The incidence of melanoma is rising worldwide, and in the United States has increased by approximately 2.8% annually since 1981. Melanoma is more common in whites, and is generally more prevalent in men. However, there is a 6.1% annual increase in US incidence of melanomas in white women younger than age 44, with growing concern that increases in skin cancer in younger women may reflect recent trends in indoor tanning. Melanoma incidence is also greater in higher economic groups. Globally, melanoma incidence is highest in Australia, followed by the United States and parts of Europe.
- •
Melanoma incidence has been increasing since data collection began in the United States in the 1970s.
- •
There is an increase in melanoma incidence in young women, and there is concern that this may reflect recent trends in indoor tanning.
- •
Melanoma incidence is highest in higher socioeconomic groups, but when it occurs in lower socioeconomic groups it is usually diagnosed at a later stage.
US trends in melanoma incidence over time
Melanoma incidence has been on the rise in the United States for several decades as tracked by the US Surveillance, Epidemiology, and End Results (SEER) program ( Fig. 1 ). The SEER program, which is supported through the National Cancer Institute, provides cancer surveillance in the United States through registries representative of the US population. Data collection began in 1973 and it has grown from the original nine locations to include more than 17 registries and 28% of the US population. Melanoma age-adjusted incidence in 2008 (the most recent SEER data available) in the United States has reached 22.5 per 100,000 (2000 US population). Melanoma incidence has been increasing steadily by roughly 2.8% annually from 1981 to 2008. According to a recently published study, which includes SEER and National Program of Cancer Registries data, the national rate of melanoma was 19.2 per 100,000 from 2004 to 2006. Combining the two databases during that time period covers 77.6% of the US population.
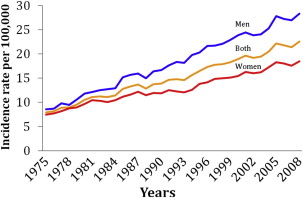
Gender
The incidence and the mortality of melanoma are generally greater in men than women. In 2008, the incidence of melanoma in all males was 29.1 per 100,000 compared with 19 per 100,000 in women. In 2008, age-adjusted incidence for men remains higher than for women at 28.3 and 18.5 cases per 100,000, respectively. The percent increase from 1986 to 2008 in men is 3% (delay-adjusted), and is 2.4% annually for women between 1980 and 2008.
Similarly, the annual percent increase in melanoma for all ages is greater in men than women, 6.1% compared with 2.8%. However, there is growing concern about a shift toward higher incidence in young women. Younger than age 44 the incidence for women is 8.2 per 100,000, whereas for men it is 5.3 per 100,000. This higher incidence of melanoma in young women compared with young men is generally an increase in thin lesions. There is growing concern that increases in skin cancer in younger women may reflect recent trends in indoor tanning.
The most common location for melanoma in men is on the trunk, followed by the upper extremities. In women, the lower extremities are the most common location for melanoma.
Race and Ethnicity
Melanoma most commonly affects whites, but it also occurs in other races. From 2004 to 2008 the age-adjusted rates in Hispanic, black, Asian/Pacific Islander (API), and American Indian/Alaska Native (AI/AN) were 3.9, 1, 1.4, and 3.7 per 100,000, respectively ( Fig. 2 ). This is in comparison with non-Hispanic whites, in whom the incidence is 28.7 per 100,000. The lower incidence of melanoma in darker-skinned individuals is attributed to the protective effects of higher melanin densities.
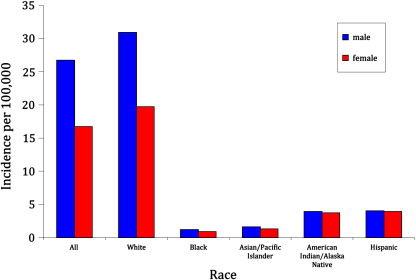
In Hispanics, AI/AN, and APIs, a greater percentage of melanomas occurred in younger age groups (24.4%, 22.9%, and 20.8% less than 40 years old, respectfully) compared with blacks and whites (15.8% and 14.3% younger than 40 years old). Most cases in blacks, API, and Hispanics were female, compared with whites, in which men were more likely to develop melanoma. In blacks, acral lentiginous was the most common subtype, whereas superficial spreading was the most common in all other racial groups. The rates of melanoma rise with increasing age in all groups. Nonwhite groups were more likely to be diagnosed with distant melanomas. Only 4% of melanomas in whites are distant at diagnosis, whereas anywhere between 7% and 13% of other ethnic groups have advanced melanomas at diagnosis.
Tumor Characteristics
In the United States from 1992 to 2004, in non-Hispanic whites 37.5% were superficial spreading melanoma, 7.4% were nodular melanoma, 7.3% were lentigo maligna, 0.9% were acral lentiginous melanoma, and 4.4% were other subtypes. There were no significant differences in the proportions of the histologic subtypes over the time interval. Similar proportions are reported from 2004 to 2006 as 28.8% superficial spreading, 6.9% nodular, 6% lentigo maligna, and 1% acral lentiginous, although 57.2% were reported as melanoma not-otherwise-specified. Of the subcategories of melanoma not-otherwise-specified, 1.2% were desmoplastic melanoma and 0.4% were amelanotic melanoma.
In non-Hispanic whites aged 0 to 85 and older from 1992 to 2004, there were increases in all groups of tumor thickness. For tumors less than or equal to 1 mm there was a 4.8% increase for men and 4.7% for women, and for tumors greater than or equal to 4.01 mm a 4.1% increase for men and 3.3% increase for women. The annual percent change in incidence rates for tumor thickness were even greater in the subgroup older than age 65. In a similar analysis of SEER data from 1992 to 2006, there were increases in melanoma incidence in men of all tumor thickness for those aged 65 and older. In younger men, only thin tumors increased in incidence. Similarly, among women, tumors of all depth increased in incidence over the time interval, except tumors greater than 2 mm in women aged 40 to 64 and tumors 2.01 to 4 mm deep in women younger than 40 years old. In men and women older than 65 years, there was almost a twofold increase in the rates of thick tumors compared with thin tumors.
International
Melanoma incidence is significant outside of the United States. Australia has the largest incidence of melanoma, with incidence rates roughly twice that of the United States. The Australian Institute of Health and Welfare has been collecting statistics about melanoma incidence in Australia since 1982, and these are available through 2007. In 2007, there were 10,342 melanomas, an incidence of 46.7 per 100,000 people (age-standardized to 2001 Australian population). For Australians, there is a 1 in 28 risk of developing melanoma by the age of 75. The average annual change in incidence rates for melanoma of the skin in Australia from 1982 to 2007 is 2.3%, comparable with US changes.
In Europe, incidence has not reached the same magnitude as the United States and Australia. In the United Kingdom the incidence from 1998 to 2002 for men ranges from 6.9 to 10.7 age-standardized rate per 100,000 and 7.1 to 12.6 per 100,000 for females. In males, the incidence is the greatest in Germany, Norway, and Switzerland, with age-standardized rates of 12.7, 14.2, and 18.6 per 100,000, respectively. In females, Denmark, Norway, Iceland, and Switzerland have the highest age-standardized rates at 14.1, 14.6, 19, and 19.6 per 100,000, respectively. In general, melanoma incidence rates in whites decrease with distance from the equator. However, in Western Europe, the inverse pattern is observed, with greatest incidence in the North. This has been postulated to be because lighter-skinned northern Europeans travel to southern Europe where they receive intense, intermittent sun exposure.
Risk Factors
Established risk factors for melanoma are genetic and phenotypic traits, risk behaviors, and environmental factors. Genetic and phenotypic predisposition can be further specified as increasing age, fair skin and hair color, greater than 20 nevi, freckling, greater than or equal to three atypical nevi, greater likelihood of burning with sun exposure, immunosuppression, previous psoralen UV-A treatment, solar keratoses, squamous cell carcinoma, xeroderma pigmentosum, and family history of dysplastic nevi or melanoma. Environmental exposure is important in melanoma with attention being given to history of greater or equal to three episodes of sunburn; periodic excessive sunlight exposure (vacations with intense exposure); possibly long-term continuous sunlight exposure; and UV exposure at tanning salons. Other environmental factors, such as ozone depletion and latitudes closer to the equator, may also relate.
Sociodemographic factors in melanoma incidence
Income
Over the past several years it has come to light that melanoma is generally more common in those of higher economic class. Reyes-Ortiz and colleagues performed a review of 25 studies in the United States and other countries examining socioeconomic status (SES) and melanoma incidence. In all except two, there was a positive association between higher SES and increased melanoma incidence. This effect was greatest in men of higher SES. The authors proposed several possible explanations. The first is biologic susceptibility. Patients that have melanomas and increased SES are likely to have phenotypic risk factors, including fair skin and hair color, increased likelihood to burn instead of tan, increased freckling, and a large number of atypical melanocytic nevi.
The second is increased UV exposure. High SES groups have greater leisure time and more opportunity for periodic excessive sunlight exposure. In the Norwegian Women and Cancer Study, the average number of sunburns yearly increased by level of education, which likely represents greater travel to southern climates, common in middle and high SES in Norway. Similarly, people living in larger towns in Sweden (higher incidence of melanoma) have increased frequency of foreign travel, detected by increased passport use.
Although melanoma incidence parallels SES, a recent US study suggested that all SES groups may actually have increasing incidences of melanoma. According to Linos and colleagues, California patients living in areas of highest SES were at higher absolute risk of all melanomas. However, patients living in low SES areas experienced the greatest increases in incidence, and the greatest increases in incidence were among the thickest tumors (2.01–4 and ≥4 mm). Similarly, Greenlee and Howe demonstrated that living at higher poverty levels increased the odds of late-stage melanoma by twofold.
A similar relationship between SES and melanoma incidence has been reported in Europe. In Denmark, Birch-Johansen and colleagues evaluated all 3.22 million Danish residents born between 1925 and 1973 without a previous history of cancer. Socioeconomic, demographic, and health-related indicators were obtained from Danish registers. Melanomas diagnosed from 1994 to 2003 were associated with the highest disposable income, an incidence rate ratio (IRR) of 1.4 (confidence interval [CI], 1.3–1.5); higher education, with an IRR of 1.7 (CI, 1.6–1.9); and unemployment was negatively associated, with an IRR of 0.8 (CI, 0.7–0.9).
Similar results have been found in England, where the most deprived had a relative risk of 0.5. Shack and colleagues assigned a socioeconomic group based on their address at the time of diagnosis, using the income domain of the Index of Multiple Deprivation.
Similar findings have been reported by Goodman and colleagues, who showed there is a lower incidence of melanoma in outdoor workers. Among indoor occupations, funeral director/embalmers and dentists had the highest incidence (odds ratio, 5.3 [CI, 2.1–13.6] and 3.1 [CI, 1.9–5.1], respectively).
Education
In 1999, the National Cancer Institute initiated the SEER-National Longitudinal Mortality Study, which connects the SEER registry to self-reported, detailed demographic and socioeconomic data from the Census Bureau’s Current Population Survey. Of the categories of education, family income, poverty status, and place of residence, only education and income were significant for differences in incidence of melanoma. Those with less than a high school education had a relative risk of 0.55 (CI, 0.37–0.82), signifying a lower risk of melanoma in the less-educated population. Similarly, those with a family income less than $12,500 had a relative risk of 0.59 (CI, 0.36–0.95).
In Iceland, the population is small and ethnically similar and has been postulated to have high social equity. However, there are still differences in SES, and education has been found to be the most reliable measure of social status in Iceland. Vidarsdottir and colleagues conducted a study linking the Icelandic Cancer Registry and information on education from the 1981 census. Higher educational level was associated with an increased risk of melanoma. The least educated had a standardized incidence ratio of 0.60 (CI, 0.36–0.85), and the standardized incidence ratio was 147% higher in the highest-educated group.
The effect of education on melanoma incidence was also reported in the United States. Harrison and colleagues compared SEER melanoma incidence statistics from 1973 to 1993 with SES information from the 1950, 1960, 1970, 1980, and 1990 census data. The percentage of high school graduates over time was significantly associated with an increase in melanoma incidence, which was not mediated by income, age, or gender.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree