Wound Closure Techniques
Wound Healing
The inflammatory phase (days 0-5) begins immediately after wounding and within 1 to 2 hours; there is a release of vasoactive substances including histamine, serotonin, and cytokines. These substances cause an increase in local vessel permeability leading to an increased exudation of plasma. The leaky capillaries allow cells such as T lymphocytes, leukocytes, neutrophil granulocytes, monocytes, and macrophages to reach the wound area. Neutrophils (polymorphonuclear leukocytes) predominate in the wound during the first 48 hours after wounding. The polymorphonuclear leukocytes provide a nonspecific cellular defense that is the initial protection against wound infection. The nuclei of neutrophils contain proteolytic enzymes that facilitate cleaning of the wound and phagocytosis of bacteria. Following the neutrophils, macrophages start to migrate into the wounded area and predominate by day 4. The macrophages’ main role is to phagocytose debris and to digest bacteria. At the fourth day of wound healing, fibroblasts begin to appear. During this early phase of wound healing, the tensile strength of the wound is minimal and is the result of the fibrin coagulum in the wound bed.1
In the absence of significant infection or wound contamination, the second stage of wound healing begins. The proliferative or granulation phase (days 6-14) is characterized by the formation of granulation tissue in the wound. Granulation tissue consists of a mixture of cellular elements, including fibroblasts and inflammatory cells, along with newly formed capillaries contained within a matrix of collagen, fibronectin, and hyaluronic acid. Early in the second phase, there is a rapid increase in the numbers of fibroblasts. The increase is secondary to an influx as well as in situ production of fibroblasts.2 Structural proteins required for wound repair are primarily synthesized by fibroblasts. Most important, fibroblasts produce large quantities of collagen, which makes up the majority of the extracellular wound matrix. It is this matrix that is responsible for the tensile strength of scar tissue. The collagen is initially deposited in a disorganized fashion. Through cross-linking, the individual collagen fibrils are subsequently reorganized into regularly organized bundles. The new collagen array is oriented along the lines of mechanical stress in the healing wound. The process of fibroblast proliferation and synthetic activity is termed fibroplasia. Revascularization of the wound proceeds in parallel with fibroplasia.3 Capillary buds sprout from blood vessels adjacent to the wound and extend into the wound space. With continued growth, the new vessels eventually branch at their tips and join to form multiple capillary loops. With formation of capillary loops, blood flow recommences. New sprouts then extend from these loops to form an active capillary plexus.
The differentiation or maturation phase is the third segment of wound healing. This occurs from day 15 to 1 year postoperatively and beyond. During this period, there is a gradual egress of fibroblasts and macrophages. Overall, the wound becomes less vascular. Collagen fibers progress on the continuum from disarray to organization. As the collagen becomes more organized, wound strength continues to improve; 45% of normal wound strength is achieved by day 70 and 50% by day 120.4 In general, with optimal wound healing, scar tissue strength approaches 80% of the original tissue strength before wounding. Many factors contribute to normal wound healing; these are listed in Table 4-1. An understanding of these factors assists successful primary wound closure.
TABLE 4-1
Factors Affecting Wound Healing
| Local Factors | General Factors |
| Blood supply | Age |
| Denervation | Endocrine function (pancreas, thyroid) |
| Fluid collection | Drug therapy (anti-inflammatory, cytotoxic) |
| Infection | Sepsis |
| Previous or concurrent irradiation | Major organ failure (pulmonary, cardial, hepatic, renal) |
| Mechanical stress | Obesity |
| Surgical technique | Malignant disease |
Investigators have used their understanding of wound healing science to guide novel therapies. Lee et al5 showed that the use of laser therapy (intense pulsed light) or microneedle techniques could increase collagen deposition during the wound healing response. An increase in collagen deposition tended to result in improved scar appearance and overall wound healing. Other investigators have shown a decrease in the incidence of scar hypertrophy and an improvement in wound healing by use of lasers to treat scars after surgery.6 Kim et al5 showed that three postoperative treatments of suture line scars with the erbium : glass laser (1550 nm) dramatically improved the appearance of thyroidectomy scars.
Surgical Technique
Local Anesthesia
The pharmacologic action of local anesthetics is to block nerve impulses by disrupting the permeability to sodium during an action potential. The interval between an anesthetic injection and its influence on the action potential is dependent on the pharmacokinetics of the drug used and the dosage administered. There are significant differences in potency and duration between various anesthetic agents. An agent’s potency and length of action depend on its level of hydrophobicity.7 When the agent is mixed with epinephrine, the resulting vasoconstriction increases the time required for clearance of the agent. This reduction in clearance rate increases the agent’s duration of action and decreases the total dosage required to achieve an effective nerve block. Many surgeons use anesthetics containing epinephrine for the added benefit of improved hemostasis.
The core chemical structure of local anesthetics is an amine connected to an aromatic end. The amine end is hydrophilic, and the aromatic end is lipophilic. Changing the amine or aromatic end alters the pharmacokinetics of the drug. There are two classes of local anesthetics based on variations at the amino end: amino amides and amino esters.8 The class of amino amides includes lidocaine, mepivacaine, and bupivacaine. The amino esters group includes tetracaine, cocaine, and benzocaine.
Lidocaine is the most frequently used infiltrative local anesthetic. It is available in a variety of concentrations. A 1% solution is commonly used with or without epinephrine. With a rapid onset of action, it is an ideal choice for simple soft tissue surgery. Bupivacaine has a longer duration of action than lidocaine and thus may be more appropriate for complex wounds requiring prolonged repair times. The author (B.C.M.) prefers a 1 : 1 mixture of 0.5% bupivacaine (Marcaine) and 1% lidocaine with a total concentration of 1 : 100,000 epinephrine. If a surgical procedure is to occur without general anesthesia, 10% by volume of an 8.4% bicarbonate solution is included in the anesthetic mixture. This mixture produces an excellent rapid-onset anesthesia with long-term analgesia. The addition of bicarbonate buffers the solution and decreases injection discomfort.9
During infiltration, the surgeon must avoid intravascular injection. This complication can be minimized by frequent aspiration during introduction of the local anesthetic. Inadvertent intravascular administration can lead to lidocaine toxicity. Central nervous system lidocaine toxicity occurs first. The initial manifestations are excitatory, such as tingling, numbness, mental status changes, and eventually seizures. As lidocaine blood levels increase, there is a progression to central nervous system depression with somnolence and increasing respiratory depression. Higher serum concentrations have cardiovascular effects, such as myocardial depression and arrhythmia.
Incisions
A wide variety of scalpel blades are commercially available for performing skin incisions (Fig. 4-1). For soft tissue surgery, most surgeons prefer the No. 15 blade. This scalpel blade provides a sharp tip for precise angulation and a moderately rounded belly for an efficient cutting surface. A No. 11 blade is often helpful for complex incisions, such as those required for a geometric broken-line scar revision. This blade has an elongated tip with a straight belly that allows an accurate incision of acute angles with short sides. A newer scalpel blade, the 15C, is a modification of the traditional No. 15 blade. This design is a hybrid of the No. 11 and No. 15 designs. An elongated tip with a rounded but low-profile belly allows traditional scalpel use with improved accuracy for complex geometric incisions.

FIGURE 4-1 The diversity of available surgical blades is demonstrated by the No. 15, No. 11, and No. 12 blades.
Soft Tissue Technique
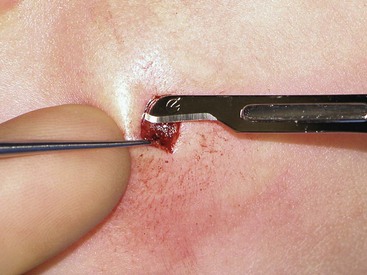
The proper handling of soft tissues is the foundation of successful wound closure and healing. Whether the surgeon is completing a primary wound closure or transferring a local flap, attention should be directed toward the details of wound approximation. Wound closure often begins with the placement of subcutaneous sutures. Proper eversion of the skin at the margin of the wound is required for accurate placement of these sutures. The use of tissue graspers, such as Adson or Adson-Brown forceps, is favored by many surgeons. Although these instruments make tissue handling facile, the operator must be careful not to induce a soft tissue crush injury. An alternative is to use a single-prong skin hook (Fig. 4-2). In this technique, the tissue edge is everted with the skin hook and the operator’s middle finger. The suture needle is then stabilized with the skin hook. After reloading of the needle, the contralateral suture is placed in a similar fashion. Once this technique is mastered, it allows skin edge eversion with less soft tissue trauma compared with the use of tissue forceps for wound repair.
Soft tissue dissection is an essential component of wound closure. Proper technique includes a uniform undermining of the skin for primary wound closure. Whereas there are some tissue planes that lend themselves to blunt dissection (e.g., subgaleal, sub–superficial musculoaponeurotic system), sharp dissection is the general rule. Dissection at the proper depth is facilitated by the use of a single-prong tissue hook. The operator should use the nondominant hand to engage the skin hook while the dominant hand holds the scalpel. The middle finger of the nondominant hand then relays tactile information while maintaining traction to aid the dissection (Fig. 4-3). Although this two-handed technique can be technically challenging, its use results in a more consistent plane of dissection.
Various methods of wound closure are detailed later in this chapter. Each of these methods relies on the fundamental principle of a tension-free wound repair. Achieving a tension-free wound closure is important in the short-term to prevent wound dehiscence and to promote tissue viability. Wound closure tension also plays a role in the long-term appearance of the scar.10 In soft tissue surgery, a number of techniques should be used to decrease wound closure tension. Undermining of the soft tissue at the wound edge will allow easier approximation. Depending on the anatomic location and depth of dissection, a layered closure with deep buried sutures will effectively diminish wound strain. For some procedures, a series of relaxing incisions, such as galeatomies beneath the forehead skin, allow the recruitment and advancement of adjacent tissue and reduction of wound closure tension.
When undermining and layered wound closure fail to minimize wound closure tension, the surgeon may elect to alter the mechanical properties of the skin itself. Because skin is viscoelastic, its intrinsic shape can be altered by mechanical creep. Mechanical creep is defined as the elongation of skin beyond the skin’s intrinsic extensibility by a constant load over time. The stretching is usually performed intraoperatively, and tissue lengthening is due to collagen realignment, displacement of fluids, and fragmenting of elastin fibers. The force used to elicit mechanical creep may be applied with standard instruments, such as towel clamps applied to the skin (Fig. 4-4), or with a number of commercially available devices. Disadvantages of rapid intraoperative skin expansion include tissue damage and problems with extrusion of the expanding device. A promising technique has been the use of external tissue expanders. These devices work more slowly than intraoperative devices. They apply steady and significant tissue traction around an open wound without causing tissue trauma. They are effective in assisting in closure of large wounds that cannot be repaired with conventional techniques.11
A large variety of needle drivers are available to surgeons. The delicate nature of soft tissue work creates a number of requirements for these instruments. The jaws of the driver must be able to effectively grasp the small-caliber needles commonly used for facial skin closure. In addition, the instrument should accommodate the wrist pronation required for proper suture placement. The small-caliber Castroviejo needle driver is an excellent choice for soft tissue work (Fig. 4-5). With its unique design, the locking version of the Castroviejo provides excellent needle traction while allowing more ergonomic wrist pronation. The result is a more accurate and consistently placed suture.
Wound Apposition
Wound repair should be performed with the least wound closure tension necessary to approximate the wound margins. Wound closure tension can be minimized with the placement of proper subcutaneous sutures. The addition of dermal sutures will also assist with reduction of dead space and skin edge eversion. The path of such sutures should start and end at a point farthest from the surface of the skin. On placement of dermal sutures, care must be taken to match the entry and exit points of the suture on both sides of the wound. Misplaced sutures will result in uneven wound edges and poor skin edge eversion. An equal distribution of wound closure tension is achieved by inserting the suture needle below and parallel to the surface of the skin, following the curve of the needle and exiting below and parallel to skin on the contralateral side of the wound. Poor eversion of skin edges results when the needle enters too far from the skin edge or at an improper angle.
Once the subcutaneous tissue layers of a wound have been approximated, the method of cutaneous closure must be determined. Suture remains the “gold standard” material for repair of skin incisions. Sutures are highly adaptable to complex wounds and may be tailored to each individual wound. The limiting aspect for all cutaneous suture techniques is the time required to perform the procedure. When suture closure is performed, with or without deep sutures, the surgeon must use precise techniques to promote skin eversion (Fig. 4-6). At the completion of an ideal wound closure, the skin edges will be slightly everted. In time, with wound contraction, the everted skin edge will retract to leave an aesthetic cutaneous scar. In contrast, when skin edges are approximated without eversion, contractile forces may result in a depressed or widened scar. Sutures that are placed too far from the wound edge may result in telltale suture marks (i.e., train tracks) from pressure necrosis (Fig. 4-7).
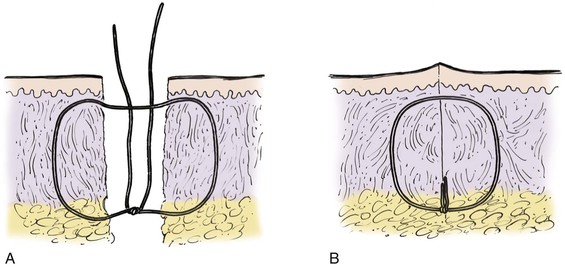
FIGURE 4-6 Schematic diagram of deep suture placement. Placement of deep sutures should eliminate dead space and accomplish wound edge approximation and eversion.

FIGURE 4-7 A, Proper placement of cutaneous suture showing equal distribution of tension along entire wound edge. Everted surgical wound edges provide aesthetic result. B, Improper placement of cutaneous suture with surgical bite too far from skin edge and too superficial. This creates vector forces that are greatest in a horizontal direction and produces inverted wound. C, Improper placement of cutaneous suture farther from skin edge with more superficial surgical bite. Force vectors on wound are greater in a horizontal direction and create more wound inversion. In addition, permanent suture marks result in areas of pressure necrosis where wound closure tension is greatest.
The most basic cutaneous suture is the simple interrupted suture (Fig. 4-8). This technique enables the surgeon to adjust to variations in the level of the wound edges with each individual suture. Whereas an excellent wound closure can be achieved with this technique, it is time-consuming. If the level of the wound edges does not require many adjustments, they may be approximated with a simple continuous (running) suture (see Fig. 4-8). This method provides a rapid wound repair and an even distribution of wound tension along the length of the incision. Wounds near an area of increased motion, such as the lips or medial cheeks, may benefit from an interrupted suture repair. More stress is placed on cutaneous sutures in these areas compared with other regions of the face, and as a result, there is a greater risk for sutures to break. Should this occur to a continuous suture, wound dehiscence is likely.
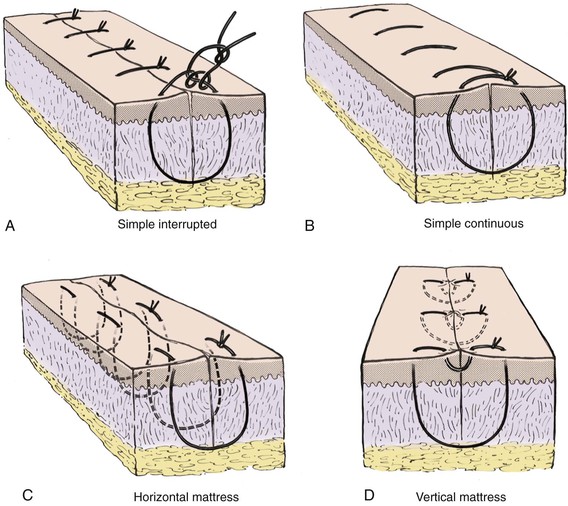
FIGURE 4-8 A, Simple interrupted suture. B, Simple continuous suture. C, Horizontal mattress suture. D, Vertical mattress suture.
The cutaneous suture that creates maximum wound edge eversion is the vertical mattress suture. This suture passes in arcs from two opposing points distal to the wound margin to two opposing points immediately adjacent to the wound margins (see Fig. 4-8). When it is tied, this suture provides vectors of force that maximize wound edge eversion. It also has the benefit of decreasing dead space compared with a simple interrupted or simple continuous cutaneous suture. The horizontal mattress suture does little to decrease dead space, but like the vertical mattress suture, it provides maximum wound edge eversion (see Fig. 4-8). A horizontal mattress suture is placed by taking two equidistant bites of tissue on either side of the wound in a purse-string fashion.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree