Fig. 23.1
The Vaser System: (Left) First version (2001/2012). (Right) Second version (2013)
1.
Infiltration system with flow rate control (tumescent infiltration)
2.
Ultrasound device for selective fat destruction thus emulsification (Vaser handpiece and probes)
3.
Negative pressure aspiration and collection of emulsified fat in disposable canister (VentX)
Foot pedals control infiltration of fluids and ultrasound delivery. Amplitude is adjustable at the console with increment from 10 % from 0 to 100. Solid titanium probes (2.2, 2.9, 3.7, and 4.5 mm in diameter) are used to selectively emulsify body fat. Choice of probe diameter depends on tissue type (less or more fibrotic) or thickness and location of body surgery. Probes have 1, 2, 3, or 4 rings at the end of the shaft to better treat the fat, depending on the amount of existing fibrosis in fat tissue. The number of rings of probe is intended proportional to the amount of fibrosis present (less rings in more fibrotic tissue). The Vaser system provides administration of continuous energy as well as interrupted (50 % of energy in the same amount of time), so-called pulsed, very effective when treating more fibrotic tissue and superficial layers.
As a crucial guideline, an appropriately sized and grooved Vaser probe is selected depending on the volume of fat present and how much the tissues are soft and fibrous. For superficial definition and contouring of the abdominal region, use 3.7 mm, two-grooved probe, at amplitude of 80–90 % in a continuous mode, with an adequate amount of tumescent infiltration provided.
The author normally infiltrates tumescent solution superficially first and then deeply. The reason is that tumescence is a temporary condition, and the author started operating with Vaser, starting first on the superficial layer and then the deeper, to prove that the tumescence was really effective. With this strategy, pulsed Vaser mode was never needed to be utilized in the author’s experience (around 300 cases a year as average, plus those treated before with first-generation ultrasound technology, SMEI).
Vaser technology advantages are as follows if compared with traditional liposuction, power assisted liposuction, and others [2]:
1.
Blood loss is always lower as Vaser is a selective technique, which targets only fat cells, sparing vessels, nerves, etc.
2.
Less aggressive technique, less bruising, less trauma, and faster recovery time.
Minimal discomfort to patients, as not damaging nerve structure (traditional techniques provide a blind removal of tissue of the subcutaneous layers, without selection, thus imply more bleeding and pain, not sparing vessels and nerves) especially in fibrotic areas or back and posterior flanks
3.
Vaser is a soften technique, with a less effort for the surgeon, as the Vaser probes act to gently emulsify fat, and to aspirate the emulsified fat to follow.
4.
Vaser main indication is to work in the superficial layer of subcutaneous tissue to undermining without caring of wasted irregularities, and to allows better skin retraction of tissues.
5.
The majority of fat aspirated following treatment with Vaser is viable.
This allows surgeon to harvest fat for contouring the buttocks, hips, breast, and abdomen in body enhancement cases [4].
23.2 Male Abdominal Contouring
The ideal shape of a well-defined male abdomen is the so-called six packs or eight packs (Fig. 23.2). This was drawn by Leonardo da Vinci and by Michelangelo Buonarroti (Figs. 23.3 and 23.4). It includes enhanced transition zone from the lateral bellies of the rectus abdominis muscle and the oblique muscle (vertically) and the linea alba (vertically) where natural depression and “shadow” should be created.
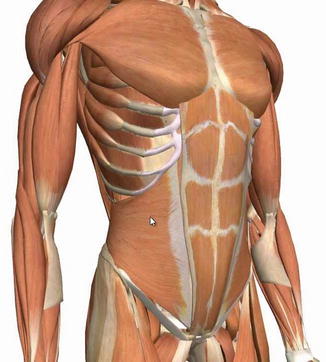
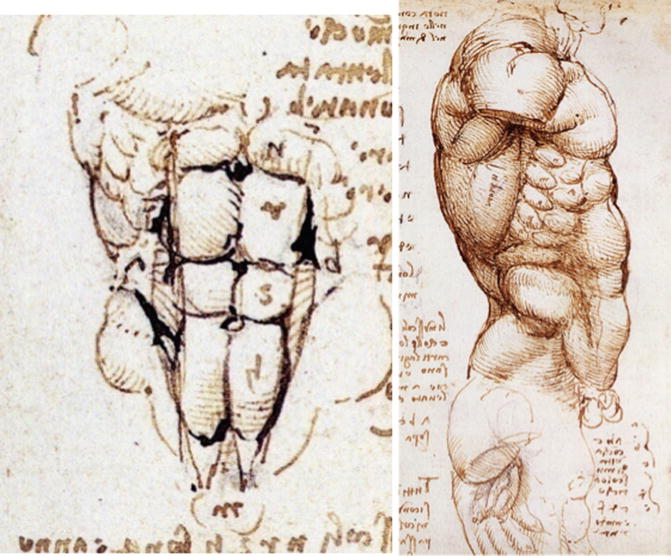

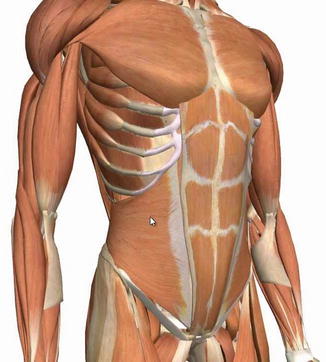
Fig. 23.2
Male anatomy of the abdominal wall and oblique muscles
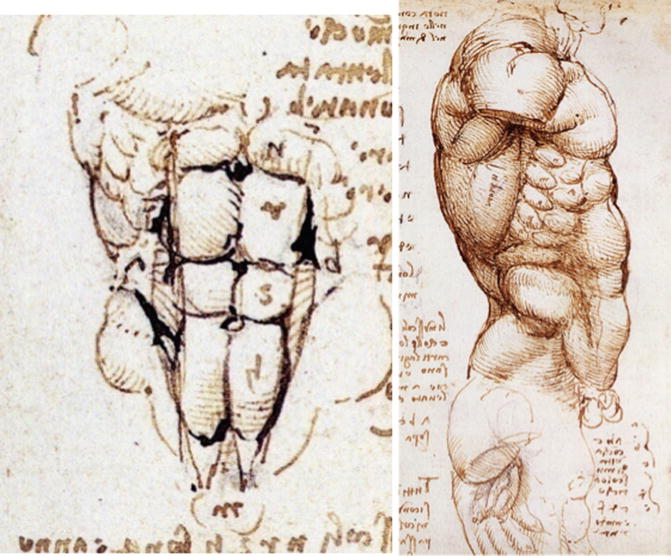
Fig. 23.3
Leonardo da Vinci’s anatomical drawings

Fig. 23.4
Michelangelo Buonarroti’s Sistine Chapel drawings
More horizontal lines and depressions with very superficial thinning should re-create the evidence of the rectus abdominis muscle fascia and belly, enhancing definition [3]. The possibility of producing an athletic muscular appearance depends on:
1.
Body type of patient, thus body mass index standing
2.
Genetic–hereditary condition
3.
Fat localization (intra-/extra-abdominal)
4.
Attitude to healthy lifestyle and exercise to work out in muscle strength
23.2.1 Markings
All patients are marked in the standing position, in standard cases: marking the rib cage first, to prevent perforation in this area, lateral edges of rectus abdominis, and the linea alba carefully and marking the hip contour, edge of the latissimus dorsi, and the pectoralis muscle (as required in high definition cases or when combined with other body contouring procedures of chest, as gynecomastia) (Fig. 23.5).


Fig. 23.5
Markings
23.2.2 Skin Incisions
Two incisions are made at the pubis line, one at the lower margin of xiphoid and two others below the nipple to approach chest as well when needed. Umbilical incision is complementary to access vertical midline. Further skin incisions could be placed at the lateral upper margin of the rectus muscles if needed (Fig. 23.6).


Fig. 23.6
Skin incisions
23.2.3 Technique
The majority of the author’s procedures are in abdominal wall contouring that are performed under general anesthesia. The reason is in the sensibility of the area and the aggressiveness of the surgery, which involves superficial and deep layers; in selected cases, tumescent anesthesia and sedation are used.
23.2.4 Infiltration
Even when the procedure is performed under general anesthesia, tumescent solution is used with 1000 mL of saline solution, 1 mL of adrenaline, and 300 mg of lidocaine. The amount of lidocaine added helps the postoperative analgesia of all the area, as lidocaine is slowly absorbed and released in the following 48 h after surgery. There are no fixed rules in the terms of ratio of infiltration and extraction of the emulsified fat. By evaluating the case, the author knows how much will be needed in terms of infiltration for abdominal contouring. From 1000 mL (minimum) to 5000 mL (maximum) in big cases, with a medium average of 2000–2500 mL in standard cases (abdomen + anterior flanks, plus more 1000 mL are needed in chest approach).
The superficial layers are infiltrated first and then deeper. The reason is tumescence is a temporary state and will not last much if not treated first, as for gravity forces the fluids drop to lower areas.
23.3 Vaser Emulsification
The procedure is started in the superficial layers first when the firmness of tissue is maximized (Fig. 23.7). Ultrasound requires fluids to act properly through the cavitation phenomenon, and fluids decrease the density of tissue thus letting fragmenting and easier penetration of probes. The author does not wait 10–12 min before starting ultrasound probe action. The reason is that you need to wait for the effect of analgesia when you work under local tumescent anesthesia and sedation but not with general anesthesia. You do not need to wait for the onset of adrenaline added to the tumescent solution when performing Vaser ultrasound.
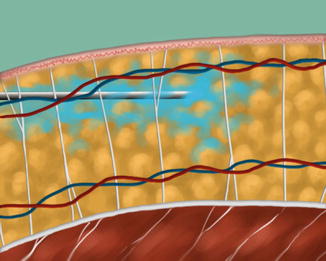
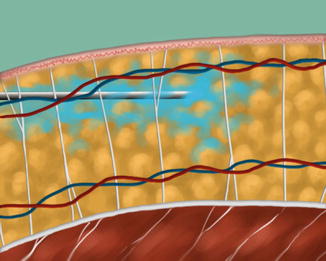
Fig. 23.7
Vaser emulsification
Vaser is selective, so it does not affect vessels when inside the body. The technique is going to be bloodless initially as soft undermining of tissues of superficial layers is performed. When the aspiration of the emulsified fat is performed, the inset of adrenaline has taken place. The superficial layers are treated with 3.7 mm Vaser probes, usually 2–3 rings (Fig. 23.8).


