19. Chemical Peels
Preoperative Evaluation
Consultation with the patient to establish realistic goals and expectations
Does the patient have an indication for chemical resurfacing?
Superficial or deep rhytids/photoaging
Preneoplastic or neoplastic lesions such as actinic keratoses and lentigines
Underlying skin disease such as acne
Pigmentary dyschromias
Demarcation lines secondary to other resurfacing procedures
Any contraindications (Box 19-1)?
Box 19-1% Contraindications for Chemical Peels
Absolute
Poor physician-patient relationship
Lack of psychological stability and mental preparedness
Unrealistic expectations
Poor general health and nutritional status
Isotretinoin therapy within the last 6 months*
Complete absence of intact pilosebaceous units on the face
Active infection or open wounds (such as herpes, excoriations, or open acne cysts)
Relative
Medium-depth or deep resurfacing procedure within the last 3-12 months*
Recent facial surgery involving extensive undermining, such as a facelift*
History of abnormal scar formation or delayed wound healing
History of therapeutic radiation exposure
History of particular skin diseases (such as rosacea, seborrheic dermatitis, atopic dermatitis, psoriasis, and vitiligo) or active retinoid dermatitis
Fitzpatrick skin types IV, V, and VI*
*These contraindications are for medium- and deep-depth peels and do not apply to touchups.
Comprehensive medical and surgical history and physical examination
Bleeding complications/risks from prescription and herbal medicine
Is the patient taking isotretinoin, birth control pills, or immunosuppressants?
Is the patient pregnant?
Patients having a history of cold sores require herpes simplex prophylaxis.
All patients should receive antiviral prophylaxis regardless of history.
Does the patient have a history of hypertrophic or keloid scars?
Does the patient have a history or risk of hepatitis or HIV?
Does the patient have certain cutaneous diseases in the operative site?
Tip:
Patients with rosacea, seborrheic dermatitis, atopic dermatitis, psoriasis, or vitiligo may be at increased risk for postoperative complications, including disease exacerbation, prolonged erythema, contact hypersensitivity, or delayed healing. Patients with rosacea have a vasomotor instability and may develop an exaggerated inflammatory response.
What skin regimens have been used and what were the results?
If patient has history of skin rejuvenation, what type of rejuvenation was done, what were results, and did problems occur?
Identify dyschromias and determine the best depth of peel (Box 19-2).
Determine depth of pigmentation using a Wood lamp.
View patient in darkest room possible.
Hold lamp 8-12 inches from patient’s face and rotate wrist to change angles.
Under a Wood lamp, epidermal hyperpigmentation is bright and accentuated. Deep dermal hyperpigmentation is not seen or is less pronounced.
Determine and document patient’s skin type (using the Fitzpatrick skin type classification) 1 and photoaging grouping (Tables 19-1 and 19-2), degree of actinic damage, sebaceous gland density, dyschromias, suspicious lesions, and scarring.
Point out any skin excess and gravitational changes that will not be corrected by chemical peels.
Standard preoperative photographs for surgical planning (see Chapter 3)
Presurgical arrangement and understanding about financial responsibilities for revisions
Analysis and operative planning based on patient’s desires, clinical examination, and photographs.
Tip:
The worse the patient looks under a Wood lamp, the more superficial the pigmentation.
Box 19-2% Peel Results for Different Dyschromias
Superficial Peel | Medium-Depth Peel |
Excellent Results | Excellent Results |
Ephelides | Ephelides |
Epidermal hyperpigmeritation | Epidermal melasma |
Epidermal melasma | Epidermal postinflammatory hyperpigmentation |
Lentigines simplex | |
Senile lentigines | |
Variable Results | Variable Results |
Lentigines simplex | Dermal and mixed melasma |
Mixed (epidermal and dermal) melasma | Dermal and mixed postinflammatory hyperpigmentation |
Mixed postinflammatory hyperpigmentation | Seborrheic keratoses |
Senile lentigines | |
Poor Results | Poor Results |
Dermal melasma | Nevi |
Dermal postinflammatory hyperpigmentation | Some exophytic seborrheic keratoses |
Junctional nevi | |
Seborrheic keratoses |
Nonfacial Peeling
Indications
Back
To remove sunburn freckles across the shoulders and upper back
To improve acne scars
To improve postinflammatory hyperpigmentation from acne
Chest
To improve hyperpigmented macules, usually lentigines or flat seborrheic keratoses and sunburn freckles
To improve acne scars, especially in areas of hypopigmented scars and hyperpigmented actinic damage
To improve postinflammatory hyperpigmentation from acne
To improve fine wrinkling (usually vertical lines over the sternum)
Hands and forearms
To improve hyperpigmented macules (age spots)
To improve superficial wrinkling
To improve rough texture
Some key points
It usually takes nonfacial areas 50%-100% longer to heal than the face. Patients need to be sure they have time to undergo this type of therapy before having it done.
Dermal peels on the arms, hands, neck, and chest are more prone to scarring or abnormal textural changes. It is safer to perform epidermal peels in these areas. Dermal hyperpigmentation and most types of scars on nonfacial areas should not be treated with chemical peeling, because they will not improve significantly.
Most nonfacial peels are done to improve fine wrinkling and blotchy discoloration (including age spots). One intraepidermal peel is usually not sufficient to give these patients their best results. Nonfacial peels are usually repeated several times to achieve the best response.
Most nonfacial peels are performed on large areas of skin (a larger surface area than the face). If a peeling agent with potential toxicity is used, there is a greater risk of developing a systemic reaction.
The larger the area treated and subsequently wounded, the more difficult it is for patients to care for it, and the greater the chance of a complication, particularly premature peeling or infections.
Informed Consent
Recommended items to be included in the informed consent:
No warranties, guarantees, or special contracts about the success and longevity of the procedure
Review of the healing process and how the patient will look and for how long
Possible need for additional surgeries/procedures
Complications, especially pigment changes (hyperpigmentation and hypopigmentation), scarring (including keloids, hypertrophic scarring), fever blisters (herpes simplex) activation, infection, milia, and “pink areas” (erythema)
Review (with the patient) the things chemical peels can and cannot do (Box 19-3).
Box 19-3% Things Chemical Peels Can and Cannot Do
Peel Preparation
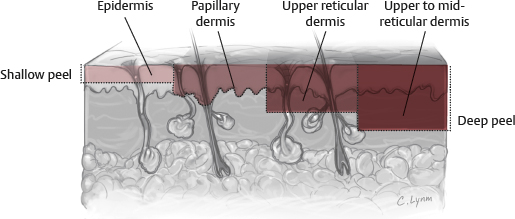
Chemical peels may be classified as:
Superficial (epidermal injury)
Medium-depth (superficial dermal injury to the papillary dermis)
Deep (mid-dermal injury to the reticular dermis).
Degree of injury is dependent on:
Chemical agent used
Concentration
Time of application before neutralization
Number of coats and the amount of peeling agent placed with each application (i.e., degree of wetness of the applicator)
Fig. 19-1 is a review of skin anatomy. The different chemical peel formulations commonly used are summarized in the section Common Chemical Peel Agents.
Common Chemical Peel Agents
Glycolic Acid
The product
Not light sensitive: Does not need to be stored in a dark bottle
Very stable (>2 years)
Deliquescent (absorbs moisture): Must be kept in a tightly capped bottle
Features
Most practitioners use 30%-70% glycolic acid and neutralize the skin with a bicarbonate solution or rinse with water at the onset of erythema.
Caution must be used, because uneven peeling and dermal wounding can occur.
White, scattered frosting indicates epidermal necrosis and dermal inflammation.
Moy et al 5 found a protocol of 10%-15% glycolic acid applied twice daily and 50%-70% glycolic peels given weekly for 4 weeks effective in the treatment of fine wrinkles and superficial lesions. Van Scott and Yu, 6 using a similar protocol for 10 months, reduced wrinkles in 21 of 27 patients.
Glycolic peels are less effective for solar keratoses and solar lentigos.
Piacquadio 7 concluded that retinoids, light TCA peels, and glycolic lotion represent a better consumer value than glycolic acid peels.
Tip:
Glycolic acid is an alpha-hydroxy acid (AHA) made from sugar cane. Other AHAs include lactic acid (from sour milk), malic acid (from apples), citric acid (various fruits) and tartaric (from grape wine).
Jessner Solution
Formulated by Dr. Max Jessner. The combination allows decreasing the concentration and toxicity of each ingredient.
The product
Contains resorcinol, salicylic acid, lactic acid, and ethanol
Retains strength for up to 2 years if container is opened for only 5 minutes per month
Light and air sensitive! May develop a salmon-colored tone on exposure to light and air—store in a dark amber bottle with a tight cap
Features
It creates a uniform-depth peel that results in an excellent exfoliation.
It is useful in treating hyperpigmentation by increasing epidermal turnover and yielding a decrease in the number of melanin-containing keratinocytes.
Complications are rare because of the limited penetration.
Use is limited to the face because of the potential for salicylate (tinnitus, headache, nausea) or resorcinol (methemoglobinemia and hypothyroidism with prolonged use) toxicity.
It is thought to break the intracellular bridges between keratinocytes and has the capacity to remove the epidermis.
Used alone, it causes superficial epidermal peel.
Depth is controlled by number of applications.
No neutralization is needed.
It can be combined with TCA for a medium peel.
Application first causes a faint erythema followed by a more pronounced erythema on second application. After further applications, a frost begins to form. Significant exfoliation is seen for 8-10 days when a frost is achieved; however, no weeping or crusting is seen, because it remains an intraepidermal peel.
Trichloroacetic Acid (TCA)
The product
Not light sensitive
Refrigeration not needed
Stable for at least 23 weeks in an opened container
20%-100% TCA stored in an unopened TCA-resistant clear plastic container for 2 years—TCA concentration within 3% of the labeled strength
Colorless and clear
Free of precipitate
Features
TCA is commonly used in 30%-35% concentration for medium-depth peeling penetrating into the upper reticular dermis.
The concentration, skin preparation, pretreatment skin type, and method of application contribute to the peel depth obtained.
An intraepidermal, epidermal, or papillary dermal peel can be successfully obtained with 20% TCA. Superficial papillary dermal necrosis was shown histologically in a porcine model at 24 hours using 20% TCA; however, no change in the number of fibroblasts or elastic fibers was detected at 28 weeks after the peel. 8
Dolezal 9 suggested four levels of superficial and intermediate TCA peels.
Level 0: Has no frost, and the skin looks slick and shiny, which represents removal of the stratum corneum.
Level 1: Has an irregular, light frost with some erythema; this is an intraepidermal peel that creates 2-4 days of light flaking.
Level 2: Has a pink-white frost, which suggests a full-thickness epidermal peel, and heals in about 5 days.
Level 3: Has a solid white frost and is thought to extend into the superficial retinacular dermis. Johnson et al 10 described an additional sign of “epidermal sliding” for a papillary dermal peel.
Croton Oil Peel
The product
Initially utilized by “lay peelers.” The formula was obtained by Tom Baker in the early 1960s. The original Baker Gordon formula utilized high concentrations of phenol and croton oil (50% phenol, 2.1%-2.4% croton oil). Although excellent results could be obtained, long-term hypopigmentation became a problem and croton oil peeling fell into disfavor.
Phenol-croton oil peeling regained popularity in the early 2000s due to the work of Hetter 11 – 14 and later Stone and colleagues. 15 – 16 Hetter refuted a number of the concepts espoused by Baker (phenol-croton oil peeling is an “all or none phenomenon,” and decreasing concentrations of phenol led to deeper injury). But most importantly both Hetter and Stone demonstrated by reducing the concentration of phenol and croton oil, complications could be significantly reduced while the results could be maintained.
Features
Stone suggested that the depth of peeling is dependent on the concentration of both the phenol and croton oil, whereas Hetter suggested that croton oil is the critical agent determining peel depth.
Ozturk et al 17 stated that a concentration of 33% phenol and 1.1% croton oil is associated with acceptable side effects in Fitzpatrick I and II skin types, especially in the perioral area.
Gatti et al 18 stated that treatment of the lower lids with phenol 22% and 1.1% croton oil is effective in treating hyperpigmentation and fine lines.
Standard concentration 88%
Used alone causes medium-depth peel
Causes keratin protein coagulation
Rapidly absorbed through skin, metabolized in the liver, excreted renally
Can lead to renal failure, hepatotoxicity, directly irritates myocardium causing arrhythmias
Requires cardiac monitoring and testing of kidney, liver, cardiac function
Hypopigmentation and scarring significantly minimized by reducing concentrations of phenol and croton oil.
Peel in subunits, allowing 15-20 minutes per site between units.
Phenol-Croton Oil and TCA Peels
Although traditionally TCA was considered a medium-depth peeling agent and phenol-croton oil a deep peeling agent, this has clearly been disproven by Hetter and Stone. Using modern peeling understanding, both agents can peel in subunits to superficial (epidermal), intermediate (papillary dermal), or deep (mid-reticular dermal) levels depending on:
Concentration of agents used
Number of applications
Wetness of the applicator
Most critical to the level of the peel is the degree and nature of the frost obtained.
Pink-white frost suggests injury to the papillary dermis; dense white frost suggests superficial reticular dermal injury, and gray-white suggests mid-reticular dermal injury.
Therefore, TCA and croton oil peels should not be thought of as intermediate or deep peeling agents only, but as agents that can peel to any depth desired. This significantly increases their respective versatility.
Salicylic Acid
The product
Made into a paste and spread over the skin using a tongue depressor
Formula: Salicylic acid powder USP, 50%; methyl salicylate, 16 drops; Aquaphor, 112 g
Features
The incidence of significant complications is low, and it is easy to use.
Deep penetration is difficult.
It is effective for the treatment of hyperpigmented age spots on the hands and arms. Patients will need to have their hands/arms wrapped in plastic wrap and gauze for 48 hours.
In concentrations of 3%-5% it is keratolytic and enhances topical penetration of other agents.
It has mild potency as a fungicide.
Symptoms of salicylate toxicity include ringing in the ears, muffled hearing, dizziness, and/or headache several hours after the peel. Increased water intake and removal of the bandage may improve mild salicylism.
Application of salicylic acid will cause mild stinging for 1-3 minutes followed by superficial anesthesia to light touch. After 5 minutes of air drying, the face should be washed with water.
Peeling starts around days 3-5 and continues until day 10.
Beta-Lipohydroxy Acid
The product
Eight-carbon fatty chain linked to a benzene ring (derivative of salicylic acid)
Available in formulations of 5% and 10%
Features
The safety profile is good with less skin irritation, compared with glycolic acid, and neutralization is not required.
It reduces melanosome clustering and epidermal pigmentation and is used for treatment of photoaged skin and acne.
It increases the skin’s resistance of UV-induced damage.
It has antibacterial and antifungal effects.
The corneosome-corneocyte interface is targeted to cleanly detach individual corneosomes, preventing desquamation in clumps and resulting in skin smoothness.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree