Widespread rashes
Georgina E Elston MRCP
Graham A Johnston FRCP
Introduction
In order to diagnose a rash correctly, a history and examination are necessary. An experienced dermatologist may be able to take one look at a rash and come up with a diagnosis but, for the less experienced, the history, distribution, configuration, and morphology of the rash will point to the correct diagnosis or differential.
Urticaria
Introduction
Urticaria is characterized by an acute eruption of recurring, pruritic papules and plaques (3.1). It is often self-limiting, but in many patients becomes chronic and relapsing where it can greatly impair quality of life.
Clinical presentation
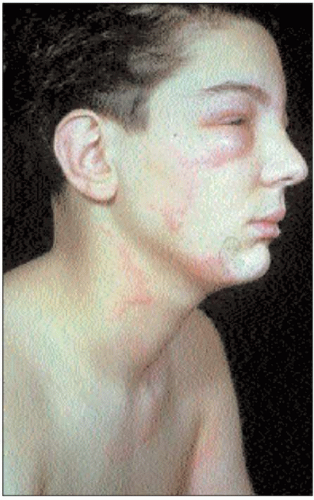
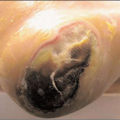
An urticarial rash consists of weals: pruritic, raised, oedematous papules and plaques, usually erythematous with a pale centre. Scaling is always absent. An important clinical clue is that individual lesions appear on any part of the skin within a few minutes and will have resolved within 24 hours, although new lesions may be appearing elsewhere on the skin. Another clue to the diagnosis is if the patient is dermographic (although not demonstrable in all cases) (3.2). A firm, but gentle, scratch of the skin with an orange stick will produce a linear weal within 5-10 minutes. Rarely, the condition is associated with angio-oedema where there can be swelling of the lips, tongue, and around the eyes (3.3).
Histopathology
A biopsy is not usually indicated for diagnostic purposes, as the features are nonspecific, with oedema and a mixed dermal inflammatory infiltrate. However, histology can exclude the possibility of urticarial vasculitis.
Differential diagnosis
Drug reactions should be considered if there is a history of new drugs preceding the rash (3.4). In urticarial vasculitis, lesions persist for more than 24 hours and resolve with bruising. Contact urticaria should be considered if local applications of products preceded the rash (3.5). Papular urticaria is possible if there is a history of contact with mosquitoes, bed bugs, or fleas (are their pets scratching too?) (3.6, 3.7).
Management
Acute urticaria, normally triggered by drugs, food, or infections has a good prognosis, resolving in less than 1 month. Treatment is symptomatic with high-dose antihistamines.
Chronic urticaria lasts longer than 6 weeks and may continue for many years in some cases. It is idiopathic in the vast majority of cases and investigations are not indicated. Again treatment is with single or combination high-dose antihistamines and avoidance of associated triggers (which may include pressure, sun exposure, and exercise, although there is usually no history of a trigger). Addition of H2 blockers such as cimetidine as well as the tricyclic antidepressant doxepin can also be helpful.
Erythroderma
Introduction
Erythroderma is an acute and serious medical condition that can make patients feel shivery and unwell. Patients should be admitted to hospital for close monitoring and treatment.
Clinical presentation
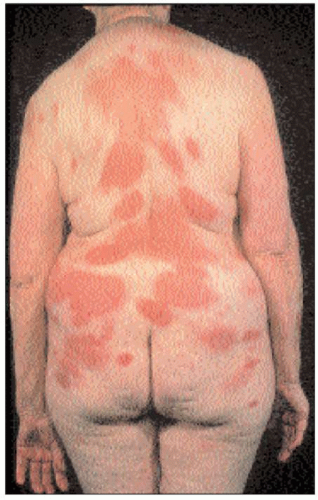
Erythroderma simply means red skin with involvement of over 90% of the skin surface area. The skin is angry, inflamed, and hot to touch. Usually there is a surface scale, which may be fine or coarse (3.8, 3.9 and 3.10). The skin is not always itchy. Patients become acutely unwell with fever,
shivering, malaise, and lethargy due to the considerable loss of heat, fluid, and protein from their inflamed skin. Palmoplantar involvement is common, with hyperkeratosis and fissuring. Nails can exhibit onycholysis or may even shed. Hair loss can occur with scalp involvement. Patients become dehydrated and hypothermic as a result of insensible fluid loss from the skin. Peripheral oedema develops due to low albumin and high output cardiac failure. Lymphadenopathy may be found but should alert one to the possibility of cutaneous lymphoma.
shivering, malaise, and lethargy due to the considerable loss of heat, fluid, and protein from their inflamed skin. Palmoplantar involvement is common, with hyperkeratosis and fissuring. Nails can exhibit onycholysis or may even shed. Hair loss can occur with scalp involvement. Patients become dehydrated and hypothermic as a result of insensible fluid loss from the skin. Peripheral oedema develops due to low albumin and high output cardiac failure. Lymphadenopathy may be found but should alert one to the possibility of cutaneous lymphoma.
Histopathology
A biopsy may be nonspecific in the early stages but can help differentiate psoriasis and eczema. The presence of eosinophils would lead to a careful inquiry about drugs including nonprescribed medication.
Differential diagnosis
There are four main causes of erythroderma:
Less common causes include pityriasis rubra pilaris and seborrhoeic dermatitis. Clues to the cause include a preexisting dermatosis or recent changes of medication. Consider lymph node biopsy and CT/MRI imaging if lymphoma is suspected.
Management
Patients should be admitted to hospital. Liberal and frequent application of bland emollients should be applied to the whole skin. Careful attention to fluid and electrolyte balance is needed, and protein replacement with high calorie/protein supplements should be considered. This condition can be life threatening, particularly in the elderly, who may develop infections, hypothermia, and associated high output cardiac failure.
Atopic eczema
Introduction
Atopic eczema usually presents in childhood and settles spontaneously by the teenage years. In some patients atopic eczema persists into adult life or can start for the first time in adulthood. Asthma and hay fever are commonly associated with this condition or may be found in first-degree relatives.
Clinical presentation
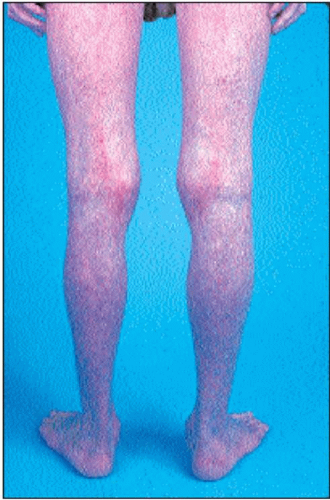
The clinical features include generalized xerosis (dry skin) and red, itchy, patches and plaques of dry, scaly skin with overlying excoriations (3.10, 3.12). More chronic disease presents with thickening of the skin with accentuation of the surface markings (lichenification) (3.12). This is a consequence of continual scratching. In patients with darker skin there will also be hyperpigmentation at the site of the eczema. The distribution usually includes the popliteal and antecubital fossae but may involve any site (3.12, 3.13 and 3.14). White dermographism is a clue to the diagnosis, being a white line produced after gentle scratching of the skin. Palmo-plantar involvement often presents with erythema, vesicles, scaling, and painful fissures.
Histopathology
Intercellular oedema (spongiosis) is the hallmark of eczema. Intraepidermal vesicles associated with a lymphocytic infiltrate are also seen. In more chronic disease, psoriasiform hyperplasia occurs.
Differential diagnosis
Seborrhoeic and discoid dermatitis need to be considered. Patch testing is helpful if the history is suggestive of allergic contact dermatitis. In scabies, which is often complicated by an infected eczema, look for the presence of burrows, particularly with genital involvement.
Management
Emollients should be applied regularly to the dry skin and used as soap substitutes. Topical steroids are the mainstay of treatment and the strength needed varies depending on the site, severity, and chronicity of the eczema. Ointments are preferable to creams in the majority of cases where the skin is dry and scaly. Calcinuerin inhibitors are useful alternatives to steroids for facial eczema. They should not be used if patients get recurrent herpes infections, and patients should avoid direct sunlight. Oral steroids are sometimes required for severe flares of eczema and are preferred in short courses.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree