10 Circumferential Abdominoplasty

Abstract
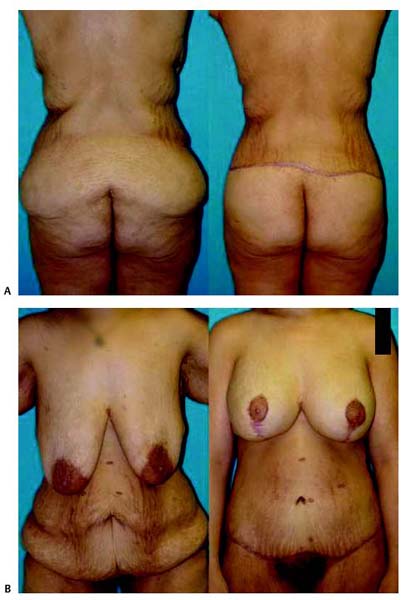
Body contouring after massive weight loss is an expanding and evolving field in plastic surgery. An increase in the popularity of gastric bypass and banding procedures has led to a population of patients with unique anatomic and physiologic deformities that can cause cosmetic as well as functional debility. Traditional abdominoplasty techniques are not well suited to this patient population. Circumferential or near-circumferential abdominoplasty, also termed a lower body lift, is more effective in providing an improved mid-body contour and abdominal wall tightening. The approach that we have utilized involves a circumferential or near-circumferential incision, vertical and/or horizontal abdominal wall plication, minimal back undermining, suspension of the superficial fascial system, and a sterile method of rotating the patient on the operating room table. The procedure has demonstrated a low complication rate, shortened operative time, and high level of patient satisfaction.
Introduction
In the United States, 20% of the population is obese, and 5% is morbidly obese, defined as a body mass index (BMI) of 40 kilograms per height in meters squared (kg/m2) or higher, or more than 100 pounds over the ideal body weight.1 Surgery for the treatment of the morbidly obese patient is today being performed much more frequently than in the past. This is due to the fact that endoscopic surgery has made the procedure much safer. Thousands of these procedures are being done in the United States each year. As a result of this surgery, patients can lose between 100 and 300 lb, become normotensive, generally bring their diabetes under control, and possibly decrease their risk exposure to pancreatic cancer.2 With the massive weight loss, however, patients experience severe sagging of the body’s tissues that creates significant deformities that are often as concerning to patients as was their preoperative obesity. The anatomy and physiology of these patients’ deformities are unlike that of their slightly overweight counterparts, in part due to the retention of the increased circulation that developed in response to the weight gain, the inelasticity of the skin envelope, and the volume redistribution of the underlying soft tissue structure. Body contouring after weight loss is a burgeoning field, with a 77% increase in these surgeries over the past 5 years, with even greater growth anticipated.
The mid-body, including the abdominal area, is often of the greatest concern to weight-loss patients. In patients who do not desire facial rejuvenation, mid-body contouring is usually the first stage in the body-sculpting continuum. Deformities of the mid-body after massive weight loss present functional as well as aesthetic concerns. Redundant skin can extend along the abdomen, hips, and back, often over the thighs, and to the knees, creating problems with hygiene and clothing. Skin breakdown and intertrigo recalcitrant to medical treatments, such as antifungal creams, are common. Buttock ptosis can conceal the gluteal fold.
Indications
Our experience has demonstrated that traditional abdominoplasty techniques are inadequate to address the unique anatomic problems present in this population of patients. Traditional abdominoplasty, as popularized by Pitanguy 50 years ago, does not address the excess and ptotic lateral thigh, hip, and buttock skin, which require elevation at the time of mid-body contouring. Circumferential abdominoplasty was initially described for obese patients by Gonzalez-Ulloa3 and Hunstad,4 but has been adapted in the last decade to the massive weight loss patient.5–9 These deformities almost always require circumferential abdominoplasty, which also has been referred to as belt lipectomy or mid-body lift, or near-circumferential abdominoplasty to the posterior axillary line, which is more appropriate in patients with little to no buttock ptosis. As discussed in other chapters in this textbook, the bariatric patient also demonstrates a series of back rolls that are amenable to surgical correction. The lower back roll and hip roll can be addressed as part of the mid-body contouring procedure. In addition, the buttocks and lateral thighs can cohesively be melded into the abdominoplasty procedure. Furthermore, the surgical approach must address the abdominal wall, including the rectus and oblique muscles and the umbilicus, as these patients frequently have concomitant deformities of these structures, including ventral hernias, incisional hernias, umbilical hernias, severe rectus diastasis, and horizontal as well as vertical laxity of the abdominal wall.
Patient Selection
In the series that we published in 2006,9 all patients had a prebariatric BMI in excess of 40 kg/m2, with postbariatric surgery weight loss ranging from 100 to 300 lb. Mid-body contouring surgery is reserved until the patient’s weight is stable for a period of at least 3 to 6 months, not varying more than 10 lb in this period. This typically occurs 1 to 2 years after weight-loss surgery. As discussed in detail in other chapters, a comprehensive preoperative medical evaluation is conducted in tandem with the primary care physician, as nutritional, metabolic, and electrolyte abnormalities may be uncovered during this time. This work-up is crucial, as mid-body contouring is frequently the first operation in the body-sculpting staging for these patients and subjects them to significant anesthesia time, fluid shifts, and blood loss.
Surgical Technique and Method
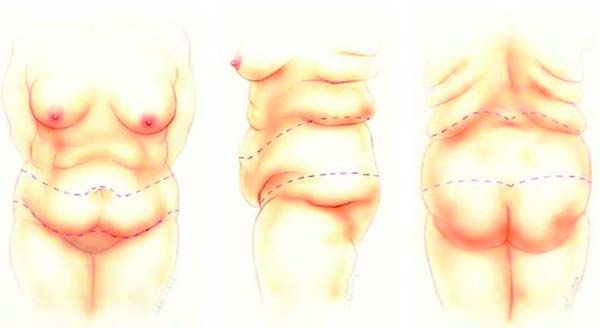
Patients are marked in the standing position. Patients with a heavy pendulous pannus are instructed to support the pannus with their hands. A wide-open W-shaped lower marking is made with a marking pen, extending laterally and inferiorly to a point just above the inguinal crease. The mons incision is marked 2 to 3 cm inferior to the pubic hairline to effect a lift to this area. From the inferior point of the W, a line is drawn superiorly and laterally aiming at the midpoint of the hip fold. The planned superior incision is marked 2 to 3 cm superior to the umbilicus in a W-shaped pattern, estimating the excess tissue by palpation. It is expected that during the flap redraping, after dissection and abdominal wall plication, the superior marking may be adjusted to provide minimal tension on the closure. Along the back, the superior marking is made at the apex of the lower thoracic back roll,10 directed slightly inferior toward the midline to decrease tension on the midline closure. The posterior incision is drawn, continuing from the anterior marking, extending toward the midline to a level just cephalad to the buttock crease ( Fig. 10.1 ). In summary, the lower thoracic and hip roll excesses are the key to the extent of the resection both posteriorly and anteriorly.
The patient is prepped with sterile technique in the standing position in the operating room, from the calves to the neck. The patient is placed onto two sterile cloth sheets on the operating room table, with the operating room staff assisting patient placement by rotating the legs onto the table after placing sterile stockinette dressings to the level of the knees. This position is completed prior to induction of anesthesia. After induction, a Foley catheter is placed and an intravenous dose of antibiotics given. Sequential compression devices are placed on the arms or under the stockinettes with an opening left near the foot to allow for passage of the connecting tubes.
The anterior abdomen is addressed first with the patient in the supine position. The inferior incision is made from medial to lateral as far posteriorly as possible. Dissection of the abdominal flap is performed just superficial to the abdominal musculature to the level of the umbilicus. Single hooks are placed into the umbilical skin opening, which is then incised with a 15-blade scalpel. Metzenbaum or facelift scissors are used to dissect the umbilical stalk to the level of the muscle fascia. The flap is divided along the midline with a 10-blade and cautery to the level of the umbilicus to assist in the dissection. Dissection of the flap is then completed to the level of the costal margins laterally and xiphoid process medially. The upper incision is then completed with scalpel incision of the previously marked line. The flaps are raised at the level of the fascia and are retracted laterally first on the surgeon’s side and then toward the opposite side. With strong traction on these flaps, further dissection at the level of the fascia is simplified. Additionally, the larger vessels going into the flaps are visualized and interrupted. With traction on the flaps now medially, the balance of the skin incision is made superiorly and inferiorly to the posterior axillary line. This is easily visualized by traction on the flaps to the opposite side, allowing for turning of the patient to expose the posterior axillary line.
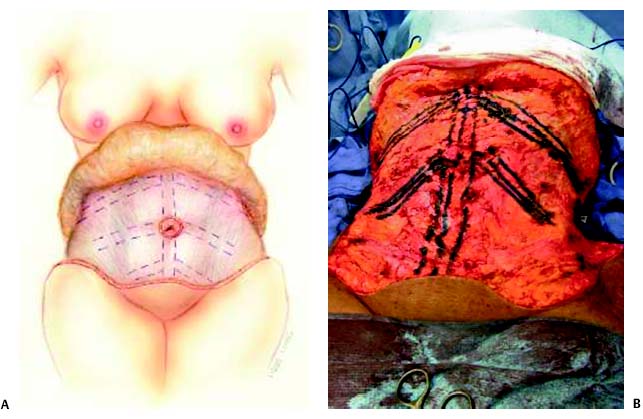
Abdominal wall anatomy is next addressed. Preexisting abdominal wall hernias are often addressed at this time through primary repair, mesh or biologic implant placement, or component separation techniques. The medial borders of the rectus abdominis muscles are marked for planned plication. Plication is then performed using buried figure-of-eight Nurolon or Prolene suture from the xiphoid to the umbilicus and from the umbilicus to the pubis. To diminish vertical laxity and to shape the abdominal contour, a series of oblique plications of the abdominal wall can be performed. A superior plication is performed at a level 2 to 3 cm below the costal margins, obliquely to the mid-flank area. A second plication is placed from the umbilicus obliquely to the iliac crest and/or along the lower abdomen. A third, lower plication may rarely be needed. We refer to these as “military” plications, as they resemble private, corporal, and sergeant stripes ( Fig. 10.2 ).
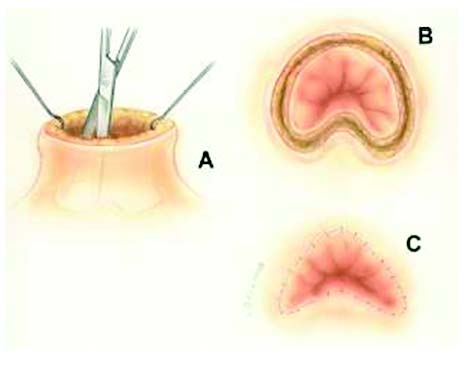
The upper flap is now inverted so that the surgeons are looking at the deep fatty layer. The fat deep to Scarpa’s fascia is now excised meticulously with scissors. This is reasonably atraumatic compared with liposuction. The mons can similarly be contoured. Liposuction of any portion of the superior flap, flanks, or hips is found to be unnecessary and is avoided to prevent any further sacrifice of the blood supply. A new umbilical opening is made through the flap at the level of the iliac crests and along the midline using a variety of incisional patterns, depending on the appearance of the umbilicus. The most common incisions are either a simple vertical ellipse or an inverted V-shaped incision with the lower portion of the umbilicus split at the 6 o’clock position and then inset ( Fig. 10.3 ). Two Jackson-Pratt drains are placed deep to the abdominal flap and brought out through the mons flaps and secured; two Penrose drains are placed under the flap and brought out at the posterior axillary line. The transverse incision is closed in three layers, using 2–0 silk in the superficial fascia system (Scarpa’s fascia), 3–0 Monocryl deep dermal sutures, and 4–0 Monocryl subcuticular sutures. Dermal glue and Steri-Strips complete the closure. Sterile dressings are placed to cover the anterior incision at this point and secured in place using large sterile Tegaderm dressings (3M, St. Paul, MN).
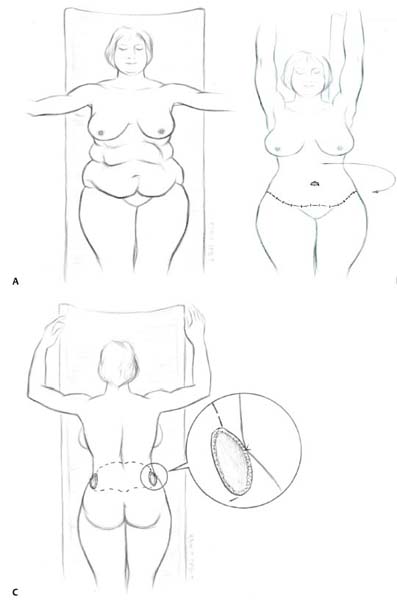
Rotation of the patient into the prone position can cohesively and safely be accomplished with the assistance of the anesthesiologist, surgical assistant, and two operating room attendants without resorting to nonsterile technique. The sterile sheets to the right of the patient are grasped and pulled laterally, bringing the patient past the edge of the operating room table. The nonsterile arms are positioned above the head, each being held by an attendant. Extreme vigilance to the endotracheal tube is paid by the anesthesiologist. The surgeon raises the sheets, allowing for chest bolsters to be positioned beneath the sterile sheets, and the patient is then rotated 180 degrees. Sterility has been maintained during the process, which takes no more than 5 to 10 minutes ( Fig. 10.4 ).
As the anterior resection has been extended far laterally, the posterior portion of the resection can be performed expeditiously. The preoperative markings are reinforced with a marking pen and then incised. The incisions are carried down superiorly and inferiorly to the level of the deep back fascia. The flap is raised sharply, and perforators are cauterized. Minimal to no undermining of the superior and inferior back flaps is performed. Closure of the back proceeds in the same manner as for the anterior portion. Two Jackson-Pratt drains are placed and brought out separately through the lateral incisions. The back is then dressed with sterile dressings. The patient’s recovery bed is brought into the room, and the patient is rotated back into the supine position onto the bed. The recovery room bed is flexed. The anterior dressings are then reinforced, and an abdominal binder is placed. Extubation is performed with the patient on the recovery room bed. Using these techniques, we have been able to reduce the length of surgery to between 3 and 3.5 hours on average.
Patients are mobilized the night of surgery or early on postoperative day 1. Antibiotics are given intravenously before surgery and during the hospital stay, and continued orally until the drains are removed. All patients receive prophylactic low molecular weight heparin subcutaneously at 4 hours after surgery and until discharge from the hospital. Penrose drains are removed at 24 hours, and suction drains are removed when drainage from each drain is <30 mL/day. Patients are typically discharged on postoperative day 1 or 2. After our initial published series of 75 patients, pain control was accomplished primarily with pulsed electromagnetic field therapy (Ivivi, Northvale, NJ). This allowed for a comfortable discharge on the first postoperative day, thus shortening the patients’ hospital stay by 1 to 2 days.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








