Vertical Rectus Abdominis Myocutaneous Flap for Perineal Reconstruction
Sahil K. Kapur
Charles E. Butler
DEFINITION
The vertical rectus abdominis myocutaneous (VRAM) flap plays a beneficial role in improving postoperative outcomes for patients with defects created following abdominoperineal resection (APR) and pelvic exenteration (PE) surgery.
Complications following APR and PE are related to large noncollapsible dead space, commonly irradiated dead space, with poor vascularity and bacterial contamination.1
The flap provides healthy vascularized tissue to help obliterate the pelvic dead space—created after the resection. It serves as a barrier between the abdominal and pelvic cavity, as well as a source of skin and soft tissue for reconstructing and resurfacing the perineum.
ANATOMY
The rectus abdominis muscle originates from the 6th, 7th, and 8th costal cartilages and inserts on the pubic bone. It measures approximately 6 cm in width at its origin and 3 cm in width at the insertion.
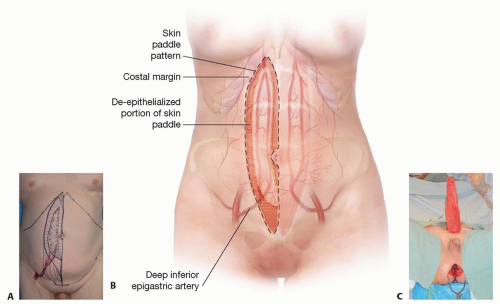
It has a dual codominant blood supply (Type III Mathes/Nahai). Superiorly, it is supplied by the superior epigastric artery, a branch of the internal thoracic artery. Inferiorly, it is supplied by the deep inferior epigastric artery a branch of the external iliac artery.
The deep inferior epigastric artery originates from the external iliac vessels at a point between the inguinal ligament to about 6 cm above it. The vessel enters the posterior rectus sheath at about the level of the ASIS and the arcuate line (4 to 6 cm above the pubic bone). This artery usually splits into a lateral and medial branch that supplies the lateral and medial row of myocutaneous perforators. Knowledge of perforator anatomy is important when attempting the fascial-sparing approach of VRAM harvest.
The skin paddle for the VRAM flap is usually designed to include paraumbilical myocutaneous perforators. Extension of the skin paddle superiorly can be carried out without taking additional fascia (extended VRAM flap as described later). This is possible because the intercostal perforators supplying the extended portion have direct perforator-to-perforator connections with the epigastric perforators in the standard skin paddle.2
PATIENT HISTORY AND PHYSICAL FINDINGS
Patients are assessed preoperatively to determine risk factors that would increase complication rates such as obesity, hernia, smoking, steroid treatment, and prior chemoradiation.
A detailed surgical history is important to ensure that the patient has not had any prior surgeries that could have injured the deep inferior epigastric artery pedicle. Surgeries such as C-sections have a more medially placed scar and generally do not lead to pedicle injury. Prior abdominoplasty surgery is a relative contraindication to the use of a skin paddle because the perforators have been divided.
Physical examination includes an examination of the abdomen and pelvic region for scars and assessment of hernias.
IMAGING
Imaging involving CT or MRI is generally available because most patients have undergone an oncologic workup. CT images help determine the amount of diastasis, integrity and bulk of lateral abdominal musculature (in case a component separation is needed), and the presence of hernias.
No special imaging to assess perforators is necessary for this reconstruction.
SURGICAL MANAGEMENT
Preoperative Planning
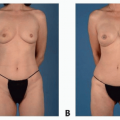
Patients with pelvic or perineal defects benefit from pedicled VRAM flap reconstruction. The flap is based on the deep inferior epigastric artery. A skin paddle is used to provide skin resurfacing of the perineum. It can be de-epithelialized to provide bulk if necessary when the perineal skin is completely closed.
Positioning
Patients are generally positioned in the lithotomy position by the resecting team. All areas of resection including the perineum and the abdomen beyond the level of the costal margin are prepped into the field.
Approach
In general, two or more teams are involved. The reconstructive team will begin the operation if a fascial-sparing technique is to be used. The reconstructive team performs the laparotomy and spares the medial aspect of the anterior rectus sheath. Following the oncologic resection, the reconstructive team performs their portion of the procedure.
The ostomy(s) are matured after the reconstruction is completed and the abdomen is closed.
TECHNIQUES
▪ Flap Harvest
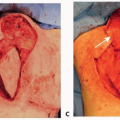
Make a midline skin incision, and dissect down to the linea alba (TECH FIG 1A,B).
Once the rectus sheath is identified, begin dissecting laterally, superficial to the rectus sheath, to locate periumbilical and medial row perforators to the skin paddle.
Incise the anterior rectus sheath 2 to 3 cm lateral to the midline but medial to the medial row perforators.
Retract the rectus abdominis muscle laterally to expose the posterior rectus sheath.
Incise the posterior rectus sheath 2 cm lateral to the midline to gain intraperitoneal access. Curve the incision back toward the linea alba at the arcuate line.
Advance and suture the posterior rectus sheath to the anterior rectus sheath to protect the rectus abdominis muscle during the resection component of the procedure.
Resume reconstruction once the resection has been completed. The ostomy is usually passed through the contralateral rectus abdominis muscle and matured by the primary team after the reconstruction and abdominal closure.
Examine the perineal defect to estimate the bulk and nature of tissue needed. This information is used to decide if a skin paddle will be used or the perineal skin will be closed primarily over the flap.
Design the skin paddle over the rectus abdominis muscle such that it will reach the defect once the muscle is transposed.

Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree