Vascular anomalies are disorders of the endothelium that can affect each part of the vasculature (capillaries, arteries, veins, or lymphatics). Although nearly always benign, vascular anomalies can involve any anatomic structure. Significant progress in understanding and treating patients with vascular anomalies has been made during the past quarter century since the introduction of a biologic classification for these lesions.
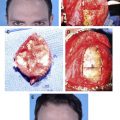
Vascular anomalies are disorders of the endothelium that can affect each part of the vasculature (capillaries, arteries, veins, or lymphatics). Lesions are usually diagnosed during infancy or childhood and are common; the estimated prevalence is 4.5%. Although nearly always benign, vascular anomalies can involve any anatomic structure. The most common problem is psychological morbidity caused by disfigurement; many lesions affect the head and neck. Local complications include bleeding, destruction of anatomic structures, infection, obstruction, pain, thrombosis, and ulceration. Vascular anomalies can also cause congestive heart failure, disseminated intravascular coagulation, pulmonary embolism, thrombocytopenia, and sepsis.
The field of vascular anomalies is confusing because (1) numerous types of vascular anomalies exist, (2) different lesions often look similar, and (3) many practitioners use imprecise terminology. Because vascular anomalies most commonly involve the integument, patients are often referred to a plastic surgeon. Although the reconstructive surgeon can manage many lesions independently, several types of anomalies require the care of additional specialists.
Significant progress in understanding and treating patients with vascular anomalies has been made during the past quarter century since a biologic classification for these lesions was introduced. For example, imaging instead of biopsy is now the standard for diagnostic confirmation, antiangiogenic drug treatment is available for problematic vascular tumors, sclerotherapy has replaced resection of vascular malformations in many instances, and techniques for excision have been improved. Several multidisciplinary vascular anomalies centers now serve as regional, national, or international referral sites. However, despite improvements in the management of vascular anomalies, these disorders continue to cause significant morbidity and their etiopathogenesis remains poorly understood.
Terminology
The field of vascular anomalies has been impeded by imprecise terminology that has created diagnostic confusion, blocked communication between physicians, inhibited research, and caused incorrect treatment. Historically, vascular anomalies were labeled descriptively, according to the type of food they resembled (cherry, strawberry, port wine). Vascular anomalies were later divided histopathologically into angioma simplex, angioma cavernosum, or angioma racemosum; these terms became synonymous with superficial hemangioma, deep hemangioma or venous malformation (VM), and arteriovenous malformation (AVM), respectively. Lymphatic malformation (LM) was separated into lymphangioma or cystic hygroma.
Capillary or strawberry hemangioma became associated with hemangioma affecting the dermis, which appears red. Hemangioma located below the skin is blue and was often called cavernous hemangioma. The terms capillary and cavernous were also used to describe capillary malformation (CM) and VM, respectively. Another label for CM was port-wine stain. Cystic hygroma and lymphangioma became common terms for macrocystic and microcystic lymphatic malformations, respectively. To add to the confusing terminology, hemangioma continued to be used to describe any type of vascular anomaly, including both tumors and malformations.
Classification
A biologic classification clarified the field of vascular anomalies by categorizing lesions based on their clinical behavior and cellular characteristics ( Table 1 ). Vascular tumors rapidly enlarged postnatally and demonstrated endothelial proliferation. Malformations were errors in vascular development and had stable endothelial turnover; lesions were named based on the primary vessel that was malformed (capillary, arterial, venous, lymphatic). The terminology was further clarified because the suffix “-oma”, meaning upregulated cellular growth, was reserved for vascular tumors. Thus, terms such as lymphangioma (microcystic lymphatic malformation), cystic hygroma (macrocystic lymphatic malformation), and cavernous hemangioma (VM), which describe nonproliferating malformations, were abandoned. Using this classification, 90% of vascular anomalies could be correctly diagnosed by history and physical examination. This classification was accepted by the International Society for the Study of Vascular Anomalies (ISSVA) in 1996 ( Table 2 ).
| Hemangiomas | Malformations |
|---|---|
| Proliferating phase | Capillary |
| Involuting phase | Venous |
| Arterial | |
| Lymphatic | |
| Fistulae |
| Tumors | Malformations | |
|---|---|---|
| Simple | Combined | |
| Hemangioma | Capillary (C) | AVF, AVM, CVM, CLVM LVM, CAVM, CLAVM |
| Others | Lymphatic (L) | |
| Venous (V) | ||
| Arterial (A) | ||
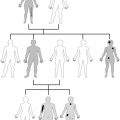
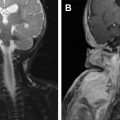
The most common vascular tumors consist of infantile hemangioma (IH), congenital hemangioma (CH), pyogenic granuloma, and kaposiform hemangioendothelioma (KHE) ( Fig. 1 ). Malformations are divided into rheologically slow-flow lesions (CM, VM, LM) or fast-flow anomalies (AVM, arterial aneurysm/atresia/ectasia/stenosis) ( Fig. 2 ). Combined vascular anomalies, most commonly lymphatic venous malformation, can also occur. Eponymous syndromes that include vascular anomalies exist; one example is Klippel-Trénaunay syndrome, a capillary lymphatic venous malformation of an extremity with overgrowth.
The classification of vascular anomalies continues to expand and has become more precise as the knowledge of these lesions evolves ( Table 3 ). For example, CHs and KHE have been differentiated from IH. Genetic studies have identified subtypes of VMs (cutaneomucosal, glomuvenous). New vascular anomalies have recently been characterized (ie, capillary malformation–arteriovenous malformation, phosphatase and tensin homolog–associated vascular anomaly).
| Tumors | Malformations | |
|---|---|---|
| Slow Flow | Fast -Flow | |
| IH | CM Cutis marmorata telangiectatica congenita Telangiectasias | AM Aneurysm Atresia Ectasia Stenosis |
| CH Rapidly involuting congenital hemangioma Noninvoluting congenital hemangioma | LM Microcystic Macrocystic Primary lymphedema | AVM CM-AVM Hereditary hemorrhagic telangiectasia PTEN-AVA |
| Hemangioendotheliomas KHE Others | VM Cerebral cavernous malformation Cutaneomucosal venous malformation Glomuvenous malformation Verrucous hemangioma | Combined malformations Capillary arteriovenous malformation Capillary lymphatic arteriovenous malformation |
| Pyogenic granuloma | Combined malformations Capillary venous malformation Capillary lymphatic malformation Capillary lymphatic venous malformation Lymphatic venous malformation | |
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree