1 Fundamentals and Principles
1.1 Etiology of Vulvovaginal Defects
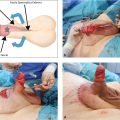
There are many different causes of vulvar defects. Tumors of the vulva are the main cause. They represent about 5% of all malignant disorders of the female genital system and about 1% of all malignancies in women. Vulvar carcinomas are observed increasingly often after the fifth or sixth decade of life (▶Fig. 1.1). The modified radical vulvectomy as described by Taussig (1940) 12 and Way (1948) 13 involves mobilization of a large composite flap of skin and fatty tissue and en bloc resection of the regional lymph tissue together with the primary tumor and adjacent vulvar tissue. Yet, the radical vulvectomy with separate bilateral inguinal lymphadenectomy is also an established surgical procedure.

Advances in surgical treatment and perioperative patient care now allow patients with extensive carcinoma of the vulva that has spread to adjacent organs, such as the urethra, urinary bladder, and/or rectum, to undergo extensive tumor surgery, provided that these patients are in good general health and remote metastases have been excluded. This surgery generally involves anterior, posterior, or total exenteration combined with a radical vulvectomy and an inguinofemoral lymphadenectomy, which leaves large defects (▶Fig. 1.2).
In recent decades, the prevalence of vulvar intraepithelial neoplasia has increased significantly, especially in young women. In diffuse disease, what is known as a skinning vulvectomy may be considered for treatment. Rutledge and Sinclair first described the surgical procedure in 1968, 9 which creates a defect only at the level of the dermis (▶Fig. 1.3). The operation can be regarded as a more conservative method in multifocal diffuse vulvar carcinomas in situ. Compared with a total vulvectomy, the procedure yields a far better cosmetic result, and sexual sensation is less impaired. The intervention nonetheless often places a significant emotional burden on the patients, who are often very young.

Malignant melanomas account for about 3% of malignant carcinomas of the vulva and require extensive resection, depending on their stage (▶Fig. 1.4).

Vascular malformations or hemangiomas can require surgical correction in the region of the vagina and vulva in children or later in adults (▶Fig. 1.5). Other congenital deviations such as vaginal atresia can also require early genital reconstruction.

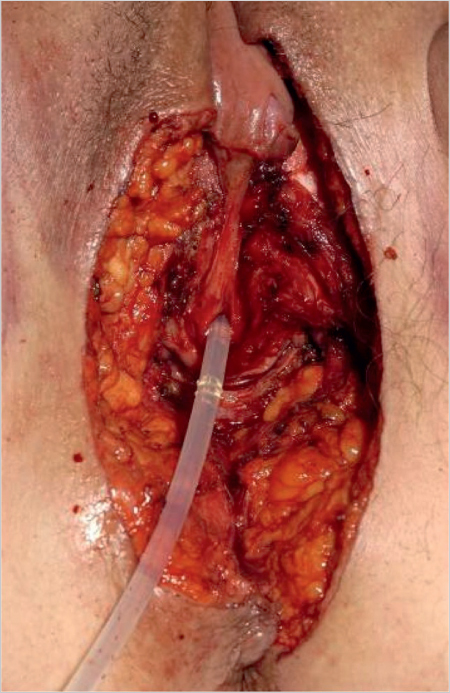
Aside from malignant disease, extensive vulvar defects can also result from necrotizing fasciitis (▶Fig. 1.6). The increase in shaving and piercing in the genital region has coincided with an increased prevalence of this disorder.

Perineal lacerations also warrant mention as a cause of vulvoperineal defects. These soft-tissue injuries occurring during vaginal delivery are divided into four degrees of severity (▶Table 1.1).
The prevalence of first- or second-degree perineal lacerations is said to be about 10 to 15%. More severe perineal lacerations (third degree or higher), occurring in about 1% of all vaginal deliveries, are the most common cause of anal incontinence symptoms and severely impair the patient’s quality of life. Therefore, they should be treated promptly in the immediate postpartum phase. Nonetheless, the sequelae of a perineal laceration, especially scarring and residual soft-tissue defects, often cause physical symptoms that require surgical intervention. The same applies to defects or scarring occurring secondary to surgery such as episiotomy, trauma, or burns (▶Fig. 1.7).

Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree