these patients are unlikely to have underlying venous reflux.
Symptomatic patients should undergo further evaluation with venous duplex imaging to identify the presence of superficial or deep venous insufficiency.
Informed Consent
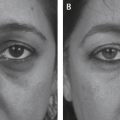
Veins will lighten and become less noticeable but may not completely disappear.
Multiple treatments are typically required to achieve the desired effect.
Hyperpigmentation is a relatively common complication.
Tip:
Veins are documented photographically before each treatment and reviewed with the patient periodically.
Technique
Sclerosants may be used in their liquid form or mixed with room air as a foam, to increase their surface area for the treatment of larger veins.
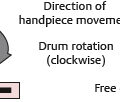
Tessari method involves using a three-way stopcock and two syringes, mixing air with liquid to create a foam. 9
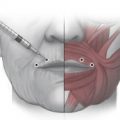
After the sclerosant liquid or foam (with or without lidocaine) is mixed into a syringe at the appropriate concentration, attach the syringe to a 27- or 30-gauge needle.
Place the patient in Trendelenburg position to discourage refilling of injected veins.
Apply alcohol to clean the area, introduce the needle into the vein, aspirate to ensure intraluminal position, and inject using a low pressure, a fixed amount of the sclerosant.
Withdraw the needle, apply compression, and massage the treated area to prevent refilling of the injected vein.
Secure a compressive dressing in place with tape while advancing to other treatment areas.
Senior Author Tip:
The use of 2-way Baxa connectors are an easier, more rapid way to generate foam.
Tip:
Larger underlying reticular veins should be obliterated before more superficial telangiectasias are treated.
Postoperative Care
Compressive stockings should be worn continuously for at least 24 hours and then daily for 2-3 weeks. 10
Avoid strenuous exercise and sun exposure for 2-4 weeks.
Repeat injections are not performed for at least 4-6 weeks.
Clearance of 60%-80% of treated telangiectasias, reticular veins, and small varicose veins can be expected. 11
Senior Author Tip:
In the sclerotherapy consultation, inform patients that new spider veins will occur over time and annual maintenance treatments are encouraged.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree