16. Condition-Specific Rhytidectomy: An Evidence-Based Paradigm Shift in Facial Rejuvenation
16.1 Introduction
Why the modifier “condition-specific” in the title of this chapter? As one delves into the pages that follow, the answer will become rather obvious. Not all faces are the same, and the same face is a different face at different times in an individual’s life. Skill sets vary from one surgeon to the other and at different stages in the surgeon’s career. So why should all facelifting operations be the same—even in the same surgeon’s hands? The fact is they should not be.
For a century, aesthetic surgeons have sought the “Holy Grail” in facelifting–us included. The fact that a surgeon is tempted during his or her career to change from the technique taught is proof that the “ideal” facelifting technique has yet to be discovered. Perhaps surgeons have been searching for the wrong thing. Rather than a specific technique, with length of incisions, depth and extent of dissection, vectors of tension, suspension materials used, and so forth, the “ideal” facelift is one arising from the enlightened selection—and performance—of a variety of techniques and materials, each being the “right” or “wrong” choice, depending on the conditions present in a given face at a specific time in that face’s evolution.
Why should it be a surprise to surgeons—and patients—that long-lasting, natural-appearing posttreatment faces are a rarity after “one-size-fits-all” rejuvenation techniques. The fact is that “one-size-fits-all” is the wrong size for faces at the extremes of the aging spectrum. Idealized outcomes, on the other hand, tend to follow an appreciation of widely variable factors: (1) an artistic eye capable of quantifying the naturally occurring conditions associated with aging; (2) an algorithmic mind-set that translates findings into a condition-specific treatment plan; (3) a skill set, instrumentation, and materials necessary to convert findings into outcomes; and (4) the wisdom to know when—and to what degree—intervention is advisable, if at all.
History is a trusted instructor. It is often called on to teach the same old lessons, one of which is that fads generally pass as rapidly as they appeared on the scene. As a rule, it takes 5 to 7 years of nonbiased observation to determine how well “new” techniques or modifications of time-tested ones, products, and devices measure up to those they were designed to replace.
In keeping with the “quick fix” mind-set of 21st century Western societies, rejuvenation medicine and surgery have been inundated with “change.” The appearance-enhancing industry has been flooded by a new breed of physicians and surgeons who bring with them a nonsurgical, minimally invasive ideology, calling for procedures, products, and devices that match their skill sets.
Through massive marketing campaigns—driven by manufacturers rather than physicians—not only are mind-sets of the medical professions being manipulated, but patients are being directed toward less invasive, shorter-lifespan alternatives to address their concerns. Aesthetic surgeons no longer lead the development of technology. Many are compensated by manufacturers of trendy products and devices to assist in their marketing. The result: a “less is more” ideology has brought Newton’s laws of motion into the aesthetic industry. Forces opposed to surgical correction have resulted in a paradigm shift toward lowered expectations and long-term mediocrity.
Aesthetic surgeons are partly to blame. When the public sees high-profile faces with the telltale signs of poorly conceived or poorly performed plastic surgery, every surgeon in the industry pays the price. Patients are driven toward nonsurgical solutions to their concerns, oftentimes resulting in disappointment.
As the art and science of facial rejuvenation enter the second decade of the 21st century, a “condition-specific” system, designed to provide natural-appearing, longer-lasting results could qualify as a “stitch-in-time” paradigm shift back to common sense. Nineteenth century French visionary Victor Hugo might describe the authors’ call for a return to reason “an idea whose time has come.”
The following pages elaborate on the rationale behind—and clinical application of—the senior author’s previously published classification system for facial rejuvenation and provide clinical evidence that—when thoughtfully applied—provides the right surgeon with the best opportunity to offer the right patient the right treatment plan at the right time in that patient’s life.
16.2 Brief History of Surgery to Rejuvenate the Face
The earliest attempts at surgical rejuvenation of the face were reported in Western literature in 1912. These early rhytidectomies consisted of simple preauricular elliptical skin excisions. 1 Since then, there have been numerous advances in surgical technique, 2 in the conceptualization of the pertinent anatomy as is applies to the study of aging, 3 and in the development of technical adjuncts. 4 , 5 , 6 High points in this evolution of understanding include the recognition of the importance of the superficial musculoaponeurotic system (SMAS), 7 , 8 , 9 , 10 , 11 the study of the supporting ligaments of the face, 12 and recognition of the interrelated anatomy of the lower eyelid and midface. 13 There are many others, too numerous to detail, that have furthered our attempts to improve the lives of patients though surgical rejuvenation. Facial aging is a complicated process that involves several marginally understood processes that include, at least, the following: a loss of the tone and elasticity of the skin, a relaxation of soft tissue support structures, atrophy and remodeling of the facial skeleton, and atrophy and redistribution of the associated fatty masses. What occurs at the cellular level that causes these deleterious changes is even less understood and probably largely unidentified. In view of this acknowledged biological complexity, it is easy to understand why the current literature is replete with a constellation of techniques and nomenclatures describing aging dynamics and solutions for rejuvenation. Most of these are based on the sound expert opinion of competent, credible clinicians. Some of these, however, are based on less confident foundations that fail to persist. Nomenclature is flawed because there is a lack of standardization of anatomical descriptions as well as of the naming of techniques. 14 Finally, consensus is lacking about the descriptions of aging, as well as how outcomes are judged. 15 The senior author has described a classification system directed at creating a more objective measurement of facial aging, as well as outcomes of treatment. 16 This classification system will aid the advancement of the study of facial aging and foster its entry into the realm of evidence-based medicine. In this chapter, many of the current philosophies of the senior author about how the patient seeking facial rejuvenation is approached will be related with implementation of the McCollough classification system.
16.3 The Effort to Understand, Communicate, and Quantify Facial Rejuvenation
The senior surgeon’s training in facelifting arose from a fellowship served under three different surgeons in different parts of the United States. None of his three mentors performed the operation in the same manner. Incisions differed. The extent of undermining, treatment of fat, suspension—or lack thereof—of deeper facial tissues, wound closure, postoperative management, and so forth, were as varied as the climates in the regions of the country where they lived and practiced. So what is a young surgeon to do? Which technique does he or she follow? All produced acceptable results and built large, successful practices. The senior surgeon chose to perform the technique learned from each of his mentors for 20 consecutive facelifts and compare the results. The answer he arrived at set the stage for the development of a condition-specific approach that came four decades later. Portions of each of the techniques learned were incorporated into a condition-specific ideology. Approximately 6,000 facelifts later, the senior author came to a long-overdue realization. No universally accepted or implemented classification system for the regionalization and quantifiable analysis of facial aging or facial rejuvenation surgery has been described in the aesthetic surgery literature.
Applying the age-old adage “Necessity is the mother of invention,” he formalized a classification system to standardize the language of facial aging rejuvenation. With the establishment of such a system, it becomes possible to facilitate facial analysis, to have clearer communication between practitioners, and to study objectively the natural evolution of facial aging. Currently, surgeons make treatment decisions routinely as part of a general internalized subjective system.
The senior author stresses that the classification system that can be applied to facial rejuvenation is still evolving. One goal is to create one as comprehensive as the tumor, node, metastasis (TNM) system (Union for International Cancer Control and American Joint Committee on Cancer) used in the management of cancer. Another goal is to have the classification system be as readily used as the House-Brackmann grading of facial paralysis 17 or the Manson classification of nasoethmoid orbital fractures. 18 Through the adoption of a facial rejuvenation classification system and the standardization of facial analysis, it becomes possible to aid decision making in the selection of procedures for the surgical correction of a particular patient’s anatomy. For instance, after continued use of the classification system, it is possible to predict more accurately or select which combination of procedures is determined to be “ideal” for each patient. For example, some patients may be a candidate for only a cheek and neck lift. Others at the same chronological age may require a cheek, temporal, or forehead procedure. Still others might benefit from various combinations of these.
This predictive or guidance capacity becomes more reliable with increasing recruitment of patients for analysis and classification. The classification system allows for more precise communication methods within the aesthetic medicine and surgery community. An evidence-based perspective is possible. Although this classification system continues to evolve, it currently involves the standardized grading of aging changes of specific areas of the face.
For the purposes of this chapter, the senior author’s classification system will be used as part of the preoperative analysis of candidates for rhytidectomy. In an expanded form of the classification system, however, there are components allowing it to be used to grade changes of the neck, periorbital, perioral, and forehead areas, as well as eyelids and skin.
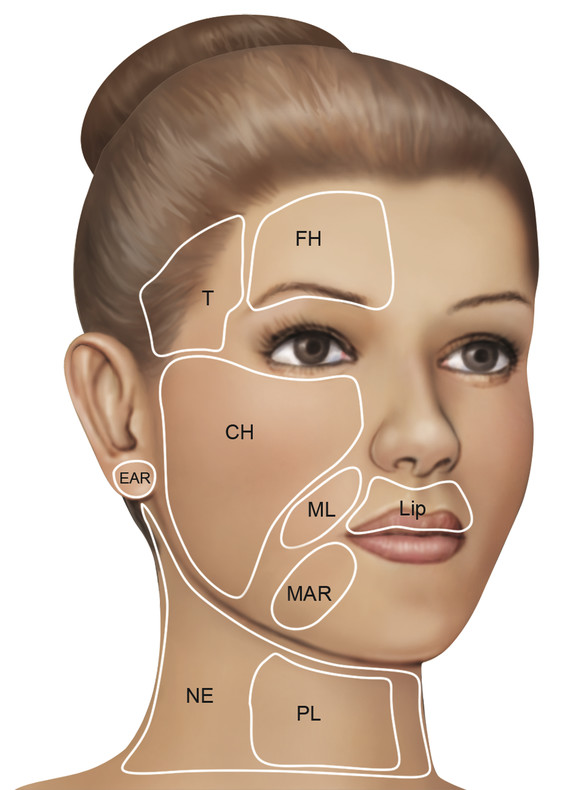
Fig. 16.1 depicts the pretreatment evaluation form of the expanded classification system, which is comprehensive for application in the analysis of patients with significant aging of their neck, periorbital, perioral, and forehead areas. The document encompasses all areas of the face commonly considered in the context of facial rejuvenation. It differs from the version initially reported. 19 Updates and modifications will evolve as more data are collected. In its most comprehensive form, the system is easily used in the research setting to allow the acquisition of large amounts of data. For the working clinician, the system may be modified and adapted to the practice.
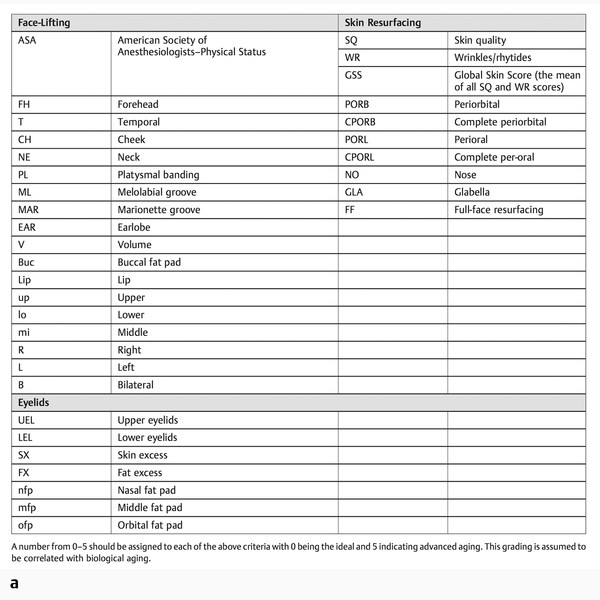
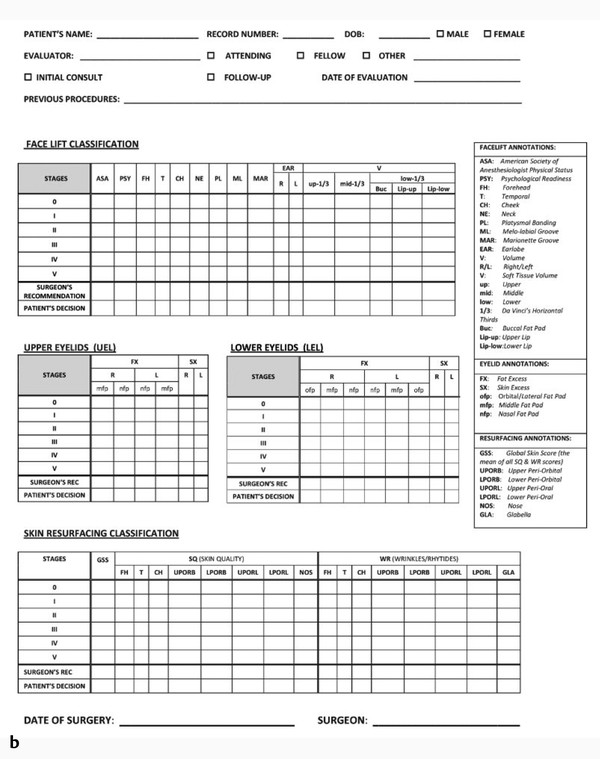
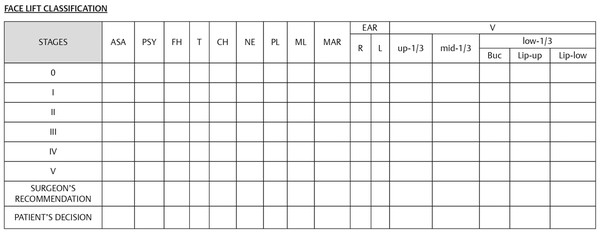
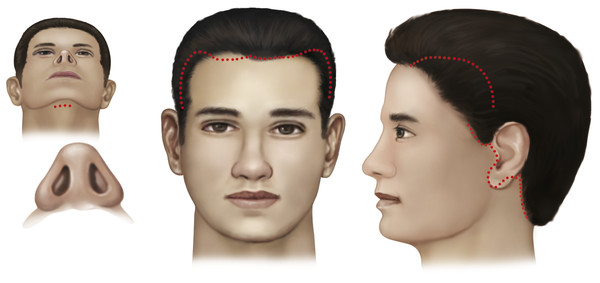
Fig. 16.2 depicts the components of the classification system to be used in this chapter to illustrate the application in a more simplified fashion. Fig. 16.3 depicts the facial areas examined in the classification of facial aging.
16.3.1 The Consultation
The initial consultation may be the most important part of the surgeon’s contact with the patient. Its sole purpose should be to establish mutual respect and a trusting relationship between the surgeon and the patient. In many ways, it is in this interaction that the surgeon sets the stage for every interaction that follows. Of course, the patient’s initial welcome into the office serves a similar first-impression and setting-the-stage role. Thus, every staff member plays an important role in the patient’s experience. For purposes of this publication, the role of the surgeon is highlighted.
The consultation is a mutually beneficial encounter. It allows the surgeon to evaluate the prospective patient. It also allows the patient to evaluate the surgeon. Today, patients are smart. They have access to a plethora of information. It is easy for them to size up a surgeon and—rather quickly—determine whether the surgeon is attempting to “sell” them an operation or product. The latter assessment will end with the patient deciding to go elsewhere or result in a relationship where there is little resilience. This will prove fragile should the patient have a less than optimal result after surgery. The central interpersonal and psychological aspects of the consultation are what these authors would like to emphasize as the groundwork for a long and happy relationship.
The setting in which the patient meets the surgeon for this first time should be warm, inviting, and professional (Fig. 16.4). The surgeon must never appear hurried or distracted and must be able to devote 100% of his or her attention to the patient.

The duration of the consultation is of less importance than the patient’s perception of the quality of the interaction. In the initial interview with the patient, the surgeon should ascertain the patient’s mental and physical health, as well as motivations for surgery. Motivations will have to be based in reality with realistic goals and expectations. Otherwise, the surgery will likely be deemed unsuccessful. If the patient’s motivations are founded on an emotional or reactionary basis, he or she is probably a poor candidate, and the experience is likely to be unhappy for both the patient and the surgeon.
Essential aspects of the history should be obtained, either by the surgeon or by an assistant. An appropriate history includes information about the patient’s general health, prior experiences with surgery and anesthesia, and a complete list of medications and allergies. Several general health issues would jeopardize a patient’s candidacy for surgery, including—but not limited to—life-threatening heart conditions and use of anticoagulants or platelet inhibitors. It is crucial that clotting inhibitors be discontinued before facelifting surgery that involves extensive undermining of the skin and deeper structures of the face and neck. If the preoperative workup reveals consequential risk factors, consultation with the appropriate medical colleague(s) should be considered.
The history of previous surgeries may give clues as to how the patient will tolerate necessary anesthesia for rhytidectomy. It is, of course, important to note whether the patient has had previous facial surgery, where the incisions were placed, whether or not the procedure was considered successful, and whether any complications ensued during or after the surgery.
Although the initial screening of patients for rejuvenation surgery may be performed via electronic media, technology does not supplant a surgeon’s firsthand examination of the patient, especially before the administration of medications that could alter the patient’s mental capacities.
The presurgical examination should not only be visual in nature, but should also involve palpation of underlying structures and the assessment of skin quality, laxity, and elasticity.
Part of the examination is carried out with the patient in front of a mirror. Most surgeons have a systematic routine in evaluating the patient’s skin, face, and neck. The senior author begins at the top of the face, assessing the brow, the eyelids, the cheeks, the jaw area, and finally the neck. By touching the patient and gently manipulating the structures, the surgeon gives the patient both visual and tactile feedback.
A three-way mirror is a valuable tool in the presurgical education of a patient. It allows the surgeon to demonstrate his or her findings to the patient, from a variety of angles—especially any asymmetry in facial features. The potential improvement of laxity is demonstrated by gently repositioning the skin and subcutaneous tissues to a more youthful position. In this way, the patient can see how sags and bulges are to be addressed. With a gentle lifting on the skin in the appropriate vectors, the patient can visualize the potential correction of his or her neck, jowl area, cheek, and jawline. The amount of skin to be removed is demonstrated. Using a nontraumatic pointing device, the placement of incisions is demonstrated on the patient’s face and neck. Similarly, the amount of excess skin to be eliminated by blepharoplasty, if contemplated, is demonstrated in the mirror.
Finally, any blemishes or photodamage of the skin is demonstrated, followed by a description of alternative resurfacing procedures. Note that although the focus of this chapter is rhytidectomy, many candidates for the procedure will benefit from several simultaneously performed procedures, including blepharoplasty, rhinoplasty, volume augmentation of the face and lips, and skin resurfacing. “Informed consent” involves addressing the interrelationship of these factors in rejuvenating any aging face and alternative methods of treatment.
A crucial part of the consultation involves discussion of a consent form and demonstration of the proposed surgical plan on the appropriate drawing(s) (Fig. 16.5). Incisions, postsurgical scars, vectors of tissue movement, and areas to be resurfaced are noted. The patient is given ample time to–and encouraged to–ask questions about anything discussed or proposed. Questions are answered in a forthright manner, including a discussion of the procedures to be performed, alternative methods of treatment, limitations of each procedure, risks, imponderables of treatment, and the vagaries of healing.
Patients are provided access to printed and electronic materials about the procedures and encouraged to call with any questions that might arise after they leave the office. Subsequent consultations may be advisable in some cases, particularly if the patient is unsure as to the surgical plan or postoperative management of the treatment. Each patient is invited to meet with a surgical coordinator and scheduler after the consultation. The cost of surgery, anesthesia, operating room, postoperative care medications, and materials and follow-up are discussed. Revealing these costs before surgery is a good way to maintain a congenial doctor–patient relationship for years to come.
16.3.2 Application of the McCollough Classification System in the Selection of Technique
Fig. 16.6, Fig. 16.7, and Table 16.1 illustrate the application of the McCollough classification system. This patient would be coded preoperatively as V-3, FH-3, CH-4, ML-4, MAR-3, NE-3, and PL-2. Although we are still collecting data on the application of the classification system, this patient would be considered to have a stage III aging classification and thus was considered to benefit best from a forehead, temporal, cheek, and neck lift with suction-assisted lipectomy of cheeks and neck. (Note: The patient, in addition, underwent upper and lower blepharoplasty, but for simplicity of illustration in this publication, it was not coded.) As more data are collected with this system, it is planned to develop recommendations based on analysis through classification to optimal procedure. The reader is directed to the cited references for an in-depth description of the classification system.


Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree