13 Circumferential Dermolipectomy of the Lower Trunk: Lower Body Fit
Abstract
Due to the high incidence of obesity in the United States and Mexico, there has been a constant rise in the number of postbar-iatric surgery patients who achieve massive weigh loss (MWL). This has caused, by consequence, an incremental increase in patients undergoing plastic surgery to correct the silhouette alterations that result after MWL. The plastic surgeon needs to select and adjust current reconstructive and aesthetic techniques to accomplish the functional and cosmetic goals of the postbariatric patient. This wide range in surgical tools is used for one objective: to restore form and and function by fitting the dermo-adipose tissues to a proper muscle-aponeurotic structure of the lower trunk. The techniques and methods used need to be matched to each patient’s unique skin and fat distribution. Meticulous preoperative preparation and surgery design are essential to obtain satisfactory results.
Introduction
The World Health Organization has declared a “global obesity epidemic,” which is considered by many one of the most pressing issues in public health.1 This problem is especially prominent in the United States and Mexico, where the number of patients with extreme or morbid obesity (body mass index [BMI] of at least 40 kilograms per height in meters squared [kg/m2]) who undergo bariatric surgery is on the rise.2,3 There are various bariatric procedures that are of a restrictive or malabsorptive nature, such as the gastric band, vertical gastroplasty, and gastric bypass.3–5 Because of bariatric surgery and better postoperative medical and nutritional management, it has been possible for this group of patients to achieve massive weight loss (MWL) and maintain it in the long term.6
These patients present a great variety of silhouette deformities due to the excessive stretching and laxity acquired, as has been noted in patients with a BMI >35 kg/m2.6–8 Progressive and relatively rapid weight loss brings, as a consequence, loss of support of the integumentary system that was previously provided by the excessive fat content. The collagen and elastic fibers, not only in the dermis but also in the deep fascias, are permanently disrupted in the overstretching period.9 Therefore, these patients acquire a “molten candle” look, with large skin and fat folds that hang from the anterior and posterior midlines in a pattern and quantity that are difficult to predict prior to the bariatric surgery.10 The MWL causes not only aesthetic and silhouette alterations, but also psychological and functional disorders.11–13 This is compounded by the fact that most patients, and sometimes their significant others, were not psychologically prepared for the magnitude of flaccidity that would be a consequence of the massive weight loss.10,13 As plastic surgeons, we must remember that our patients submitted themselves to bariatric procedures not only for the overall health improvement but also to improve their self-esteem and self-image, which conveys both physical benefits and psychological relief.11,13
Relevant Anatomy
The abdominal wall is composed of several layers: the epidermis, dermis, subcutaneous fat, superficial fascial system (SFS), and aponeurosis, as well as the muscle groups composed in their medial aspect by the anterior abdominal rectus muscles and on the lateral aspect and flanks by the major oblique, minor oblique, and transverse muscles.
Huger14 described three vascular zones of the abdominal wall, demarcated by the multiple penetrating musculocutaneous and septocutaneous vascular pedicles originating from the wide superficial regional muscles. Zone 1 is delimited in the mesogastrium by the deep epigastric vascular arcade. Zone 2 is located in the hypogastrium and supplied by the external iliac artery through the circumflex vessels. Zone 3 consists of the flanks and hypochondrium zones with blood supply from the costal, subcostal, and lumbar arteries.15 Extensive dissection in a surgical subfasciocutaneous plane is detrimental to the blood supply in this region.16
History
The history of body contouring dates to the first cases publicized by Kelly in the late 1800s, who tried to correct the excess of body skin and fat by a horizontal dermolipectomy that included the umbilicus. This procedure was developed early in surgical history, considering that the first painless tooth extraction made possible by anesthetics occurred in 1845. Over the ensuing century, evolution in the abdominoplasty technique included fleur-de-lis excision patterns; preservation of the umbilicus, lower abdominal, and “bikini-line” incision placement; and abdominal wall aponeurotic plication and fascial tightening.17 Lockwood18 contributed to the great progress in body-contouring techniques by developing the concept of deep closure of the superficial fascial system to minimize tension and migration of the scar line, thereby improving scar cosmetics and location. He also determined that abdominal flaccidity was mainly due to the maximal laxity of tissue in the lateral body contour and hypogastrium, thus developing the high lateral tension abdominoplasty.
Aesthetic Considerations
The reason to operate on postbariatric patients is to improve function as well as aesthetics. Therefore, our objectives are not only to remove the excess skin, but also to bring the silhouette to a more acceptable form, to make the result long-lasting, and to pay special attention to scar location and quality. Although postbariatric patients present with varying degrees of dysmorphia, all wish to alleviate the psychological and physical discomfort caused by their MWL. Therefore, we are obligated to develop and execute procedures designed to maximize aesthetic results.
The concept of beauty changes over time, and we have seen a tendency toward slimmer figures, mainly in women, since the 1980s. The arrival of new aesthetic surgery procedures such as liposuction in the 1980s has given us novel tools to accomplish our goals.19 It is unlikely that patients will want a wider hip appearance anytime in the near future and at least for another generation. The current ideal female aesthetic model tends to be a more athletic and slimmer image, somewhat like an adolescent.20 The high-cut bikini was originally designed to give a longer appearance to the leg, but it enhances the hip. Current trends place emphasis on low-cut clothes and underwear, as they tend to reduce the apparent width of the hips. Because the waist-to-hip ratio is an important factor that determines attractiveness in women, strategies must be changed to accomplish beauty in this aesthetic unit. Liposuction and the “lower body fit” technique described here are successfully employed, in our hands, to make the leg appear slimmer and longer, the hip narrower, and the waist even narrower, hence maintaining an ideal waist-to-hip ratio of 0.7.21 Also, in the buttock area there is a fashion trend for lower-cut pants. Patients often complain that when bending forward their scars become visible. Thus, the traditional high-cut bikini lines have become outdated and have been replaced by a low-cut alternative. This is why we choose to leave our scar lines at the hip level.
Lower Body Fit
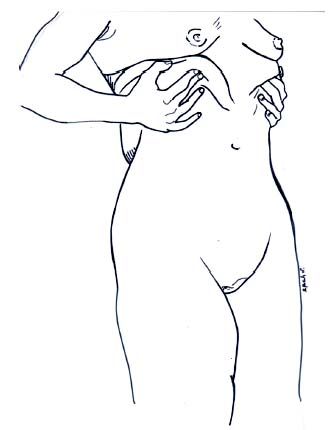
Many different terms have been used to describe the various surgical procedures executed to tighten the lower body: panniculectomy, lipectomy, dermolipectomy, circumferential abdominoplasty, belt lipectomy, high lateral tension abdominoplasty, lower body lift, among others. They all describe one or various procedures whose goal is improvement in the contour of the lower trunk in postbariatric patients. Our own term, lower body fit, encompasses all these ideas, and we think it is more accurate in describing the objective of our efforts, which is to make the skin and subjacent tissues “fit” the body of our patient, thereby restoring its natural contour. This is not limited to lifting ( Fig. 13.1 ), but includes tightening, liposuction, de-epithelialized flap augmentation, silicone implants, lipoinjection, and dermo-lipoaugmentation. A more explicit explanation of the lower body fit is low circumferential high-tension dermolipectomy of the lower trunk.
The approach used by our surgical group is to consider the trunk, thigh, and buttock areas as a whole, with tension exerted across all three regions, using the superficial fascial system for wound closure and fixation.18 One of the main objectives of our technique is positioning the scar lines in places where they can be hidden without the necessity for large underwear. We also avoid positioning scar lines in certain regions, such as across the gluteus; rather, we design our surgery to respect an “almond-shaped” contour, leaving the scars at its frontiers.
Lower Body Fit Objectives
There are differences between the anterior and posterior trunk; among them are the blood supply, direction of undermining, and vector of tightening. Historically, it was considered that the anterior trunk’s main aesthetic problem is localized in the lower abdomen, mainly because of the genetic distribution of fat deposits in that area and lack of attachment of the superficial fascial system to the midline.18 We must emphasize that the upper abdomen cannot be overlooked, because it also shares with the lower abdomen two main aesthetic problems: skin-fat excess and muscular diastasis. Treatment of both problems provides a more structurally sound abdominal wall, thus improving functionality and appearance.19
Liposuction of any flap has long been controversial. In the abdominal area, liposuction increases the risk of compromising vascular perfusion, with increased potential of skin or fat necrosis, and presents the risk of thrombotic or fat embolism.22 The literature, however, demonstrates the resiliency of the abdominal flap. Properly done, liposuction and/or direct excision of the deep fat compartment can be incorporated into the approach.23 We execute only limited liposuction by fluid infiltration: an average of 1 L saline solution with epinephrine distributed on the four quadrants of the abdomen (no lidocaine is used) to help dissection and hemostasis, followed by the same amount of lipoaspiration (1:1). The objective is to tunnel and liberate the flap. We reserve more aggressive liposuction for a second-stage procedure performed at least 3 months later.
Along the posterior trunk, our priorities change because we must resolve the problems affecting both the lower back and the buttock area. As discussed previously, we cannot undermine or liposuction much of the lower back, first, because of the limited vascular supply, and, second, because these tissues are not very mobile. Instead, we must lift the gluteal skin as a fasciocutaneous flap and anchor it to the lower back.
Another region to take into account is the flank area, which is responsible in great part for the contour deformities observed in postbariatric patients. The fitting of the lateral region was once ignored, but thanks to a deeper understanding of the trunk and thigh aesthetic unit, its relevance has been noted. Proper application of the high lateral tension abdominoplasty principles leads to improvement in the contour alterations of the flanks and thighs that we frequently encounter.
Pitfalls
We observed that many of the clinical cases presented in the literature show the scar line outside the bikini area, located above the gluteal limits, and also raise the hair-bearing area of the pubis. We also have noted significant scar migration and widening and/or pigmentation. Sometimes, the resection goes across the intergluteal crease in a perpendicular manner in a very low position; consequently, the scar trespasses the gluteal aesthetic unit.


Rather than being the antagonistic tension between superior and inferior flaps that causes ischemia or dehiscence, the true culprit is excessive local wound tension and diminished blood supply. The extent of skin resection, the patient’s position, and the patient’s movement contribute to tension exerted across the wounds. Skin resection can be planned in the preoperative stage by careful surgery design and precise measurement. In the early postoperative period, the patient rests in a flexed supine posture; we arrange the patient during surgery flexed in a similar manner but in a prone orientation during posterior resection. This is then inverted to a semi-Fowler position during anterior excision. Another determinant in the early postoperative period is the frequent repositioning of resting posture, alternating lateral and dorsal decubitus, and thus preventing posterior flap ischemia by compression. We have seen complications arise because of the patient’s refusal to mobilize during the postoperative period due to fear of causing an adverse event. Ironically, this complication is in actuality due to impaired blood flow as a consequence of continued pressure from im-mobility ( Fig. 13.2 ). Starting at the second day after surgery, we begin patient mobilization out of bed.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