Fig. 23.8
3.7 mm, 2.9 mm Vaser probes: 1, 2, 3 rings
Only once the procedure is completed, the emulsification passes to deep layers, where larger probe (4.3 mm diameter) to speed up emulsification can be utilized. Deep emulsification is close to muscle layer, to be sure to remove really all the fat from the areas. Probes feel the muscle, but has to be oriented parallel to the muscle orientation, to avoid puncture and damage to the muscle fascia and risk of penetration.
The Vaser probe’s action is continuous until all the fat layers are “fed” and no further “resistance” is encountered. This is a clinical feeling that the surgeon learns in clinical practice.
Minutes of Vaser action are an indication of the emulsification needed as well as undermining needed.
The definitions are:
1.
Superficial undermining of tissue – the subcutaneous liberation of adherences with middle and deeper fat layers. This phase is what makes Vaser unique as a technology. This creates a thin superficial flap (but perfectly vascularized), which is then free to retract and redrape to the underlying frame, once this is properly reduced of the extra fat layer present.
2.
Deep layer fat emulsification to debulk the volume of fat deposit is extended to middle and deep fat layers.
The abdomen has a clear distribution at the Scarpa’s fascia, which separated the intermediate and deep fat layers. The body needs to be addressed to compare the debulking process. Vaser timing for an abdominal contouring could range between 10 and 30 min (Fig. 23.9). The superficial phase is the most challenging one. The surgeon must learn that Vaser probe gently removes inside the superficial layers of subcutaneous tissues. No forceful action is needed to speed up the process. Probes advance gently into tissues, and if resistance is encountered, the surgeon must change angle of action eventually.
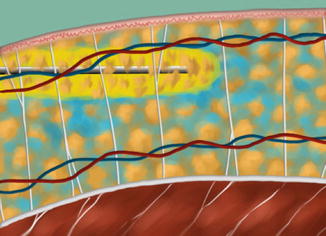
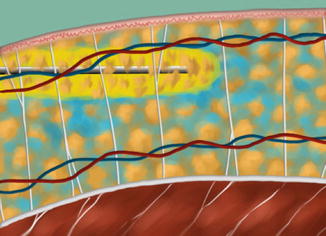
Fig. 23.9
Vaser ultrasound action
Vaser ultrasound is not standard liposuction. Standard liposuction is a mechanical blind destruction of fat and of the tissues underlying skin, with forceful aspiration of all tissues. Vaser is a selective emulsification of fat tissue alone, sparing nerves and vessels, and gentle aspiration of emulsified fat. No force is needed to utilize Vaser probes.
23.3.1 Aspiration (Fig. 23.10)
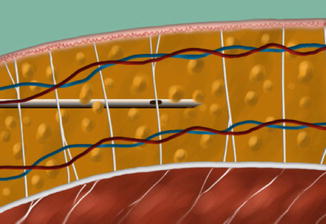
Fig. 23.10
Aspiration of emulsified fat
The final target of aspiration is to shape the body (abdomen, flanks, and chest). So the plastic surgeon must work as an artist in this phase and have a clear plan of action on how to obtain the desired shape.
The author normally starts from flanks with the lower lateral inferior incisions. The goal is to create the tinier possible flap in the area of the oblique muscle and to obtain a nice contouring and definition of this transition area with the vertical lateral edge of the rectus abdominis muscle (bilaterally).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree







