CHAPTER 12 Clinical Methods for Sclerotherapy of Telangiectasias
Historical Review of Techniques
Sclerosing treatment for telangiectasias was ignored until the 1930s when Biegeleisen1 injected sclerosing agents intradermally or subcutaneously into the general area of capillary enlargement. However, this procedure caused severe necrosis and lack of effect on the telangiectasias. Biegeleisen then developed and popularized a method of ‘microinjection’ of telangiectasias with sclerosing agents through the use of an ‘extremely fine metal needle’ (later described as a handmade 32- or 33-gauge needle).2 Unfortunately, he used sodium morrhuate in the treatment of these fragile small vessels, which produced multiple complications, including pigmentation, cutaneous necrosis, and allergic reactions. Thereafter, sclerotherapy treatment of leg telangiectasias was thought of disparagingly by most practitioners3 until the 1970s when Alderman,4 Foley,5 Tretbar,6 and Shields and Jansen7 published reports of procedures that had achieved excellent results with few adverse sequelae. In these procedures, solutions less caustic to the telangiectasia were used – hypertonic saline (HS) with or without heparin and lidocaine (15% to 30%), and sodium tetradecyl sulfate (STS) 1% – as were techniques that ensured accurate placement of the solution into the blood vessels (use of 30-gauge needles).
Indication
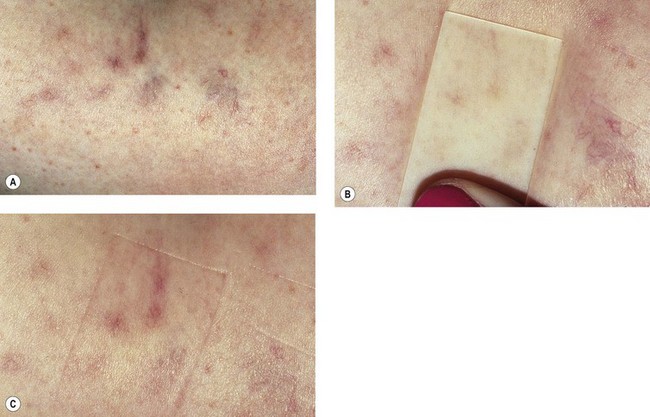
Microsclerotherapy is theoretically indicated for any small telangiectatic vessel or venule on the cutaneous surface. Best results are obtained on superficial linear or radiating vessels on the lower extremities. Telangiectasias on the face are less reliably responsive to microsclerotherapy because they probably have more of an arteriolar component and result from active vasodilation, but they can be treated successfully (see Chapter 4).8,9 In addition, bright-red telangiectasias on the leg that have a rapid refilling time after diascopy (applying pressure with a glass slide) with the patient recumbent (Fig. 12.1) are probably also supplied through arteriolar flow (see Chapter 3).10 These vessels are relatively recalcitrant to usual therapy and tend to recur after treatment. More importantly, these arteriolar leg veins are more likely to develop overlying cutaneous necrosis if sclerosing solutions reach the arteriolar feeding loop (see Chapter 8). They may be more effectively treated with the pulsed dye laser or intense pulsed light sources (see Chapter 13).
The description in Chapter 9 of the injection of varicose veins by first closing off the high-pressure reflux points with sclerosing solution, followed by sclerotherapy of remaining abnormal vessels, forms the basis for the rationale of compression sclerotherapy of varicose veins. The treatment of ‘spider’ leg veins should be just as rational.
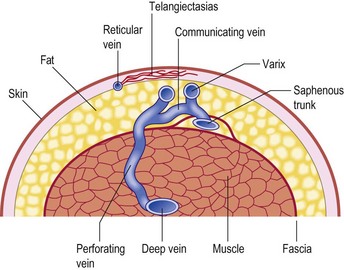
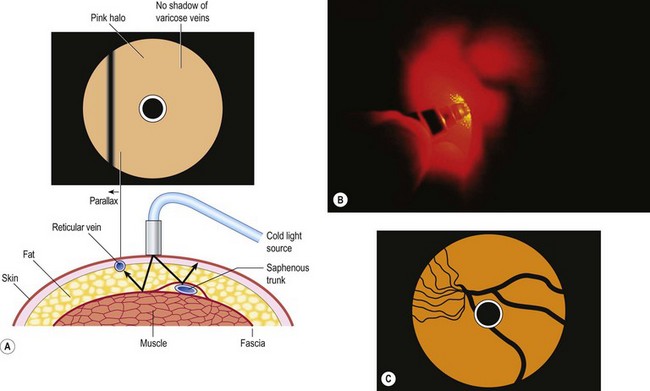
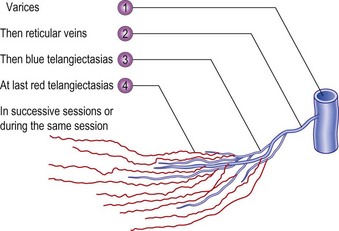
In the vast majority of cases, spider veins connect to underlying varicose veins either directly or through tributaries (Fig. 12.2) (see Chapter 3).11–13 This is typical on the lateral aspect of the thigh when the lateral network described by Albanese is visible (Fig. 12.3). Doppler examination shows that almost all visible blue reticular veins are connected to telangiectasia.14,15 Transillumination shows exactly the same pattern (Fig. 12.4). Therefore, as with varicose veins, treatment should be directed first at ‘plugging’ the leaking high-pressure outflow at its point of origin (Fig. 12.5). An appropriate analogy is to think of spider veins as the ‘fingers’ and the feeding varicose or reticular vein as the ‘arm’. Treatment should first be directed to the feeding arm and then, only if necessary, to the spider fingers. Mariani et al16 found that when telangiectasias were treated in this manner, 3-year follow-up of 109 patients showed enduring resolution of telangiectasias in 95%.
There are a number of advantages to this systematic approach to sclerotherapy. When sclerotherapy is performed in this manner, the spider veins often disappear without direct treatment, or decrease markedly in size, thus limiting the number of injections into the patient. The larger feeding vein is both easier to cannulate and less likely to rupture when injected with the sclerosing solution, thus minimizing the extent of extravasated red blood cells (RBCs) and solution. Theoretically, this method also should minimize the postsclerotherapy development of hyperpigmentation, cutaneous necrosis, telangiectatic matting (TM), and recurrence (see Chapter 8).
Injection Technique
Preinjection procedure
After a physical examination, including the use of noninvasive diagnostic techniques when appropriate (see Chapter 5), the patient is scheduled for a sclerotherapy session and given a questionnaire (Appendix C), consent form (Appendix D), and instructional material (Appendix G) to read and complete at home. Questions about the procedure are answered, and all reasonable and appropriate complications and adverse sequelae are addressed. An estimate of the approximate number of treatment sessions and the cost of treatment is given in writing to prevent any future misunderstandings. Insurance reimbursement policies are discussed and documented. Documentation of the relief of symptoms with compression stockings is helpful in gaining preauthorization of treatment from insurance companies, but in most cases insurance companies decide on the medical necessity for treatment based on the size (diameter) and type of vessel, not symptoms. If graduated compression stockings are planned to be applied after treatment, they are fitted at this time and given to the patient to wear before treatment. If the stockings produce a resolution of symptoms, the physician can assume that successful sclerotherapy will give the same result. In addition, wearing the stockings before treatment helps answer any questions about their fit to ensure they will be worn for the prescribed length of time after treatment.
With the patient standing on an elevated platform or stool, a complete set of photographs of the legs is taken from four different views, and the individual areas that will be treated are photographed up close (Fig. 12.6). Reticular veins and telangiectasias are photographed with the patient recumbent. Photographic documentation is important because patients frequently cannot remember exactly how their legs appeared before treatment. Any pretreatment pigmentation irregularities and scars may be blamed later on the sclerotherapy treatment, since patients usually look more closely at their legs once treatment has begun. In addition, when patients return in a few years with additional veins and telangiectasia, viewing pretreatment photographs will allay concerns regarding the possibility of unsuccessful previous treatment.

Figure 12.6 Standard photographs taken before treatment begins to allow accurate determinations of treatment outcome. Four standard views are taken at an F-stop of F8; close-up views are taken at an F-stop of F11, with macro-close-ups taken at an F-stop of F16. All photographs are taken with Kodachrome ASA 64 film as described in Chapter 15. A, Frontal view. B, Rear view. C, Right side (the right foot is always in front of the left foot). The right knee is slightly bent so the left inner thigh is better visualized. D, Left side (again with the right foot in front of the left). E, Documentation of scar from previous treatment for a verruca on the right anterior tibial area, which could later be thought of as a treatment scar. F, Documentation of dermatofibroma on the right medial knee area, which later could be thought of as punctate pigmentation from treatment. G, Close-up view of telangiectasia and venules (0.2–0.6 mm in diameter) on the right lateral thigh, along with pretreatment nonspecific light-brown pigmentation, which could later be thought of as postsclerotherapy hemosiderin pigmentation.
| Gauge | External diameter (mm) |
|---|---|
| 30 | 0.30 |
| 27 | 0.41 |
| 26 | 0.46 |
| 25 | 0.51 |
| 22 | 0.71 |
| 20 | 0.89 |
| 18 | 1.27 |
At the end of the treatment session, the treated areas are recorded on a diagrammatic chart to help check progress at follow-up examinations (Appendix E). Patients are given written postoperative instructions about activity and the disposition of their graduated compression stockings and/or bandages.
Preparation and visualization of the vessels
Microsclerotherapy of spider veins is performed with the patient in the supine position. Gravitational dilation of telangiectasias is unnecessary to minimize intravascular thrombosis. The skin is wiped with alcohol, making the telangiectasias more visible because of a change in the index of refraction of the skin. The glistening effect of alcohol renders the skin more transparent and helps clean the injection site. In addition, alcohol may cause some vasodilation of the telangiectasias. Alternatively, Sadick17 recommended that the skin be wiped with a solution of isopropyl alcohol 70% with acetic acid 0.5%. He found that this solution improves the angle of refraction better than alcohol alone.
Scarborough and Bisaccia18 recommended rubbing a few drops of the sclerosing solution on the skin overlying the venules with a gloved finger. They used polidocanol (POL), which also contains alcohol in water as the diluent. We agree that visualization is enhanced with this technique once the initial effects of the isopropyl alcohol have worn off through evaporation. To further enhance visualization of the vessels, we recommend the use of magnifiers from 2.25× to 5× (see Chapter 15).
Equipment
Needle and syringe
Although visualization of the vessel is important in ensuring proper needle placement, the examiner actually enters the vessel ‘by feel’. This is particularly true in the injection of reticular varices. In this situation it is best to pierce the skin rapidly and advance the needle superficially over the vessel at a slight angle in a ‘double-piercing’ technique. Penetration of the vessel is ‘felt’, even when the examiner uses a 30-gauge needle. Some authors state that the ‘feel’ is enhanced with the use of a 26- or 27-gauge needle but we find this unnecessary.19 In this regard, the use of a glass syringe would best reflect an impedance to flow if a vessel were not properly cannulated. However, glass syringes are more cumbersome to use and regulations regarding sterile technique and other hazards have relegated glass to undesirable. With the availability of high-quality plastic syringes, a good feel can be obtained and the risk of transmitting blood-borne diseases obviated (see Chapter 15).
Ideally, the goal of microsclerotherapy is to cannulate the vessel, injecting sclerosing solution within and not outside of the vessel wall. Usually, a 30-gauge needle suffices for most vessels, although some physicians recommend the use of a 32- to 33-gauge needle to decrease the likelihood of inadvertent perivenular injection in the treatment of the smallest diameter vessels.20–23 The disadvantages of using a 32-gauge needle are that it dulls rather quickly and easily bends away from the targeted vein (see Chapter 15). Boxes of needles sometimes contain individually defectively sharpened and dull needles, which give a ‘scratchy’ sensation to the tip. The physician should never hesitate to change needles if a vein cannot be cannulated easily. It is usually not the ‘tough skin’ of the patient but a dull needle that makes injection difficult.
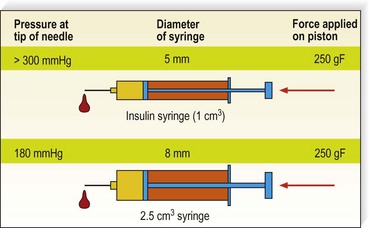
Injecting with a syringe of smaller diameter will increase the pressure of the liquid at the tip of the needle; this may cause more extravasation, more transparietal burn, and may increase the risk for ‘reverse flow’ injection and subsequent necrosis. It has been measured and calculated that for the same force applied to the piston, the pressure can almost double with a small syringe (Fig. 12.7).
One theoretical disadvantage to multiple injections with the same needle is that the needle will become dull.21 However, this was found not to occur on microscopic examination of the needle tips after eight injections into the skin (see Chapter 15).
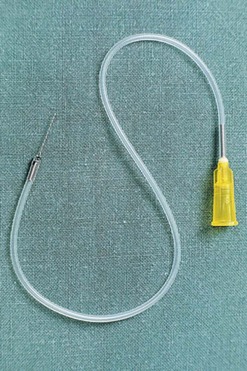
A small vein infusion set designed for sclerotherapy is available in various gauge and tubing lengths with  -inch long needles (Kawasumi Laboratories, STS Pharmaceuticals) (Fig. 12.8). These sets may provide enhanced control for cannulating small veins. In addition, the kink-resistant tubing allows for flow to ensure that the needle is in a vein and not an artery.
-inch long needles (Kawasumi Laboratories, STS Pharmaceuticals) (Fig. 12.8). These sets may provide enhanced control for cannulating small veins. In addition, the kink-resistant tubing allows for flow to ensure that the needle is in a vein and not an artery.
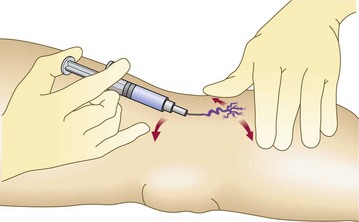
Skin tension
The skin must be taut to facilitate cannulation of the vessel. This can be accomplished with the help of an assistant who stretches the patient’s skin in at least two directions. Alternatively, with proper hand placement, the physician alone can produce three-point tension. Figure 12.9 illustrates the recommended technique for injection. The nondominant hand is used to stretch the skin adjacent to the treated vessel in two directions. Then the fifth finger of the dominant hand exerts countertraction in a third direction. With a little practice, even the most lax skin, such as that on the thighs, can be brought under tension with this technique. Skin laxity varies with patient age, adiposity, and location on the leg.
Depth of injection
The location of most leg telangiectasias is in the upper dermis (see Chapter 1). The most common error in technique is to place the needle tip deep to the vessel. To enter the vessel at a less acute angle almost parallel to the skin surface, the physician should bend the needle to 145 degrees with the bevel up (Fig. 12.10).24 If the needle is not within the vessel, the solution will either leak out onto the skin or produce an immediate superficial wheal. At times, gentle upward traction can be applied as the needle is advanced to ensure superficial placement.
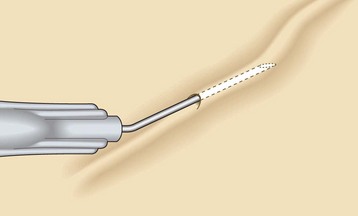
Figure 12.10 Needle is bent to 145 degrees with the bevel up to facilitate accurate insertion into the superficial telangiectasia.
(Reprinted from Goldman MP, Bennett RG: J Am Acad Dermatol 17:167, 1987, with permission from American Academy of Dermatology.)
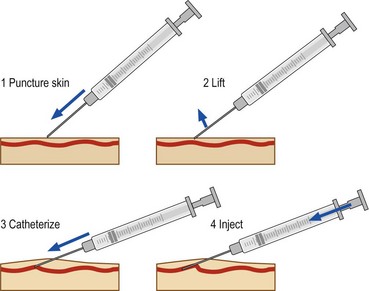
Injection with the bevel of the needle up has the advantage of minimizing the chance of transecting the vessel. Inserting the needle bevel down may be easier, probably as the result of the vacuum produced by the bevel on the skin surface. An alternate technique is to puncture the skin very superficially, to hook it, to lift it a little in order to bring the vessel in the same axis as the needle and then to cannulate it (Fig. 12.11).
Air-bolus (block) or foam technique
The air-bolus technique – injecting a small amount of air to clear the vessel before instilling the sclerosing solution – is recommended by multiple physicians.4,5,19 It is thought to minimize the risk of inadvertent intradermal injection. This, however, may not occur, since once the vessel is cleared of blood, it is more difficult to see the progress of the sclerosing solution within its lumen. Therefore, others, including ourselves, have abandoned this technique.21,23 Another theoretical advantage of the air-bolus technique is the decreased risk of intravascular thrombosis. It is thought that if the vessel is cleared of blood by first injecting air, the risk of extravasation of RBCs may also be minimized. However, antegrade and retrograde filling of the treated vessel occurs after the injection. Thus, the air-bolus technique may not prevent or lessen the incidence of post-treatment pigmentation. It is necessary to stress the risk of visual disturbances when using the air-block technique.25,26
Foam injection
Another variant of the air-bolus technique that helps visualize clearing of the vessels is that of creating a foamy solution before injection. This can be achieved with the use of any ‘detergent’ class of sclerosing solution such as STS or POL (see Chapter 7). Green and Morgan27 added Haemacel to STS to accentuate bubble formation. It is also thought that the foam causes the sclerosing agent to interact more efficiently with the endothelium (see Chapters 7 and 9). We have found that foaming a detergent solution increases its potency at least twofold while decreasing its caustic toxicity fourfold when a solution-to-air ratio of 1 : 4 is used. Therefore, the use of foam in treating telangiectasia less than 1 mm in diameter is tricky. Until a method is devised to standardize the size and stability of foam, the physician cannot accurately predict the foam’s sclerosing strength. We reserve the use of foam for treating reticular and varicose veins.
To create foam, a small amount of a detergent solution can be drawn into a glass syringe. While the open end of the syringe is almost totally closed, the plunger is pulled back, allowing the introduction of air through the sides of the plunger and syringe. This technique produces foam of fair quality that degrades 50% over 1 to 2 minutes.28 Silicone is present in syringes in order to lubricate the barrel, making for easier compression on the plunger. We have found that the foam half-life varies over 50% for different syringes.29 Some phlebologists recommend using glass syringes to avoid this variability in foam half-life. The glass syringe method necessitates appropriate sterilization of the syringe between patients.
Other methods for producing long-lasting reproducible bubble diameter foam are under development and evaluation. Sclerosing foams can be made by adding air to the liquid solution or with a tensioactive agent and CO2, according to Cabrera et al.30,31
The main difference between sclerotherapy with a solution and with foam is the longer duration of foam within the vein and the concentration of the damaging nonpolar end of the detergent molecule on the endothelial surface. This promotes sclerosis of the treated vessel with a lower concentration of sclerosing solution. Several methods for preparation of simple sclerotherapy foam have been proposed by Monfreux,32 Benigni et al,33 Mingo-Garcia,34 Tessari,35 and Frullini.36 Tessari’s method makes foam with a three-way tap and two syringes.
Hennet37 used 3-mL glass syringes into which 0.3 to 0.4 mL of POL is made up as a 0.5% solution and then diluted with 0.1 to 0.2 mL of physiologic serum. The foam is stated to last for approximately 1 minute with this technique. The syringe is withdrawn until 0.6 to 1.3 mL of foam fills the syringe. The foam, as it is injected, prevents the secondary back-bleeding and is therefore in contact with the vessel wall. Hennet reported treating 10,262 patients with over 70,000 injections between November 1995 and September 1998. Less than 0.5 mL of foam was given in each injection, and compression was not used. He reported excellent results without significant adverse sequelae.
With Frullini’s method, the foam is simply produced in a disposable vial with the air contained in the vial or, preferably, with prior withdrawal of most of the sclerosing solution. A small connector is inserted into the vial, and simply pulling and pushing the liquid produces the foam (Figs 12.12 and 12.13). The key point is to generate a turbulence that produces the foam. Foam can be produced even without the connector by directly fitting the cone of the syringe into the rubber of the cap of the vial. However, the connector makes the maneuver easier and permits reuse of the system on the same patient in order to reproduce the foam for a second injection.

Figure 12.12 Syringe inserted into a vial containing approximately 0.2 mL of sodium tetradecyl sulfate 3%.
(From Frullini A: Dermatol Surg 26:705, 2000.)

Figure 12.13 Foam produced by rapid movement of the plunger in and out of the vial is stable for 5–10 min.
(From Frullini A: Dermatol Surg 26:705, 2000.)
Benigni and Sadoun38 compared the efficacy and adverse-effect profile of 0.25% POL foam with 0.25% POL liquid in treating telangiectasia. They reported a 20% improvement in efficacy with foam versus liquid, without an increase in adverse effects. This is contrary to Weiss,39 who found an increased incidence of pigmentation and TM when 0.1 or 0.2% STS foam was used as compared with liquid STS. Forty percent of patients treated with STS 0.1 or 0.2% foam into telangiectasia of less than 1 mm had 76% to 100% improvement and 82% had greater than 50% improvement. The incidence of pigmentation and TM increased to 20% each if a second treatment was required. Kern40 has shown that more pigmentation occurs with foam, and we have demonstrated41 that more side effects were observed with foam. Finally, and following the conclusion of the European consensus,42 we do not recommend the use of foam as primary treatment of telangiectatic veins.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree