CHAPTER 6 Use of Compression Therapy
Historical Development
The oldest known illustration of compression bandages dates back to the Neolithic Age (5000–2500 BC) (Fig. 6.1).1 The ancient Hebrews, Egyptians, Greeks, and Romans used compression therapy for treatment of wounds and ulcers, as described in the Smith Papyrus (1650–1552 BC) and in the Book of Isaiah (Isaiah 1:6), eighth century BC.2 Hippocrates wrote about compression treatment in the fourth century BC, and this was followed by further refinements from Celsus and Virgo. Roman soldiers who marched for days at a time learned quickly that applying tight strappings to the legs reduced leg fatigue. The knowledge concerning the beneficial effects of compression was rediscovered by physicians during the Middle Ages, including Guy de Chauliac (1363), Giovanni Michele Savonarola (1440), and Fabrizio d’Aquapendente (1537–1619). They used compression bandages, plaster dressings, and laced stockings made from dog leather.3

Figure 6.1 Mural paintings in the Tassili caves (Sahara), 5000–2500 BC.
(From Partsch H, Rabe E, Stemmer R, Compression therapy of the extremities, Paris, 1999, Editions Phlébologiques Francaises.)
Ambroise Paré (1510–1590), Richard Wiseman (1622–1676), Christian Anton Theden (1714–1787), and Thomas Baynton (1797) were pioneers, especially in the treatment of leg ulcers, recommending different kinds of compression material that were mainly inelastic. In 1885, the dermatologist Paul Unna introduced his zinc paste boot for the treatment of venous dermatitis, and in 1910, his pupil, Heinrich Fischer, recommended firmly applied ‘Unna boots’ for treating venous thrombosis.3,4
The use of elastic compression occurred with the development of elastic stockings in the mid 1800s and the discovery by Charles Goodyear in 1839 of a vulcanizing process for rubber that would increase its elasticity and durability. In 1839, John Watson, MD, reported on the usefulness of an elastic stocking in treating varicose veins in a 23-year-old woman with Klippel–Trenaunay syndrome.5 However, these stockings, made exclusively from rubber threads, were uncomfortable. It was not until Jonathan Sparks patented a method for winding cotton and silk around the rubber threads that elastic stockings became comfortable and popular.3
Mechanism of Action
Edema
By increasing the tissue pressure, compression works against filtration, which is the basis of both prevention and removal of edema. Occupational leg swelling in sitting and standing professions can be prevented by light compression stockings,6 which are also able to reduce mild edema.7,8 Reduction in intradermal edema has been measured with 20-MHz ultrasound in patients with chronic venous insufficiency (CVI) and lipodermatosclerosis.9 Application of class I or II graduated compression stockings decreased dermal edema by 17% in 4 days, with no statistical difference between the two classes of compression. However, severe stages of limb swelling benefit more from compression devices exerting higher pressure.
Compression may also exert beneficial effects in nonphlebologic causes of edema, such as inflammatory edema (arthritis, cellulitis), cardiac edema, dysproteinemic edema, renal edema, lymphedema, and cyclic idiopathic edema.10A study by Arpaia et al11 showed an improvement in the quality of life (QOL) in patients with chronic CVI who wore class I graduated compression stockings.
Lymph drainage
Several beneficial mechanisms of compression therapy on the swollen extremity may be explained by its effects on the lymphatic system:12
One mechanism of central importance is the restriction of capillary filtration, which corresponds to the amount of the lymphatic load. With compression, the skin and dermal tissues are in closer contact with the superficial capillary network, which is otherwise separated by a pericapillary halo of protein-rich edema fluid.14
Compression removes more water than protein from the tissue, thereby increasing oncotic tissue pressure and reinforcing the need for sustained compression. Therefore, in chronic edema, success is dependent on continued compression.15
Compression together with movement enhances the contraction of the lymphatic system. Olszewski was able to demonstrate that both compression and exercise stimulated the movement of stagnating lymph through the lymph collector in lymphedema patients, in which the lymphatic trunks were filled.16,17 This is probably one explanation for the reduction in intralymphatic hypertension obtained by complex decongestive therapy, as demonstrated by Franzeck and co-workers by lymph capillary pressure measurements.18
Intermittent pneumatic compression enhances prefascial lymph drainage.15 Unna boots are able to increase subfascial lymph transport, which is reduced in post-thrombotic syndrome.19 Consequent compression leads to a morphologic improvement of pathologic initial lymphatics in patients with lipodermatosclerosis, which can be demonstrated by indirect X-ray lymphography (Fig. 6.2).20
Venous system
Depending on the exerted pressure and the body position, external compression is able to narrow or occlude superficial and deep leg veins.21 In the supine position, an external pressure of 10 to 15 mmHg is enough to decrease the venous diameter. This results in an increase in blood flow velocity, as shown by measuring the circulation time with isotopes,22 and is the rationale for recommending light compression stockings for thromboprophylaxis in bedridden patients. A graduation in pressure (18 mmHg at the ankle, falling to 8 mmHg at the thigh) leads to a significantly increased velocity in the deep femoral vein flow.23
In the upright position, such low pressure will have only a minimal effect on decreasing the diameter of the leg veins.24 However, a very small decrease of venous diameter will result in an over-proportional decrease of the local blood volume, as demonstrated by several plethysmographic studies.25–32 Stockings with an ankle pressure of around 20 mmHg have been shown to improve the venous pump.25,30,31 Elastic compression stockings with as little as 8 mmHg pressure have also been found to significantly reduce symptoms of CVI in patients during daily work activity.33–35
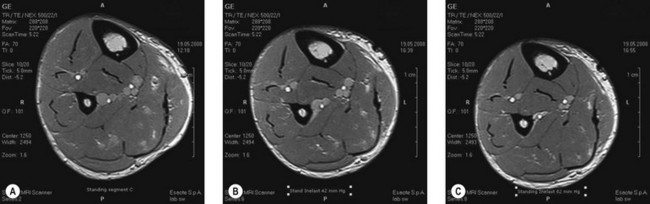
Bandages may provide much higher pressure in the upright position. Magnetic resonance imaging (MRI) is able to show that, during standing, deep veins will be narrowed by an external pressure of 42 mmHg and nearly occluded by a pressure of 82 mmHg (Fig. 6.3). During ankle movements and walking with stiff bandages, pressure peaks of this magnitude will therefore lead to an intermittent occlusion of the veins (Fig. 6.4). Such high pressure may be tolerated only with inelastic (not with elastic) material.
The compression pressure when starting walking counteracts the lateral expansion and dilation of leg veins during muscle contraction by encasing the veins in a semirigid envelope.36,37
The application of an external pressure with a blood pressure cuff blown up to 40 to 60 mmHg to various portions of the leg containing incompetent valves led to an abolishment of reflux.38,39 This effect was directly associated with a decreased vein diameter. Reduction of venous refluxes and improvement of ambulatory venous hypertension by external compression could be demonstrated even in patients without any valves (avalvulia), indicating that this effect is not necessarily explained by coaptation of distended valve leaflets but rather seems to be due to increasing the resistance to retrograde flow.40 Increasing external pressure in the upright position increases the ejection fraction of the calf muscle pump function.41
Conflicting results have been reported concerning an improvement in ambulatory venous hypertension by using compression stockings.36,42 One study showed a significant decrease of such hypertension with short-stretch bandages applied with a resting pressure on the distal leg of more than 50 mmHg, but not with elastic compression stockings exerting a pressure of 30 to 40 mmHg.37 This may be explained by the fact that inelastic, short-stretch bandages lead to an intermittent short venous occlusion during the muscle systole while walking. In patients with venous ulcers due to deep venous incompetence, short-stretch bandages are able to impede venous refluxes more effectively than are elastic stockings exerting the same resting pressure.43 Patients with severe stages of CVI benefit more from high compression pressure, whereas lower pressure is sufficient for milder stages such as varicose veins.44
To achieve complete occlusion of superficial veins, the external pressure should be higher than the intravenous pressure, and this depends on the body position. It was shown that occlusion of the leg veins can be obtained with an external pressure in the range of 20 mmHg in the supine position, but that in the sitting and standing positions the pressure has to be between 50 and 70 mmHg.21 With compression stockings, such pressure ranges can only be achieved when rolls or pads are applied over the vein, thereby increasing the local pressure by reducing the local radius (law of Laplace, see later). Such rolls may be especially useful if local compression over treated veins on the thigh is intended.45
Microcirculation
Compression accelerates blood flow in the enlarged capillary loops and reduces capillary filtration due to enhanced tissue pressure. Improvements are seen in normalization of venular flow, volume, and velocity, improved distribution of microcirculation blood flow, and normalization of leukocyte adhesion.46–52 Different studies using electron microscopy were able to show a restoration of the structural changes in the media myocytes in stripped veins53 and a tightening of intercellular junctions.54 Laser Doppler flux measured a 29% increase in blood cell velocity in patients with CVI and lipodermatosclerosis.49 Increasing flow velocity may reduce the likelihood of white blood cells interacting or sticking to endothelium with release of various factors. Effects on mediators involved in the local inflammatory response may explain both the immediate pain relief that occurs with good compression and ulcer healing.55
Studies in patients wearing class II graduated compression stockings demonstrate an improvement in skin microcirculation in as little as 1 week, with near normalization of the functional state of microcirculation becoming apparent by day 30.52 Model experiments with intermittent pneumatic compression were able to demonstrate that there is an increased release of the endothelial relaxing factor (EDRF) nitrogen oxide from the endothelial cells, depending on the amount of shear stress produced by the compression waves.56
Compression tightens the junctions between the endothelial cells of capillaries57 and reduces pro-inflammatory cytokines in venous leg ulcers.58
Arterial flow
A reduction of arterial flow may be expected when the external compression pressure exceeds the intra-arterial pressure. This may happen in patients with arterial occlusive disease with a reduced peripheral arterial pressure. In order to avoid ischemic skin lesions from external compression, therefore, it is essential to measure the peripheral arterial pressure using a Doppler probe before strong compression bandages or stockings are applied. It is generally accepted that a Doppler ankle–brachial index (ABI) of less than 0.5 is a contraindication for sustained compression. However, external compression does not invariably mean reduction of arterial flow.59 Mayrovitz reported on several experiments concerning arterial blood flow and compression60–62 and was able to demonstrate an increase of the pulsatile flow below the knee in healthy volunteers using nuclear magnetic resonance flowmetry.60 He also demonstrated a reduction in toe blood perfusion, which was greater with increased compression, but not of sub-bandage skin perfusion.
Patients with edematous legs and with an ABI of between 0.5 and 0.8 may benefit from inelastic or short-stretch bandages applied with a mild resting pressure, due to the edema-removing massage effect that will occur with every ankle movement (see later). Completely inelastic bandages, together with walking, have a similar effect as intermittent pneumatic compression. The rhythmic pressure peaks of an inelastic bandage during walking can be compared with those exerted by an intermittent pneumatic pressure pump. Several experiments with intermittent pneumatic compression have demonstrated an increase of arterial flow in patients with arterial occlusive disease.63–68 The decisive mechanisms of action are the reduction of edema, an increase of the arteriovenous pressure gradient, myogenic mechanisms, and the release of vasoactive substances from the endothelial cells.
Basic Principles of Compression
Terminology
A confusing variety of partly overlapping terms can be found in the literature:1,69–79 Only terms of practical importance are listed here:
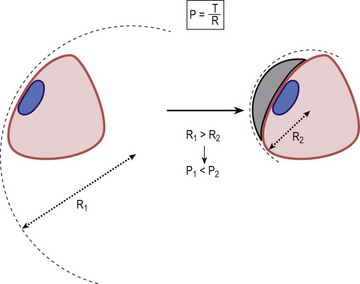
Compression pressure and Laplace’s law
The compression pressure (Pascal) is defined by the force (Newton), which is exerted to an area of 1 m2 (Fig. 6.6). The tension in a bandage is determined by the force applied to the fabric during application.
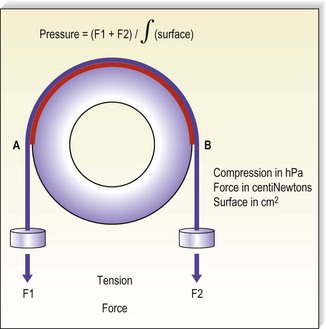
Figure 6.6 The pressure generated by an inelastic bandage is determined by the tension of the fabric.
(Courtesy Bernard Lun, Ganzoni, St Just, France.)
From Figure 6.6 it is clear that the curvature of the leg plays a deciding role for the exerted pressure. If the cylinder in the model was replaced by a cube, the pressure over the flat areas would be zero, while it would be very high along the sharp edges of the cube. This is described by Laplace’s law stating that the pressure (P) is directly proportional to the tension (T) of the bandage but inversely proportional to the radius (R) of the curvature to which it is applied (Fig. 6.7):
Practical consequences of Laplace’s law
In general, pressure is calculated for the circumference of the limb at a specific level. Because the leg has an irregular cross-section that is not circular, the applied point pressures vary at different locations around the leg. Using Laplace’s formula, it is evident that the effective pressure is greatest at the point of minimum radius and least at the point of maximum radius. Thus, when a stocking is applied, the anterior aspect of the leg receives the greatest amount of pressure, and the lateral and medial sides of the leg receive the least compression pressure. This is especially important in the malleolar area, where the lowest degree of compression occurs, because the medial and lateral surfaces are flat or hollow, the local radius being ‘negative’ (Fig. 6.8). If there is a venous ulcer situated in the dip behind the malleolus, the only way to bring compression to this region is to put a pad over that area (Fig. 6.9). The reduction of the local radius by pads or rolls in order to increase local pressure has been termed ‘positive eccentric compression’.1
On the other hand, tendons and bony prominences are susceptible to a high compression pressure and should therefore be protected under a bandage by decreasing the radius using a cotton wool inlay. The enlargement of the local radius has been termed ‘negative eccentric compression’.1
Measurement of compression pressure
Laboratory measurements of compression stockings
The effects of compression depend widely on the exerted pressure, which should be adapted to the underlying condition. Basically, the pressure of a stocking is calculated from the force–extension diagram of the elastic fabric on a wooden leg model with defined circular cross-sections using Laplace’s formula (Fig. 6.10). The range of the compression pressure indicated by the manufacturers is determined by the measurement of the force which is necessary to stretch the stocking at certain leg levels (B, B1, C, D, F, G) in a transverse direction. The proportion of stretch and force for each circumference level, which corresponds to the steepness of the so-called slope in the hysteresis curve, reflects the elasticity of the material of the stocking.
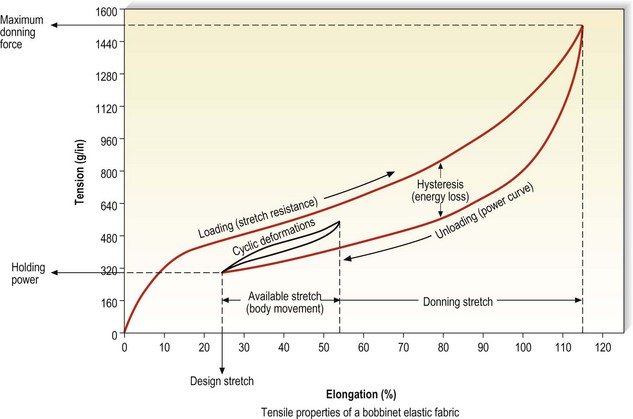
Figure 6.10 Hysteresis curve generated by a bobbinet elastic fabric.
(Courtesy of Beiersdorf-Jobst, Charlotte, N.C.)
Measuring points, lengths, and girths defined by the European standardization proposal (CEN, Centre Européen de Normalisation)69 are shown in Figure 6.11.
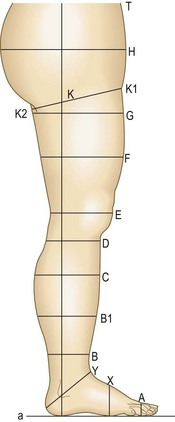
Figure 6.11 Measuring points, lengths, and girths on the human leg. Note: measurements should be taken of the patient’s leg in a standing position.69
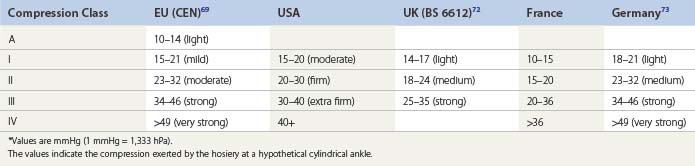
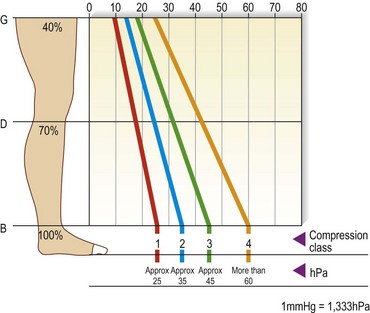
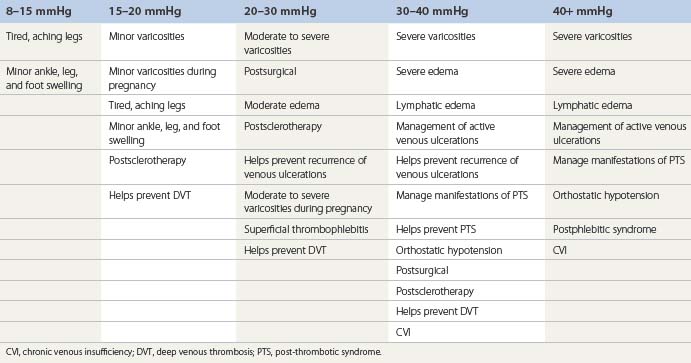
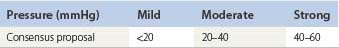
Table 6.1 gives a comparison of compression classes for ready-to-wear and custom stockings used in several countries. The range of compression pressures, and also the verbal description of these classes, are amazingly variable from one country to another. Additionally, it is important to realize that the given ranges are measured by different methods, so comparisons are problematic. These facts underline the necessity of in vivo pressure measurements on the individual leg, at least in future clinical studies. For a better universal understanding, it is recommended to use the pressure range in mmHg rather than compression classes in general.
The pressure values in Table 6.1 refer to level B. The European prestandard69 defines the ranges of pressure profiles in comparison with the pressure at the smallest leg circumference (position B) as follows: for level B1 70% to 100%, for C and D 50% to 80%, and for F and G 20% to 40% for compression classes III and IV; 20% to 60% for compression classes A and I, and 20% to 50% for compression class II (Fig. 6.12). The producers of compression stockings recommend adjusting the compression class according to the clinical severity.
There is no American standard. Table 6.2 gives an example as recommended by one company (BSN-Jobst, Charlotte, N.C.).
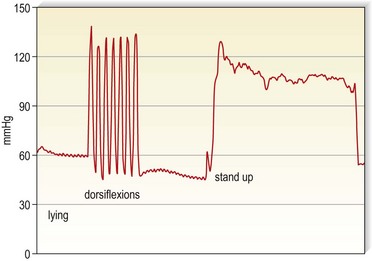
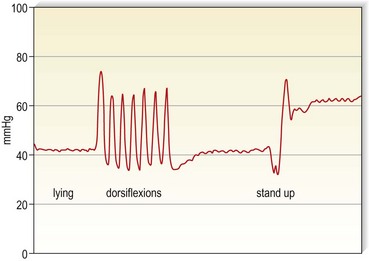
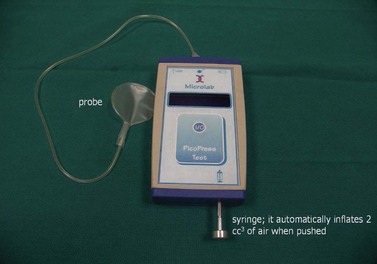
Measurements of interface pressure on the leg
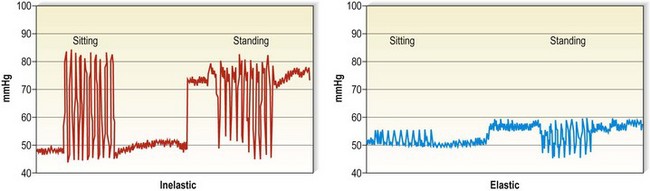
Several instruments are available, which should be calibrated on the leg according to a recent consensus recommendation.81 In this consensus paper, some prerequisites of an ‘ideal’ pressure sensor are summarized. One location that should always be included in future pressure measurements is B1. This is where the tendinous part of the gastrocnemius muscle changes into the muscular part, showing the most pronounced protrusion of the tendon and the most extensive enlargement of the leg circumference during dorsiflexion or by standing up from the supine position. Whenever in vivo measurements of interface pressure are performed, it is essential to indicate the exact measuring point, the main specifications of the instrument, including the dimensions of the probe, and the body position in which the measurements have been performed. Figure 6.13 shows a pressure measuring instrument which allows continuous pressure registration. The flat probe is inflated only when pressure is measured and can stay on the leg for several days. Figures 6.4 and 6.5 show pressure curves obtained with this instrument.
Resting and working pressure
Some probes allow measurements of interface pressure not only at rest but also continuously during movement. Figure 6.14 shows an example where the interface pressure on the distal leg was measured continuously in different body positions, both for an inelastic and for an elastic bandage. Starting with comparable resting pressure for both bandages, the inelastic bandage has a higher working pressure than the elastic bandage. This difference has a major impact on the efficacy of the compression device concerning edema reduction and improvement of venous pump. Stockings with high stiffness or slope value, even at the same compression level, are better for patients with edema from CVI or other causes.82 Inelastic bandages are more effective to reduce venous refluxes and ambulatory venous hypertension.37,43
Measurements of intramuscular pressure have shown higher resting pressure with elastic than with inelastic material, suggesting that elastic compression applied over a long period in the recumbent posture may impede microcirculation and jeopardize tissue viability.83
Measurement of stiffness
Stiffness is defined as the increase in compression per centimeter increase in the circumference of the leg, expressed in millimeters of mercury per centimeter.69 This parameter characterizes the distensibility of a textile as well as the elastic property of a composite bandage, which plays an important role concerning the performance of a compression device during standing and walking. Stiffness may be measured in the laboratory, where it corresponds to the slope of the hysteresis curve. The fact that it can also be assessed by in vivo measurements on the individual leg will certainly achieve increasing practical importance in future trials.80,81,84
Measurement of dynamic stiffness during walking requires sophisticated instrumentation and can therefore not be used in routine clinical practice.80 In order to obtain valuable information on the elastic property of a compression device, which may be quite complex when several materials are combined, the so-called ‘static stiffness index (SSI)’ may be a useful alternative.79 A calibrated pressure sensor is fixed to the medial aspect of the leg at B1. This is the area which will show the most extensive changes in local curvature and leg circumference when the body position is changed between supine and standing. The difference between the interface pressure in the standing and in the lying position, called SSI, is a valuable parameter for the stiffness of the compression system, which determines the relationship between resting and working pressure. As is shown in Figure 6.15, inelastic material produces a much higher pressure increase in the upright position than elastic material. It is important to note that different indices may be obtained with different sensors. Therefore, reliable comparisons of different compression devices will only be possible by testing using the same sensor on the same site.
It has been shown that different padding materials may change the stiffness of the final bandage.84
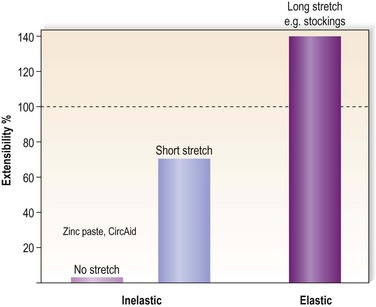
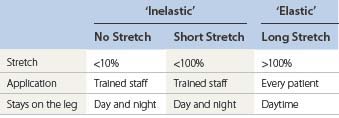
Compression Material
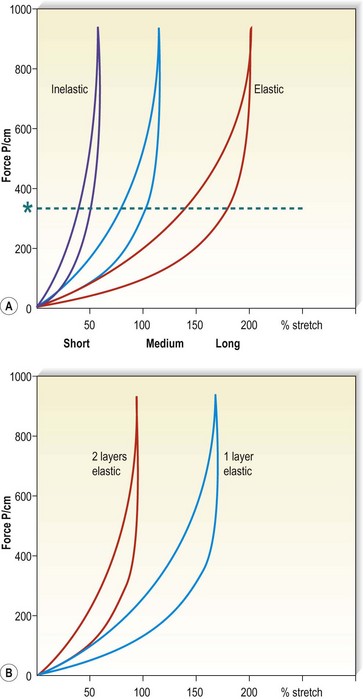
Different devices/materials are available for compression therapy (Box 6.1). The main categories of compression concerning the elastic properties of the materials are summarized in Table 6.3. Extensibility is the ability of a bandage to increase in length in response to an applied force.
Compression bandages
There are three basic types of bandages: completely nonelastic bandages, virtually without any stretch, e.g. Unna’s boot or Velcro-band products; short-stretch bandages (<100% extensibility); and long stretch (>100% extensibility) (see Table 6.3).
No-stretch and short-stretch material is frequently called ‘inelastic’ and long-stretch material ‘elastic’ (Figure 6.14).
Standards for compression bandages
There is currently only the British standard, (BS) 7505:1995, for compression bandages. It contains four categories of compression bandages,72 which are summarized in Table 6.4.
Table 6.4 Classification of compression bandages by British Standard72
| Bandage Type BS 7505 | Level of Compression | Pressure British Standard (mmHg) |
|---|---|---|
| 3A | Light | Up to 20 |
| 3B | Moderate | 21–30 |
| 3C | High | 31–40 |
| 3D | Extra high | 41–60 |
By definition, the indicated pressure levels should be achieved on an ankle 23 cm in circumference, when applied with a 50% overlap. This classification was constructed entirely based on in vitro measurements and does not correspond to the clinical reality, according to which the resulting pressure of a bandage mainly depends on the sretch during application and far less on the material. Only a few measurements of compression pressure on the human leg have been reported, applying different materials with light, moderate, and high strength.85 It could be demonstrated that the interface pressure of a bandage on the human leg was, on average, one class higher compared with the values in Table 6.1 for compression stockings. Even with intentionally very loose bandaging in an attempt to achieve ‘light compression’, the pressure of the 5-m-long bandage, short stretch and long stretch, was always higher than 20 mmHg with one bandage and higher than 30 mmHg with a multilayer technique.
Because of these dicrepancies, new proposals concerning a bandage classification were made in a consensus conference based on practical measurements in vivo.70 The eponym ‘PLACE’ was proposed, containing the main characteristics to be considered when compression bandages are applied: P stands for pressure, LA for layers, C for components and E for the elastic property of the single bandage used. Table 6.5 shows the definition of different pressure ranges. Bandages are always applied with some overlap so that one layer bandages do not exist. The only one layer system is a compression stocking. Actually, the so-called four-layer bandage is applied with much more than four layers and should correctly be called a ‘four-component bandage’ since it contains four different bandage materials. It was proposed to use the terms ‘elastic’ and ‘inelastic’ only for single bandages based on their elastic properties, but not for a final bandage consisting of different single bandages. In fact, the elastic property of the final bandage cannot be predicted based on the elasticity of the single components. Adding several bandages does not only increase the sub-bandage pressure but enhances the stiffness of the final bandage as well.
Inelastic and short-stretch bandages
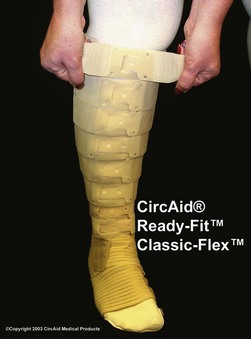
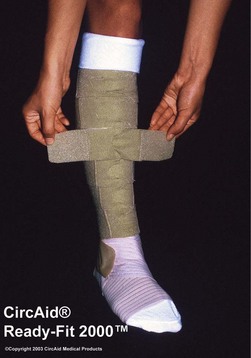
Bandages with an extensibility close to zero, such as zinc paste (Unna boot) and rigid Velcro-bands like Circ-Aid (CircAid Medical Products, San Diego, Calif.) or Hydroboot, (Incappe Inc, Brandon, Miss.) are examples of completely nonelastic material. Nonelastic bandages must be applied with skill and some knowledge. If light compression is indicated they should be applied without extension of the fabric by moulding the material to the leg without tension. When strong compression is indicated, completely rigid zinc paste bandages need to be applied with full extension of the material and adjusted to the configuration of the leg. Figure 6.16 shows a bandage applied with zinc paste on the lower leg, wrapped over with a short-stretch bandage and with adhesive bandages over the knee and thigh of a patient with a proximal deep vein thrombosis (DVT).
Short-stretch bandages can be extended 30% to 100% and should be applied with a pressure of more than 50 mmHg on the distal leg if strong compression pressure is indicated. Due to an immediate removal of edema, this pressure will fall down to pressure values which are also well tolerated in the supine position. After some hours they have a low to slight resting pressure but still a high and very effective working pressure. Short-stretch bandages exert little pressure when the calf muscles are relaxed but prevent expansion in calf diameter when the muscles are contracting during standing and walking (‘high working pressure’). They are, therefore, comfortable when patients are recumbent, and they act to decrease venous pressure with ambulation.37 The main disadvantage is that they may become loose after a few hours of wear, especially when applied too loosely. In immobile patients, correctly applied short-stretch and inelastic bandages are even more effective than long-stretch material. Even minimal toe movement or passive ankle mobilization performed by physiotherapists will produce a much higher massaging effect compared to elastic material.
Stiff bandage material is not easy to handle. Most untrained persons apply inelastic bandages with too low a pressure. In order to obtain a resting pressure on the distal leg of about 40 mmHg, the initial pressure after application should reach about 60 mmHg. As can be seen from the example in Figure 6.17, the resting pressure in the supine position drops from 70 mmHg to 50 mmHg after 2 hours. This pressure exerted by an inelastic bandage is also well tolerated during night time. However, there is less pressure loss in the standing position, so an effective range of pressure values is still maintained after 24 hours (see Fig. 6.17). Especially in the first days after bandage application, the reduction of swelling may be so pronounced that the bandages will get loose and have to be renewed. When edema reduction is stabilized, inelastic bandages may stay on the leg for several days.
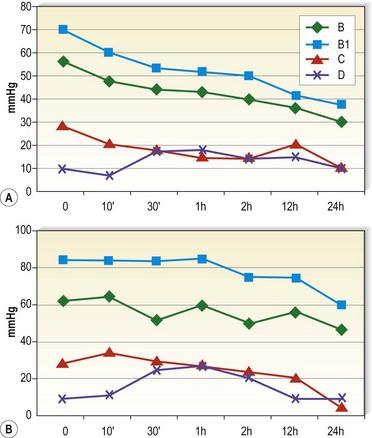
Figure 6.17 Interface pressure exerted by a multilayer short-stretch bandage (Rosidal sys, Lohmann) measured by an MST tester119 on the medial leg in the supine (A) and in the standing position (B). Measuring points: B = behind the inner ankle, B1 = 8 cm above, C = 19 cm above, D = 27 cm above the ankle. The pressure drop of this multilayer short-stretch bandage is more pronounced in the supine than in the standing position.
A study of elastic, minimal-stretch, and nonelastic orthoses (CircAid), demonstrated that 4 hours after application, elastic bandages had 94% of their initial pressure, compared with 70% for minimal-stretch and 63% for the nonelastic orthoses.86 In the supine position, the decrease at 4 hours was 72% for elastic, 59% for minimal-stretch, and 44% for nonelastic compression. One of the advantages of this particular orthosis is the fact that it can be readapted by the patient when it gets loose (Figs 6.18 and 6.19). Smaller but significant decreases in pressure under short-stretch bandages were also found in studies on changes in pressure with exercising.87,88 Measurement of compression after walking for 3 hours and then again 7 days later showed a decrease in pressure from 80.5 mmHg to 43.6 mmHg after 3 hours and to 26.3 mmHg after 7 days. In this study, Comprilan (Beiersdorf, Germany) with an extensibility of 70% was used.87 In the second study, elastic bandages did not demonstrate a similar degree of compression loss after tip-toe exercise.88 Although the authors speculate that the loss in pressure during exercise may be related to application technique of the short-stretch bandage with a maximum tension of 45% (Compridur, Beiersdorf, Germany), this could also be explained by an immediate volume reduction of the leg as shown in healthy volunteers and in lymphedema patients (Rosidal sys and Rosidal Lymphset, Lohmann & Rauscher, Germany).89
When the bandage gets loose, it should be renewed in order to prevent refilling of the extremity with edema and to avoid tourniquet effects from the down-gliding compression material. In patients with lymphedema who are best treated with short-stretch bandages in the initial phase, this may be necessary once a day.90
Elastic, long-stretch bandages
Long-stretch bandages can be extended 140% to 200% and thus have a high resting pressure; that is, they exert pressure on the superficial venous system when the limb is at rest with a decreased working pressure as compared with short-stretch bandages (see Fig. 6.15). Because of their intrinsic high resting pressure, they can damage arterial, lymphatic, and venous flow if not applied carefully, so they are best used while patients are ambulatory. Their advantage is that they may be more easily molded around the heel and ankle and can sustain their pressure better than inelastic bandages.
Multilayer bandages
In the above-mentioned consensus paper it is stated that ‘multilayer bandages’ are actually multicomponent bandages consisting of different materials for padding retention and compression.70
From these definitions it is quite obvious that many combinations of different materials are possible, which will lead not only to an increasing pressure with each layer but also to variable elastic properties of the final bandage. In a comparative trial with different brands of four-layer bandages it was found that, in fact, a bandage applied as part of a multilayered system achieves only about 70% of the pressure that it exerts when applied alone, thus challenging the commonly held assumption that the final pressure achieved by a multilayer bandaging system is the sum of the pressures exerted by each individual layer.91 The elastic property of the final bandage will change toward a more inelastic bandage due to the friction of several layers, so that it can also be tolerated in the supine position92 (Fig. 6.20). One example is the so-called four-layer bandage which consists of several components of different material (wool, crepe, elastic and self-cohesive) and which may be worn day and night (Profore, Smith & Nephew, Hull, UK).
It had been claimed that such bandages have not lost pressure at 1-week follow-up.93 Actually some of our own measurements revealed a pressure loss starting immediately after application which is less pronounced compared to short-stretch bandage systems.
One study compared eight different compression bandages under standardized conditions.92 Multilayer bandage systems composed of short and medium stretch bandages exhibit the smallest pressure loss with patient activity and have a significant pressure decrease when the patient is supine. These systems gave better postural and interface pressure changes than all types of single-layer bandages, obviously due to an increase of the stiffness of the final multilayer bandage.79,85
There are also multilayer systems consisting of short-stretch material, which are equally effective in ulcer healing when applied correctly.94,95 Examples are the Pütter bandage (Hartmann, Germany), Rosidal sys (Lohmann & Rauscher, Germany), the adhesive Actico bandage (Activa Healthcare, UK), the Coban 2 bandage (3M, Minnesota, USA) and the Fischer bandage, consisting of a tightly applied Unna boot with a short-stretch bandage on top. This latter bandage was recommended by Heinrich Fischer, the pupil of Unna, in 1910 for the treatment of DVT4 and is still one of the author’s favorites in patients with DVT, post-thrombotic syndrome, or venous leg ulcers (see Fig. 6.16). The tradition of using multilayer short-stretch bandages is rather restricted to central European countries and to the Netherlands, while many bandagers in the UK are more familiar with multilayer systems containing rather long-stretch material.
Several trials have compared multilayer long-stretch bandages with short stretch, some showing better results with the short stretch,94,95 some with long-stretch multilayer systems.96,97 Frequently unfair comparisons have been made comparing properly applied versus inadequately applied bandages. In future trials, sufficient training of the bandagers should be provided for both systems and interface pressure and stiffness should be measured.
The principle of applying several compression layers over each other is also a promising concept for elastic stockings, with regards to an increase in both compression pressure and stiffness.98,99
Training in the application of bandages
A major drawback of bandages is their non-uniform application. A comparison of the range in pressures measured during application of a long-stretch elastic bandage by skilled nurses versus nursing students demonstrated that the skilled bandager’s pressure ranged from 25 to 50 mmHg, and the unskilled bandager’s pressure ranged from 15 to 70 mmHg.100
A recent study checking the sub-bandage pressure showed that especially nurses with long professional experience tend to apply short-stretch bandages much too loosely (< 20 mmHg) and that this can be greatly improved by training.101
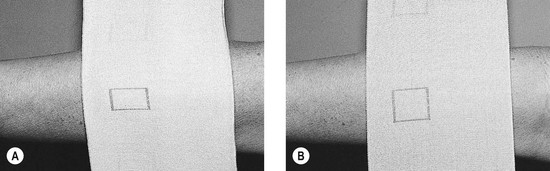
Several elastic bandages are marked with geometrical figures, such as a rectangle that becomes a square when stretched to the proper length (e.g. Setopress, Seton Healthcare Group, Oldham, UK; Proguide, Smith and Nephew, UK; Velpeau, Lohmann & Rauscher, France) (Fig. 6.21). Setopress was studied in five skilled nurses and five unskilled assistants, who also applied an Elastocrepe (Smith and Nephew, UK) bandage to the opposite leg. The Setopress bandage applied by experienced nurses most closely approximated target sub-bandage pressures whereas the unskilled group differed significantly among themselves. As before, both groups differed significantly in applying sub-bandage pressure with the Elastocrepe bandage, with a significant difference noted between the skilled nurses and unskilled bandagers.102 An additional study of 18 nurses applying an adhesive compression bandage showed 10 nurses producing a tourniquet effect, 5 producing inadequate ankle pressure, 2 excessive ankle pressure, and 1 appropriate ankle pressure but with an improper gradient in the calf.103 Training significantly improved performance. Another study of 48 trained community nurses that compared one inelastic and two elastic bandages showed similar results.104 The most common problem was production of a calf tourniquet.
In addition, even with physicians who are experts in applying bandages, a true graduation in pressure may not always be obtained. One study of five surgeons showed a range of 21.9 to 52.7 mmHg with application of a short-stretch bandage, with each individual surgeon having a range of 10 to 20 mmHg between bandage applications.105 The coefficient of variation in each individual ranged from 9.9% to 25.2% with a mean (standard deviation) of 17.0 (4.9%).
Based on the information just presented, it is obvious that training in the application of bandages is very important.101–107 This is especially true for inelastic bandages, which should be applied with a higher initial pressure compared to elastic material. Instruction of compression application with the use of interface pressure measurement has been shown to improve technique.107 In teaching 156 persons at a wound healing course, the application of appropriate interface pressures required approximately 10 exercises with the use of interface pressure transducers.
Important points to consider when applying a bandage are:
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree